Abstract
Background
US Black women have higher breast cancer mortality rates than White women despite lower incidence. The aim of this study is to investigate how much of the mortality disparity can be attributed to racial differences in natural history, uptake of mammography screening and use of adjuvant therapy.
Methods
Two simulation models use common national race- and age-specific data for incidence, screening and treatment dissemination, stage distributions, survival and competing mortality from 1975 to 2010. Treatment effectiveness and mammography sensitivity are assumed to be the same for both races. We sequentially substituted Black parameters into the White model to identify parameters that drive the higher mortality for Black women in the current time period.
Results
Both models accurately reproduced observed breast cancer incidence, stage and tumor size distributions and breast cancer mortality for White women. The higher mortality for Black women could be attributed to differences in natural history parameters (26–44%), use of adjuvant therapy (11–19%) and uptake of mammography screening (7–8%), leaving 38–46% unexplained.
Conclusion
Black women appear to have benefited less from cancer control advances than White women, with a greater race-related gap in the use of adjuvant therapy than screening. However, a greater portion of the disparity in mortality appears to be due to differences in natural history and undetermined factors.
Impact
Breast cancer mortality may be reduced substantially by ensuring that Black women receive equal adjuvant treatment and screening as White women. More research on racial variation in breast cancer biology and treatment utilization is needed.
Keywords: breast neoplasms, mammography, adjuvant therapy, mortality, healthcare disparities, continental population groups, computer simulation
INTRODUCTION
In 2009, an estimated 192,370 women in the United States (US) were diagnosed with invasive breast cancer and approximately 40,170 women were expected to die of this disease.(1) After remaining relatively constant for many years, breast cancer mortality in the US decreased by 24% from 1990 to 2000 because of diffusion of mammography screening and improved adjuvant breast cancer treatment.(2) However, trends show a growing disparity in breast cancer mortality between Black and White women. While the breast cancer mortality rates for White women steadily decreased from 1990 onward at an average annual rate of 2.4%, the rates in Black women have only decreased by 1.1% per year during this same period.(3) The higher mortality rate for Black women (i.e., in 2006 49 per 100,000 vs. 35 per 100,000 for White women age 25 and over) is particularly striking since breast cancer incidence is lower for Black than White women.(3)
Several factors are thought to contribute to the observed race disparity in breast cancer mortality. Black women are more likely to present with breast cancer at a later stage than White women.(4–6) This difference has been hypothesized to be due to low or irregular rates of use of mammography screening,(7) delays in follow-up after an abnormal mammogram,(8) and/or cultural beliefs and attitudes that may lead to delayed presentation of clinically diagnosed cases.(9) Even within stage categories, Black women have significantly worse survival than White women after controlling for age and tumor markers.(10) This racial difference in stage-specific survival has been hypothesized to be due to underuse of appropriate adjuvant therapy(11) and delays in treatment initiation.(12–13) Also, higher rates of co-morbidities, including cardiovascular disease and diabetes may affect Black women’s ability to tolerate chemotherapy and lead to dose reductions that diminish treatment effectiveness.(14) In addition, differences in tumor biology, such as higher rates of poor-prognosis triple-negative tumors in Blacks have been hypothesized to contribute to the Black-White disparities in breast cancer mortality.(15–16)
In the present study, the impact of natural history, screening use and adjuvant therapy use on the disparity in breast cancer mortality between US Black and White women is estimated using two established, independent population simulation models.(17–18) Modeling provides an excellent “laboratory” for the evaluation of the separate contribution of these factors, because hypothetical scenarios can be simulated (e.g. changing one factor at a time). Our results are intended to inform health policy debates about the most effective strategies to reduce the disparity in breast cancer mortality between Black and White women and ultimately reduce the burden of breast cancer for all Americans.
METHODS
Model Overviews
MISCAN-Fadia (MIcrosimulation of SCreening ANalysis-Fatal diameter) and SPECTRUM (Simulating Population Effects of Cancer Control inTerventions – Race and Understanding Mortality) are two simulation models developed within the Cancer Intervention and Surveillance Modeling Network (CISNET). CISNET is an international collaborative modeling effort funded by the National Cancer Institute (NCI). Collaborative modeling provides an opportunity to evaluate how model differences affect results.
The models have been described in detail elsewhere(17–18) and information about the models can be found online.(19) Briefly, both models simulate breast cancer trends in the US population in the absence of screening or adjuvant treatment and then overlay screening and adjuvant treatment diffusion over time. MISCAN-Fadia models tumor growth, where tumors can be detected once they are beyond a detection threshold and cured if the tumor diameter is below a fatal diameter. In SPECTRUM, tumors progress through stages, with screening effects due to age and stage shifts and adjuvant treatment reducing the hazard of death. In both models ductal carcinoma in situ (DCIS) is represented as a state that can regress, remain and be diagnosed or progress to invasive cancer.
