Abstract
Daclizumab, an antibody against the IL-2Rα chain, inhibits brain inflammation in MS patients, while expanding CD56bright immunoregulatory NK cells in vivo. We hypothesized that this unexpected expansion is paradoxically IL-2 driven; caused by the increased availability of T-cell derived IL-2 for NK cell signaling.
To this end we performed ex vivo functional analyses of CD56bright NK cells and T cells from patients in clinical trials with daclizumab. We developed in vitro models to investigate mechanisms for ex vivo observations.
We observed that daclizumab treatment caused decreased numbers and proliferation of FoxP3+ Tregs, a model T cell population known to be dependent on IL-2 for proliferation and survival. As anticipated, daclizumab therapy inhibited IL-2 signaling in all T cells; however we also observed functional adaptation of T cells to low IL-2 signal in vivo, characterized by the concomitant enhancement of IL-7 signaling on all T cells and parallel increase of CD127 expression by Tregs. In contrast, IL-2 signaling on CD56bright NK cells was not inhibited by daclizumab and their in vivo proliferation and cytotoxicity actually increased. Mechanistic studies indicated that the activation of CD56bright NK cells was likely IL-2 driven, as low doses of IL-2, but not IL-15, mimicked this activation in vitro.
Our study provides insight into the role that IL-2 and CD25 play in functional regulation of two important immunoregulatory cell populations in humans: FoxP3+ T regs and CD56bright NK cells.
Introduction
Natural Killer (NK) cells are an important element of the innate immune system and act against virally infected cells and tumor cells through a complex set of activating and inhibitory signals, the processing of which may lead to cytotoxicity or release of cytokines (1). In humans, there are two main classes of NK cells: CD56dim and CD56bright NK cells. CD56dim NK cells, which constitute the majority (~90%) of NK cells in peripheral blood, produce large amounts of perforin and mediate robust cytotoxicity toward MHC-I deficient targets. Alternatively, CD56bright NK cells, representing only a small fraction (~10%) of NK cells in the blood, are found in higher proportions in the lymph nodes and inflammatory lesions. They are thought to have immunoregulatory properties, primarily through their rapid production of cytokines following activation (2). Due to their lower perforin and granzyme B production, CD56bright NK cells were originally considered not to be cytotoxic. However, recent data indicate that they constitutively express granzymes A and K (3) and in addition to killing MHC-I-deficient targets, they also kill very different targets than those killed by CD56dim NK cells, namely autologous MHC-I-expressing immature dendritic cells (iDC) (4) and activated T cells (5).
Multiple Sclerosis (MS) is a debilitating immune-mediated disease of the central nervous system (CNS). While the cause of the disease is not known, it is believed that the aberrant activation of the adaptive immune system underlies focal CNS tissue destruction visible by magnetic resonance imaging (MRI) as MS lesions. Dysfunctional NK cells were described in relation to MS as early as 1980 when Benczur et al. found decreased NK cytotoxicity toward MHC-I deficient targets in MS patients (6). More recently, a correlation was found between periods of low NK cell functional activity and MS disease activity identified as new lesions on MRI scans in a time-course study of patients with relapsing-remitting MS (7). In the mouse model of MS, experimental autoimmune encephalomyelitis (EAE), NK cell-depleting antibodies (Ab) administered to mice prior to immunization with myelin oligodendrocyte glycoprotein (MOG)35–55 caused earlier onset and increased severity of EAE (8). These, and many other human and animal studies (reviewed in (9)) suggest that NK cells may play an important role in limiting neuroinflammation and perhaps autoimmunity in general (10).