Model parameters
Race-Specific Common Data Inputs
MISCAN-Fadia and SPECTRUM use a common race-specific set of data inputs to model breast cancer mortality by race. The demographic characteristics of multiple birth cohorts of Black and White women born between 1890 and 1985 were based on historical data for number of births and deaths from the US Census and the National Center for Health Statistics (NCHS).(20)
The background incidence of breast cancer in the absence of screening was estimated from the Connecticut Tumor Registry and Surveillance, Epidemiology and End Results (SEER) data with the use of an age-period-cohort (APC) model.(21) The original APC model was used for White women and adapted for Black women using an age-specific relative risk of Black vs. White incidence.
SEER data for stage distribution and breast cancer specific survival from the period 1975–1979 were used to model the natural history of breast cancer in the absence of mammography screening and adjuvant therapy since these cancer control interventions did not begin to disseminate into the population in a substantial manner until after 1980.
The dissemination of mammography in the population was estimated using a two-part model described elsewhere (22–23). The first component of the model involves estimating the distribution of age at first mammography and the second component estimates the interval between successive screenings. For both components a race-specific variant has been used resulting in somewhat lower screening rates for Black women .(24) For example, the screening rates were approximately 13% lower in Black than White women age 50–74 year in the period 1995–2005.
Age-, year-, AJCC stage-, estrogen receptor (ER), and human epidermal growth factor receptor 2 (HER2)-specific use of adjuvant therapy among Black and White women from 1975 to 2000 was estimated from data from the NCI’s Patterns of Care (POC) studies(25–26) and updated through 2010 based on data from patients presenting at National Comprehensive Cancer Network (NCCN) sites. Overall, Black women were 22% and 15% less likely to receive multi-agent chemotherapy and hormonal therapy, respectively than White women. These Black-White differences were applied to the adjuvant treatment dissemination curves from 1975 to 2010.
Non-Race Specific Inputs
Treatment effectiveness estimates are based on meta-analyses of randomized trial results from the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG).(27–29) We assume that hormonal and chemotherapy regimens are equally effective in Black and White women.(30)
The sensitivity of mammography screening is based on data from screening trials and Breast Cancer Surveillance Consortium (BCSC), and is assumed to be equal for both race groups.‡
Model Validation
SPECTRUM and MISCAN-Fadia have used several approaches to assess the internal reliability of the models and the validity of the results against external data for the US population.(17–18) For the present study, we compared model predictions for incidence rates by race over time (1975–2006) with SEER data.(31) Breast cancer incidence by race for women 25 years and older was directly age-standardized to the standard US 2000 population. We also compared model predictions of the stage (SPECTRUM) and tumor size (MISCAN-Fadia) distribution by race (assuming observed race-specific dissemination of screening) with observed SEER data in the period 2004–2006 (the last year of publically available SEER data at the time of analysis).
Impact of Screening and Adjuvant Therapy on Breast Cancer Mortality
The models were used to estimate age-adjusted breast cancer mortality rates between 1975 and 2010 for Black and White women in the US. We calculated percent mortality reductions by comparing the mortality in scenarios with screening, adjuvant treatment, and both with the background mortality predicted in the absence of screening and adjuvant treatment. Breast cancer mortality by race for women 25 years and older was directly age-standardized to the standard US 2000 population. The predicted breast cancer mortality rates were compared to the observed rates for Black women for the period 2004–2006.(32)
Factors Contributing to the Observed Mortality Difference
We investigated the effect of the following factors on the difference between White and Black women in age-adjusted breast cancer mortality in a current period (the years 2004–2006): demography and breast cancer incidence, natural history (defined as the stage distribution and survival in the absence of screening and adjuvant treatment, and ER/HER2 distribution), screening use, and adjuvant treatment use. To this end, we sequentially substituted parameter values relating to these factors in the White version of each of the two models by corresponding values from the Black version and computed the fraction of the mortality difference between White and Black women explained by each factor.
RESULTS
Model Validation
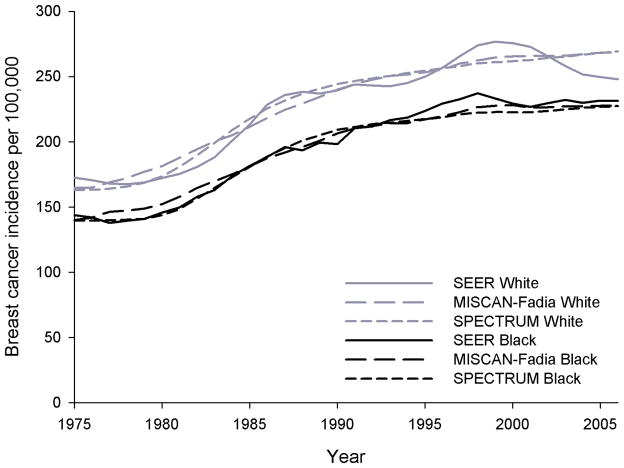
From 1975 to 2006 the observed age-adjusted breast cancer incidence rates steadily rose from 173 to 249 per 100,000 in White women and from 144 to 227 per 100,000 in Black women. These trends were accurately reproduced by both models for both races (Figure 1). The difference between the observed and predicted incidence was not more than 10% in either model in any year.
Figure 1.
Age-adjusted incidence rates (3 year moving average) over time as observed (SEER) and predicted by MISCAN-Fadia and SPECTRUM for White and Black US women ages 25 years and older
The observed stage distribution at diagnosis for the period 2004–2006 was more favorable in White than in Black women (Figure 2). This observation was reproduced by both models, with a more favorable tumor size distribution (MISCAN-Fadia) and stage distribution (SPECTRUM) for White than for Black women (Figures 2a and 2b). However, for Black women, both models predicted a slightly more favorable stage or tumor size than actually observed.
Figure 2.
Figure 2a. Age-adjusted tumor size distribution of invasive breast cancers for White and Black US women age 25 years and older as observed and predicted by MISCAN-Fadia in 2004–2006
Figure 2b. Age-adjusted stage distribution for White and Black US women age 25 years and older as observed and predicted by SPECTRUM in 2004–2006
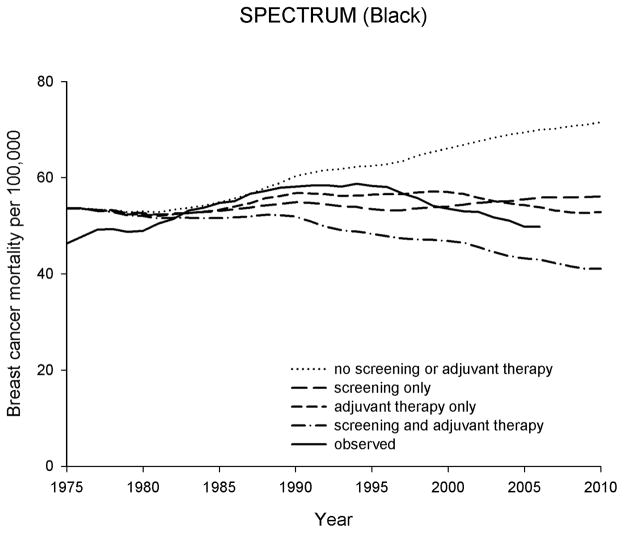
Impact of Screening and Adjuvant Therapy on Breast Cancer Mortality
There have been different trends of age-adjusted breast cancer mortality observed over time (1975–2006) by race (Figure 3A (MISCAN-Fadia) and Figure 3B (SPECTRUM) for White and Figure 4A (MISCAN-Fadia) and Figure 4B (SPECTRUM) for Black women).
Figure 3.
Age-adjusted breast cancer mortality rates (3-year moving averages) over time as observed and predicted in four scenarios for White women age 25 years and older
panel A. MISCAN-Fadia
panel B. SPECTRUM
Figure 4.
Age-adjusted breast cancer mortality rates (3-year moving averages) over time as observed and predicted in four scenarios for Black women age 25 years and older
panel A. MISCAN-Fadia
panel B. SPECTRUM
For White women, the model predicted breast cancer mortality rates with screening and adjuvant treatment as disseminated in the population were similar to the observed rates. The difference between the observed and predicted rates was less than 8% for all years between 1975 and 2006 in both models. Both mammography screening (19–22% mortality reduction for MISCAN-Fadia and SPECTRUM, respectively) and adjuvant treatment (27–31% mortality reduction) contributed substantially to the observed reduction in breast cancer mortality among White women in both models (Table 1). The combination of mammography and adjuvant therapy is estimated to have resulted in substantially lower breast cancer mortality among White women in 2004–2006 (41–44% reduction) compared to a hypothetical situation without screening and adjuvant treatment.
Table 1.
Model predicted age-adjusted breast cancer mortality rates in 2004–2006 per 100,000 US women ages 25 years and older
| Scenarios | WHITE | BLACK | ||||||
|---|---|---|---|---|---|---|---|---|
| MISCAN-Fadia | SPECTRUM | MISCAN-Fadia | SPECTRUM | |||||
| Mortality rate per 100,000 | Mortality reduction (%) * | Mortality rate per 100,000 | Mortality reduction (%) * | Mortality rate per 100,000 | Mortality reduction (%) * | Mortality rate per 100,000 | Mortality reduction (%) * | |
| No screening or adjuvant therapy | 67.0 | - | 64.0 | - | 68.2 | - | 69.5 | - |
| Screening only (as disseminated in the population) | 54.6 | 18.6% | 49.9 | 22.0% | 55.9 | 18.1% | 55.5 | 20.1% |
| Adjuvant therapy only (as disseminated in the population) | 46.3 | 30.9% | 46.4 | 27.5% | 51.7 | 24.2% | 54.3 | 21.9% |
| Screening and adjuvant therapy (as disseminated in the population) | 37.5 | 44.0% | 37.4 | 41.4% | 41.9 | 38.6% | 43.2 | 37.8% |
| Observed mortality rate | 36.1 | 49.8 | ||||||
Mortality reductions (%) are calculated by comparing the predicted mortality to the background mortality in the scenario without screening and adjuvant therapy
For Black women, the model predicted breast cancer mortality rates with screening and adjuvant treatment as disseminated in the population diverge from the observed rate. The observed breast cancer mortality decreases less and later than the predicted rates. The predicted mortality reductions in both models were somewhat lower than for White women: mammography screening (18–20% mortality reduction), adjuvant treatment (22–24% mortality reduction), and the combination of screening and treatment (38–39% mortality reduction) (Table 1).