CD25, the IL-2 receptor α-chain, has been genetically linked to MS disease susceptibility (11). When CD25 associates with the intermediate affinity IL-2 receptor (IL-2R; Kd = 1nM), composed of a β-chain (CD122) and the common γ-chain (CD132), it increases the affinity of the signaling complex for IL-2 10–100 fold; thus forming the high affinity IL-2R (Kd = 10pM) (12). Because the high affinity IL-2R is expressed on T cells upon their activation and is believed to facilitate T cell entry into the proliferation cycle, CD25 blocking Abs (e.g. daclizumab and basiliximab) were developed as immunomodulatory agents that could selectively inhibit activated T cells (13). Indeed, these agents inhibit the rejection of solid organ transplantation and daclizumab also limits immune-mediated pathology associated with inflammatory uveitis (14) and MS (15–18). We have previously reported that the inhibitory effect of daclizumab on MS disease activity is linked to the expansion of CD56bright NK cells in treated patients (5). We observed that CD56bright NK cells expanded during daclizumab therapy exhibited higher expression of IL-2 receptor β-chain and proliferated more vigorously in response to IL-2 and IL-15 in vitro than their counterparts isolated before daclizumab administration. Additionally, the expanded CD56bright NK cells had higher surface expression of IL-2 regulated genes, such as CD44, CD127 (IL-7Rα) and KIR2DL4. Therefore, we hypothesized that daclizumab expands CD56bright NK cells in an IL-2-dependent manner; by enhancing the availability of IL-2 for NK cell signaling via the intermediate affinity IL-2R due to decreased consumption of IL-2 by activated T cells.
However, the evidence for this hypothesis was only indirect. Furthermore, a similar hypothesis for the IL-2 driven proliferation of CD56bright NK cells was tested previously during therapeutic administration of IL-2 to cancer patients and was felt to be incorrect (19). Specifically, based on cell cycle analysis, Fehniger et al. concluded that the robust expansion of CD56bright NK cells in IL-2-treated cancer patients previously treated with chemotherapy resulted from enhanced NK cell differentiation from bone marrow progenitors combined with an IL-2-induced delay in NK-cell death, rather than from NK cell proliferation. Because of the apparent importance of CD56bright NK cells in regulation of neuroinflammation and the genetic link of CD25 to MS, we sought to characterize the mechanism of action of daclizumab in MS, including the mechanism of expansion of CD56bright NK cells, in greater detail. To this end, we investigated all components of our hypothesis directly by analyzing matched cryopreserved samples collected from 25 MS patients who participated in two previously published clinical trials of daclizumab in MS (17, 20): 1. We observed the expansion of CD56bright NK cells under daclizumab therapy and examined their in vivo proliferation by quantification of Ki67 staining. 2. We searched for direct ex vivo evidence that daclizumab inhibits IL-2 signaling in T cells by quantifying the numbers of FoxP3+CD4+ regulatory T cells (Tregs), which are known to be dependent on IL-2 signal for their survival (21). 3. We directly analyzed STAT5 phosphorylation by T cells and NK cells in response to exogenous IL-2. 4. We measured NK cell functional activity directly ex vivo, by employing a flow cytometry based killing assay of GFP-tagged MHC-I deficient target cells combined with CD107a staining that identifies degranulating effector cells. 5. Finally, we performed in vitro functional studies, including transwell experiments and an IL-2 consumption assay to further support our conclusions.
Materials and Methods
Patient samples
To conduct these experiments, we used cryopreserved PBMC samples isolated from lymphocytapheresis taken from patients in two separate trials: one as described in (17) where patients who were unresponsive to IFN-β therapy at baseline, were treated with daclizumab and IFN-β combination therapy and taken off IFN-β at late time points, and another trial where daclizumab was used as monotherapy (20). No significant differences were found between the two cohorts unless otherwise noted.
Ex vivo lymphocyte proliferation and FoxP3 staining
Cryopreserved PBMCs were thawed and 1×106 cells were stained for FoxP3 and Ki67 (FoxP3 staining buffer set; eBioscience; San Diego, CA). Samples were acquired by flow cytometry (LSR II, with HTS; BD Biosciences; San Jose, CA) and analyzed with FACS Diva software (BD Biosciences). Antibodies (and clones) used include: Ki-67 (B56), CD127 (HIL-7R-M21), CD56 (B159), CD8 (RPA-T8), CD4 (SK3), CD3 (SK7; all BD Biosciences), FoxP3 (236A/E7) and CD25 (BC96; eBioscience). Staining was performed in duplicates and gating was set on appropriate isotype controls.