Factors Contributing to the Observed Mortality Difference
Table 2 compares observed age-adjusted breast cancer mortality in 2004–2006 among White women (36.1 per 100,000 women-years) and Black women (49.8 per 100,000) to predictions from a series of models with White parameter values sequentially replaced by Black values. The models for the White population predict mortality correctly (37.4 and 37.5 per 100,000 respectively, in MISCAN-Fadia and SPECTRUM). First, replacing demographic characteristics and breast cancer incidence lowered mortality predictions to 32.5 and 32.2 per 100,000, as a result of the lower incidence for Black women. Next, changing natural history parameters responsible for a less favorable stage distribution and survival in Black women raised predicted mortality to 36.9 and 40.1 per 100,000. The lower rate of screening among Black women raised mortality to 38.4 and 41.3 and the lower use of adjuvant therapy raised mortality to 40.3 and 42.0 per 100,000. Changing all parameters to Black values resulted in mortality predictions of 41.9 and 43.2 per 100,000 in MISCAN-Fadia and SPECTRUM, respectively. Of the difference between observed mortality and predicted mortality after taking into account the lower incidence among Blacks, natural history explained 26% (44%), screening use 8% (7%), and use of adjuvant therapy 19% (11%), leaving 46% (38%) unexplained in MISCAN-Fadia (SPECTRUM).
Table 2.
The effect of sequential replacement of parameters for Black women in the White model on the predicted breast cancer mortality rate for Black women age 25 years and older for the period 2004–2006
| White value replaced with Black value (in bold) | ||||||||
|---|---|---|---|---|---|---|---|---|
| observed (White) | none (White model) | demography and incidence | demography, incidence, and natural history | demography, incidence, natural history, and screening | demography, incidence, natural history, and treatment | all (Black model) | observed (Black) | |
| MISCAN-Fadia | ||||||||
| Mortality per 100,000 | 36.1 | 37.5 | 32.5 | 36.9 | 38.4 | 40.3 | 41.9 | 49.8 |
| Difference, (obs-pred) | 17.4 | 12.9 | 11.5 | 9.6 | 8.0 | |||
| % explained by replaced value1 | 26% | 8% | 19% | 54% | ||||
| SPECTRUM | ||||||||
| Mortality per 100,000 | 36.1 | 37.4 | 32.2 | 40.1 | 41.3 | 42.0 | 43.2 | 49.8 |
| Difference, (obs-pred) | 17.6 | 9.8 | 8.5 | 7.8 | 6.6 | |||
| % explained by replaced value1 | 44% | 7% | 11% | 62% | ||||
calculated as the ratio of reduction of the difference between observed and predicted mortality rate and the difference between observed and predicted mortality, taken into account the lower incidence among Black women. So, in MISCAN-Fadia substituting Black natural history parameters into the White model explains 26% of the Black-White differences based on a reduction in the difference from 17.4 to 12.9 per 100,000, or 4.5 of the 17.4 per 100,000, i.e. 26%.
obs = observed; pred = predicted
DISCUSSION
To our knowledge, this is the first study using collaborative population modeling to evaluate the separate and combined impact of natural history, screening use and adjuvant therapy use on race disparities in breast cancer mortality in the US. Both models find that the majority of the Black-White disparity in mortality outcomes is attributable to variations in natural history and yet unknown factors, and to a lesser extent to differences in use of cancer screening or treatment services. In addition, the results suggest that racial differences in adjuvant treatment dissemination contribute to the racial disparity in breast cancer mortality to a greater extent than differences in screening uptake.
Our results indicate that breast cancer natural history parameters were a major driver of race-specific differences in mortality. Also, reduced screening and treatment use in Black women, which might be related to the higher proportion of un(der)insured Black women,(33) contributed to the mortality disparity. However, the models also agree that a substantial part (38–46%) of the mortality difference by race remains unexplained, which is in line with previous work showing that several predictor variables contribute to, but do not fully explain, race differences in breast cancer survival.(34)
Several factors might account for the unexplained part of the mortality difference. First, our assumptions about some inputs being equal for Blacks and Whites might be too optimistic for Black women (e.g., equal sensitivity of screening by race). Although the predicted incidence and stage distribution for Black women fit the observed data reasonably well, both models predict a slightly more favorable stage or tumor size distribution than observed for the period 2004–2006. This might indicate a somewhat reduced sensitivity of mammography screening for Black women, perhaps due to lower quality imaging or interpretation. In addition, the time interval between mammogram and follow-up might differ by race. For example, women who experienced a delay between the time of mammogram and diagnosis or last diagnostic test ruling out cancer were found to be more likely to be Black than White (odds ratio 1.45; 95% confidence interval = 1.13, 1.85).(35)
Also, as observed in several randomized clinical trials, treatment efficacy was assumed to be equal for Blacks and Whites in our models.(30) However, the higher prevalence of co-morbidities for Black women might lead to dose reductions outside clinical trials, resulting in somewhat reduced treatment effectiveness in community practice. Also, Black women have been found to be less likely than white women to be treated at high-quality hospitals(36) and experience more delays between diagnosis and the beginning of treatment.(37) In addition, Black women have been found to be more likely than White women to have no surgery,(34) to discontinue treatment before completion of all courses (11% vs. 7%, respectively; P = .07)(38) and more likely to miss appointments (19% vs. 9%, respectively; P=.0002).(38) Those factors are not captured in our models, because high-quality data on the frequency of occurrence and effect on breast-cancer survival by race, age, stage, and calendar year were not available in this level of detail.
While we modeled racial differences in the distribution of known tumor prognostic markers (ER and HER2), an alternative explanation for our inability to explain the full mortality disparity is that Black women have experienced an increasing amount of aggressive tumor types over time based on less clearly defined prognostic markers. This might, for example, be related to racial differences in the prevalence of obesity in the US, which have been increasing over the past three decades, with the most pronounced increases among Black women.(39) Obesity affects breast cancer mortality rates in several ways.(40) First, obesity may decrease treatment efficacy, because lower doses are delivered relative to what is recommended based on body surface area.(41) In addition, obesity may influence breast cancer survival(42), mammography use,(43) screening performance,(44) and mammography follow-up (e.g. a higher frequency of obese women delayed return for mammography resolution compared with non-obese women (64.7% vs. 35.3%))(45). Including obesity directly in our models would help to partition the effect of race and obesity on the disparity in breast cancer mortality. More research on the race-specific types of tumor diagnosed over time will be critical to developing the knowledge base needed to refine the natural history components of our, and other, population surveillance models.
Both models indicate that both mammography screening and adjuvant treatment contributed substantially to the observed reduction in breast cancer mortality over the past several decades for both Black and White women. This result is consistent with conclusions from past modeling work for the overall US female population.(2) The predicted mortality reductions from the present study are somewhat larger than reported in past studies, probably due to greater penetration of screening in recent years and our inclusion of newer treatments (e.g., traztuzumab and aromatase inhibitors). Also, the percent mortality reductions depend somewhat on what age range is evaluated. For example, the percentages due to screening will be somewhat larger when a smaller age range excluding women unlikely to benefit from screening (age 25–40 year) is evaluated. For Black women, the predicted percent mortality reductions were somewhat lower than for White women, in particular the mortality reduction attributed to adjuvant treatment.
Our finding that treatment variations accounted for a greater amount of race variation in mortality than screening is consistent with previous research. For instance, an earlier modeling study showed that efforts to ensure that Black women receive the same treatment as White women was a more cost-effective approach to reducing their disproportionate mortality than investing in increased screening use.(46) The finding that the effect of reduced screening use was relatively small (7–8%) is also consistent with previous work showing that the difference in screening rates between Black and White women is not very large.(47) Previous work showed that differences in mammography use can explain 10–12 % of excess late-stage breast cancer among Black women compared with White women.(48–49)
The collaboration of two groups with different model assumptions and structure provides an excellent opportunity to cross-replicate modeling results, quantify uncertainty, and indicate which results are consistent across modeling approaches and therefore less dependent on unverifiable model assumptions. The resulting conclusions about race-specific differences in the impact of natural history, screening and adjuvant treatment on breast cancer mortality rates were similar across the two models and should provide greater credibility than inferences based on one model alone.
The most important limitation of the current study is the relative paucity of data on Black women, especially for the use of adjuvant treatment. Several studies that assessed the use of treatment by Black women in comprehensive cancer centers found no difference in treatment between races.(50) However, data on treatment use in the population over time are sparse for Black women. In addition, the data that are available for Black women might suffer from selection bias, with Black women who participate in trials potentially not being representative of the overall Black population. In addition, although we used the best quality data available for Black and White women as input parameters for the models, this approach led to the use of several different data sources for different variables, with the potential problem of one (or more) of these data sources not being representative of the total Black (female) population. Next, while we portrayed known differences in biology by race and age (e.g., distribution of ER and HER2 positive tumors), some aspects of the race-specific natural history of disease are not known and/or cannot be fully captured. Even with these acknowledged limitations, the two models demonstrate meaningful, qualitatively similar outcomes despite variations in structure and assumptions.