Ex vivo signaling assays
Cryopreserved PBMCs were thawed and plated in X-vivo media (Lonza, Walkersville, MD) at 1×105 cells/well in a 96-well plate. They were rested for one hour at 37°C and pulsed with 50–100 IU/ml of IL-2 (NCI RBR Preclinical Repository; Frederick, MD, USA; all patients were tested with 100 IU/ml, a subgroup was tested also with 50 IU/ml) or 10ng/ml IL-7 (PeproTech; Rocky Hill, NJ) for 10 minutes; following which, they were fixed, permeabilized (Cytofix buffer and PhosFlow Perm buffer II, BD Biosciences) and stained with antibodies acceptable for phospho-specific staining. Antibodies used include: CD56 (MY31), CD3 (UCHT1), pSTAT5 (47, pY694-STAT5; all BD Biosciences) and CD4 (RPA-T4; eBioscience). Previous studies have determined the validity of the PhosFlow signaling methodology applied to cryopreserved PBMCs (22).
IL-2 consumption assay
Cryopreserved PBMCs were thawed and NK cells were depleted by CD56 iMag microbeads (BD Biosciences). Alternatively, T cells were isolated from PBMCs from lymphocytaphereses by negative selection (T cell isolation kit II, Miltenyi Biotech). 1×106/ml of T cells or NK-depleted PBMCs were plated in IMDM media (Lonza) containing 10% human serum and either M-A251 control antibody against CD25 which does not block the IL-2-binding tac epitope (BD Biosciences) or daclizumab (Zenapax, Hoffman-La Roche Inc., Nutley, NJ; 10ug/ml each). After incubating with the antibodies at 37°C for one hour, T cells were polyclonally stimulated with CD3/CD28 Dynabeads (Invitrogen; Carlsbad, CA) at a 0.3:1 bead:cell ratio. After IL-2 production tapered off (72 hours later), cells were washed thoroughly, recounted and reseeded at 1×106/ml in 10% human serum media with 20IU/ml IL-2 (NCI RBR Preclinical Repository; Frederick, MD), maintaining original Ab concentrations. After 48 hours, supernatants were collected and measured for IL-2 by ELISA (IL-2 Ready-Set-Go ELISA kit; eBioscience).
In vitro NK cell proliferation assays
Cryopreserved PBMCs from MS patients that have continued on long term daclizumab therapy were thawed and NK cells and T cells were isolated by negative selection (MACS Human NK Cell Isolation Kit and MACS Pan T cell Isolation Kit II, Miltenyi Biotec; Auburn, CA). These populations were determined to be of 89.1% and 96.5% purity respectively by FACS. T cells and NK cells were rested overnight in IMDM media (Lonza) with 10% AB human serum (Gemini Bio-Products; West Sacramento, CA). The NK cells were then CFSE stained (carboxyfluorescein diacetate succinimidyl diester; Molecular Probes, Invitrogen) as described previously (5) and co-cultured with T cells. The T cells were seeded at 5×104 cells/condition (200μl 10% serum in IMDM and preincubated with daclizumab for 1 hour to prevent T cell consumption of IL-2, washed twice and stimulated with CD3/CD28 Dynabeads (Invitrogen) before co-culture with increasing numbers (1×104, 2.5×104 or 5×104) of NK cells. In transwell experiments, PBMCs were CFSE stained and then NK cells were separated/depleted by CD56 microbeads (Miltenyi Biotec). The NK-depleted PBMCs were polyclonally activated with plate-bound anti-CD3 (20ng/ml) and anti-CD28 (10μg/ml) Abs (PeproTech) and the NK cells were added into transwells (3-μm pore size, Polycarbonated Membrane; Corning Costar, Lowell, MA) at a 1:10 NK:T cell ratio. Alternatively, the transwell experiment was repeated with purified, negatively-selected T cells and NK cells. T cells were polyclonally activated for 24–72 hours, extensively washed and re-seeded to the lower compartment of transwells at 1×106 activated T cells in media containing different blocking agents as indicated. Autologous NK cells were isolated from fresh or cryopreserved apheresis samples at the day of co-culture with previously activated T cells. In order to differentiate between NK cells added to the upper compartment and activated T cells added to the lower compartment of transwell, only purified NK cells were CFSE stained before co-culture. Proliferation assays were analyzed by FACS at day 3–5 for CFSE dilution. Absolute numbers of proliferating cells were evaluated as a ratio of CFSE diluted NK cells to FITC beads that were added in equal number to each well before acquisition.