The findings of the current study have important policy implications. Our results indicate that breast cancer mortality may be reduced substantially by ensuring that Black women receive adjuvant treatment and mammography screening equal in quantity and quality to that which White women receive. However, a considerable portion of the observed race differences in mortality remains unexplained. More research on racial variation in breast cancer biology, racial differences in actual treatment utilization and responses to treatment is needed to refine optimal strategies for eliminating disparities and ensuring that all women benefit equally from medical advances and public health efforts to reduce the burden of breast cancer.
Acknowledgments
FUNDING
This work was supported by the National Cancer Institute at the National Institutes of Health (grant number 2U01CA088283 and KO5CA96940 to J.S.M.) and the Department of Defense Breast Cancer Center of Excellence Award (BC043120 to J.S.M.). Breast Cancer Surveillance Consortium data collection was supported by NCI-funded Breast Cancer Surveillance Consortium co-operative agreements (U01CA63740, U01CA86076, U01CA86082, U01CA63736, U01CA70013, U01CA69976, U01CA63731, and U01CA70040).
Role of the Funding Sources
Staff from NCI and BCSC provided some data and technical assistance. Model results are the sole responsibility of the authors. The funder did not have the right to pre-approve publication of the results.
We thank the NCCN investigators for use of data on treatment dissemination.
We thank the BCSC investigators for the data they have provided for this study. A list of the BCSC investigators and procedures for requesting BCSC data for research purposes are provided at: http://breastscreening.cancer.gov/.
Footnotes
D. Miglioretti, personal communication, January 2008
References
- 1.American Cancer Society. Cancer Facts & Figures 2009. Atlanta, GA: American Cancer Society; 2009. [Google Scholar]
- 2.Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005 Oct 27;353(17):1784–92. doi: 10.1056/NEJMoa050518. [DOI] [PubMed] [Google Scholar]
- 3.Smigal C, Jemal A, Ward E, et al. Trends in breast cancer by race and ethnicity: update 2006. CA Cancer J Clin. 2006 May–Jun;56(3):168–83. doi: 10.3322/canjclin.56.3.168. [DOI] [PubMed] [Google Scholar]
- 4.Lantz PM, Mujahid M, Schwartz K, et al. The influence of race, ethnicity, and individual socioeconomic factors on breast cancer stage at diagnosis. Am J Public Health. 2006 Dec;96(12):2173–8. doi: 10.2105/AJPH.2005.072132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li CI, Malone KE, Daling JR. Differences in breast cancer stage, treatment, and survival by race and ethnicity. Arch Intern Med. 2003 Jan 13;163(1):49–56. doi: 10.1001/archinte.163.1.49. [DOI] [PubMed] [Google Scholar]
- 6.Mandelblatt J, Andrews H, Kao R, Wallace R, Kerner J. Impact of access and social context on breast cancer stage at diagnosis. J Health Care Poor Underserved. 1995;6(3):342–51. doi: 10.1353/hpu.2010.0449. [DOI] [PubMed] [Google Scholar]
- 7.Smith-Bindman R, Miglioretti DL, Lurie N, et al. Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Ann Intern Med. 2006 Apr 18;144(8):541–53. doi: 10.7326/0003-4819-144-8-200604180-00004. [DOI] [PubMed] [Google Scholar]
- 8.Press R, Carrasquillo O, Sciacca RR, Giardina EG. Racial/ethnic disparities in time to follow-up after an abnormal mammogram. J Womens Health (Larchmt) 2008 Jul–Aug;17(6):923–30. doi: 10.1089/jwh.2007.0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lannin DR, Mathews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS. Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. JAMA. 1998 Jun 10;279(22):1801–7. doi: 10.1001/jama.279.22.1801. [DOI] [PubMed] [Google Scholar]
- 10.Joslyn SA, West MM. Racial differences in breast carcinoma survival. Cancer. 2000 Jan 1;88(1):114–23. doi: 10.1002/(sici)1097-0142(20000101)88:1<114::aid-cncr16>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 11.Bickell NA, Wang JJ, Oluwole S, et al. Missed opportunities: racial disparities in adjuvant breast cancer treatment. J Clin Oncol. 2006 Mar 20;24(9):1357–62. doi: 10.1200/JCO.2005.04.5799. [DOI] [PubMed] [Google Scholar]
- 12.Lund MJ, Brawley OP, Ward KC, Young JL, Gabram SS, Eley JW. Parity and disparity in first course treatment of invasive breast cancer. Breast Cancer Res Treat. 2008 Jun;109(3):545–57. doi: 10.1007/s10549-007-9675-8. [DOI] [PubMed] [Google Scholar]
- 13.Gwyn K, Bondy ML, Cohen DS, et al. Racial differences in diagnosis, treatment, and clinical delays in a population-based study of patients with newly diagnosed breast carcinoma. Cancer. 2004 Apr 15;100(8):1595–604. doi: 10.1002/cncr.20169. [DOI] [PubMed] [Google Scholar]
- 14.Tammemagi CM, Nerenz D, Neslund-Dudas C, Feldkamp C, Nathanson D. Comorbidity and survival disparities among black and white patients with breast cancer. JAMA. 2005 Oct 12;294(14):1765–72. doi: 10.1001/jama.294.14.1765. [DOI] [PubMed] [Google Scholar]
- 15.Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006 Jun 7;295(21):2492–502. doi: 10.1001/jama.295.21.2492. [DOI] [PubMed] [Google Scholar]
- 16.Vona-Davis L, Rose DP. The influence of socioeconomic disparities on breast cancer tumor biology and prognosis: a review. J Womens Health (Larchmt) 2009 Jun;18(6):883–93. doi: 10.1089/jwh.2008.1127. [DOI] [PubMed] [Google Scholar]
- 17.Mandelblatt J, Schechter CB, Lawrence W, Yi B, Cullen J. The SPECTRUM population model of the impact of screening and treatment on U.S. breast cancer trends from 1975 to 2000: principles and practice of the model methods. J Natl Cancer Inst Monogr. 2006;(36):47–55. doi: 10.1093/jncimonographs/lgj008. [DOI] [PubMed] [Google Scholar]
- 18.Tan SY, van Oortmarssen GJ, de Koning HJ, Boer R, Habbema JD. The MISCAN-Fadia continuous tumor growth model for breast cancer. J Natl Cancer Inst Monogr. 2006;(36):56–65. doi: 10.1093/jncimonographs/lgj009. [DOI] [PubMed] [Google Scholar]
- 19.http://cisnet.cancer.gov/.
- 20.Carter SB, Gartner SS, Haines MR, Olmstead AL, Sutch R, Wright G. Population. Vol. 1. New York: Cambridge University Press; 2006. Historical Statistics of the United States. [Google Scholar]
- 21.Holford TR, Cronin KA, Mariotto AB, Feuer EJ. Changing patterns in breast cancer incidence trends. J Natl Cancer Inst Monogr. 2006;(36):19–25. doi: 10.1093/jncimonographs/lgj016. [DOI] [PubMed] [Google Scholar]
- 22.Cronin KA, Mariotto AB, Clarke LD, Feuer EJ. Additional common inputs for analyzing impact of adjuvant therapy and mammography on U.S. mortality. J Natl Cancer Inst Monogr. 2006;(36):26–9. doi: 10.1093/jncimonographs/lgj005. [DOI] [PubMed] [Google Scholar]
- 23.Cronin KA, Yu B, Krapcho M, et al. Modeling the dissemination of mammography in the United States. Cancer Causes Control. 2005 Aug;16(6):701–12. doi: 10.1007/s10552-005-0693-8. [DOI] [PubMed] [Google Scholar]
- 24.Cronin KA, Miglioretti DL, Krapcho M, et al. Bias associated with self-report of prior screening mammography. Cancer Epidemiol Biomarkers Prev. 2009 Jun;18(6):1699–705. doi: 10.1158/1055-9965.EPI-09-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mariotto A, Feuer EJ, Harlan LC, Wun LM, Johnson KA, Abrams J. Trends in use of adjuvant multi-agent chemotherapy and tamoxifen for breast cancer in the United States: 1975–1999. J Natl Cancer Inst. 2002 Nov 6;94(21):1626–34. doi: 10.1093/jnci/94.21.1626. [DOI] [PubMed] [Google Scholar]
- 26.Mariotto AB, Feuer EJ, Harlan LC, Abrams J. Dissemination of adjuvant multiagent chemotherapy and tamoxifen for breast cancer in the United States using estrogen receptor information: 1975–1999. J Natl Cancer Inst Monogr. 2006;(36):7–15. doi: 10.1093/jncimonographs/lgj003. [DOI] [PubMed] [Google Scholar]
- 27.Early Breast Cancer Trialists’ Collaborative Group. Polychemotherapy for early breast cancer: an overview of the randomised trials. Lancet. 1998 Sep 19;352(9132):930–42. [PubMed] [Google Scholar]
- 28.Early Breast Cancer Trialists’ Collaborative Group. Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet. 1998 May 16;351(9114):1451–67. [PubMed] [Google Scholar]
- 29.Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005 May 14–20;365(9472):1687–717. doi: 10.1016/S0140-6736(05)66544-0. [DOI] [PubMed] [Google Scholar]
- 30.Dignam JJ. Efficacy of systemic adjuvant therapy for breast cancer in African-American and Caucasian women. J Natl Cancer Inst Monogr. 2001;(30):36–43. doi: 10.1093/oxfordjournals.jncimonographs.a003458. [DOI] [PubMed] [Google Scholar]
- 31.SEER*Stat Database: Incidence - SEER 9 Regs Research Data. Nov 2008 Sub (1973–2006) <Katrina/Rita Population Adjustment> - Linked To County Attributes - Total U.S., 1969–2006 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2009, based on the November 2008 submission.
- 32.SEER*Stat Database: Mortality - All COD. Aggregated With State, Total U.S. (1969–2006) <Katrina/Rita Population Adjustment>, National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released May 2009.
- 33.Thamer M, Richard C, Casebeer AW, Ray NF. Health insurance coverage among foreign-born US residents: the impact of race, ethnicity, and length of residence. Am J Public Health. 1997 Jan;87(1):96–102. doi: 10.2105/ajph.87.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Curtis E, Quale C, Haggstrom D, Smith-Bindman R. Racial and ethnic differences in breast cancer survival: how much is explained by screening, tumor severity, biology, treatment, comorbidities, and demographics? Cancer. 2008 Jan 1;112(1):171–80. doi: 10.1002/cncr.23131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wujcik D, Shyr Y, Li M, et al. Delay in diagnostic testing after abnormal mammography in low-income women. Oncol Nurs Forum. 2009 Nov;36(6):709–15. doi: 10.1188/09.ONF.709-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keating NL, Kouri E, He Y, Weeks JC, Winer EP. Racial differences in definitive breast cancer therapy in older women: are they explained by the hospitals where patients undergo surgery? Med Care. 2009 Jul;47(7):765–73. doi: 10.1097/MLR.0b013e31819e1fe7. [DOI] [PubMed] [Google Scholar]
- 37.Gorin SS, Heck JE, Cheng B, Smith SJ. Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Intern Med. 2006 Nov 13;166(20):2244–52. doi: 10.1001/archinte.166.20.2244. [DOI] [PubMed] [Google Scholar]
- 38.Hershman DL, Unger JM, Barlow WE, et al. Treatment quality and outcomes of African American versus white breast cancer patients: retrospective analysis of Southwest Oncology studies S8814/S8897. J Clin Oncol. 2009 May 1;27(13):2157–62. doi: 10.1200/JCO.2008.19.1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002 Oct 9;288(14):1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 40.Carmichael AR. Obesity as a risk factor for development and poor prognosis of breast cancer. Bjog. 2006 Oct;113(10):1160–6. doi: 10.1111/j.1471-0528.2006.01021.x. [DOI] [PubMed] [Google Scholar]
- 41.Griggs JJ, Sorbero ME, Lyman GH. Undertreatment of obese women receiving breast cancer chemotherapy. Archives of internal medicine. 2005 Jun 13;165(11):1267–73. doi: 10.1001/archinte.165.11.1267. [DOI] [PubMed] [Google Scholar]
- 42.Daling JR, Malone KE, Doody DR, Johnson LG, Gralow JR, Porter PL. Relation of body mass index to tumor markers and survival among young women with invasive ductal breast carcinoma. Cancer. 2001 Aug 15;92(4):720–9. doi: 10.1002/1097-0142(20010815)92:4<720::aid-cncr1375>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 43.Cohen SS, Palmieri RT, Nyante SJ, et al. Obesity and screening for breast, cervical, and colorectal cancer in women: a review. Cancer. 2008 May 1;112(9):1892–904. doi: 10.1002/cncr.23408. [DOI] [PubMed] [Google Scholar]
- 44.Elmore JG, Carney PA, Abraham LA, et al. The association between obesity and screening mammography accuracy. Arch Intern Med. 2004 May 24;164(10):1140–7. doi: 10.1001/archinte.164.10.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fair AM, Wujcik D, Lin JM, et al. Obesity, gynecological factors, and abnormal mammography follow-up in minority and medically underserved women. J Womens Health (Larchmt) 2009 Jul;18(7):1033–9. doi: 10.1089/jwh.2008.0791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mandelblatt JS, Schechter CB, Yabroff KR, et al. Benefits and costs of interventions to improve breast cancer outcomes in African American women. J Clin Oncol. 2004 Jul 1;22(13):2554–66. doi: 10.1200/JCO.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 47.Breen N, Wagener DK, Brown ML, Davis WW, Ballard-Barbash R. Progress in cancer screening over a decade: results of cancer screening from the 1987, 1992, and 1998 National Health Interview Surveys. J Natl Cancer Inst. 2001 Nov 21;93(22):1704–13. doi: 10.1093/jnci/93.22.1704. [DOI] [PubMed] [Google Scholar]
- 48.Jones BA, Kasl SV, Curnen MG, Owens PH, Dubrow R. Can mammography screening explain the race difference in stage at diagnosis of breast cancer? Cancer. 1995 Apr 15;75(8):2103–13. doi: 10.1002/1097-0142(19950415)75:8<2103::aid-cncr2820750813>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 49.McCarthy EP, Burns RB, Coughlin SS, et al. Mammography use helps to explain differences in breast cancer stage at diagnosis between older black and white women. Ann Intern Med. 1998 May 1;128(9):729–36. doi: 10.7326/0003-4819-128-9-199805010-00005. [DOI] [PubMed] [Google Scholar]
- 50.Du W, Simon MS. Racial disparities in treatment and survival of women with stage I–III breast cancer at a large academic medical center in metropolitan Detroit. Breast Cancer Res Treat. 2005 Jun;91(3):243–8. doi: 10.1007/s10549-005-0324-9. [DOI] [PubMed] [Google Scholar]