GFP transduction of K562 cells and ex vivo NK cytotoxity assay
To fluorescently tag K562 MHC-I deficient tumor cells, they were transduced with GFP. Briefly, pMSGV1-eGFP, a retroviral vector carrying the GFP gene, was co-transfected with pRD114, providing ENV for efficient packaging into the packaging cell line, 293-GP. Pseudotype virus expressing eGFP was harvested and used for K562 transduction.
To make the GFP viral supernatant, 293GP cells (Clontech; Mountain View, CA) were seeded at 6×106 cells/well in a 10cm plate coated with Poly-D-Lysine (BD Biosciences). 9μg pMSGV1-GFP and 4.5μg pRD114 were transfected into 293-GP using Lipofectamine 2000 (Invitrogen) following the manufacturer’s protocol. 24–48 hr-post transfection, supernatants were collected and spun at 1000 ×g, at room temperature for 10 min to remove cell debris. For the transduction of the GFP gene into K562 cells, 4×106 K562 cells/well, pre-washed with PBS, were mixed with 3 ml viral supernatant, 1 ml fresh media, 10 μg/ml protamine sulfate (APP Pharmaceuticals; Schaumburg, IL) and plated in a 6-well plate. The plate was centrifuged at 1000 ×g, at 32°C for two hours and then cultured in a 37°C, 5% CO2 incubator. GFP expression was monitored using fluorescence microscopy and FACS.
Single K562 GFP clones were generated following a 0.3 cell/well limiting dilution of the eGFP transduced K562 cell mixture. Cells in eGFP positive wells were expanded and the purity of the clone and intensity of eGFP expression were confirmed by FACS analysis.
Natural killer cell cytotoxicity was measured in a similar fashion to a protocol previously described (23). Cryopreserved PBMCs were thawed and plated at 1×106 cells/well and rested for 30 minutes at 37°C before adding 1×105 GFP-transduced MHC-I deficient K562 target cells and CD107a antibody (H4A3; BD Biosciences). Control wells included effectors (NK cells only with CD107a Ab) without targets and targets (K562 cells only) without effectors. Cultures were incubated overnight, and subsequently stained for surface expression of CD3 (UCHT1), CD8 (RPA-T8), and CD56 (MY31; BD Biosciences). They were acquired by flow cytometry, additionally assessing for the presence of GFP and CD107a. Live GFP+ cells were gated on forward and side scatter and gating for CD107a (i.e. degranulation) was set from control wells of effectors without targets. Cells were proportionally enumerated between different conditions using a reference number of fluorescent beads that were added in equal numbers to all conditions.
In vitro NK cytotoxity assay
Fresh PBMCs from normal donors were isolated by ficoll separation (Lymphocyte Separation Medium; Lonza) and NK cells were isolated by negative selection (MACS Human NK cell Isolation Kit; Miltenyi). NK cells were then incubated overnight at 37°C and 5% CO2 in IMDM media (Lonza) containing 10% human serum (Gemini Bio-Products) with either no additional cytokine, 10 or 100 IU/ml IL-2, or 2 or 20 ng/ml IL-15 (PeproTech). They were then washed thoroughly and some aliquots were taken for intracellular staining of perforin as described (5). Following washing, NK cells were seeded in X-vivo media at 5×104 cells with 5×104 GFP+ K562 cells with 4 μl of CD107a PE-Cy5 Ab per pretreatment condition. Control wells were identical to those used in the ex vivo cytotoxicity assay described above. After 4 hours, the coculture assay was stained for CD107a incorporation and intracellular perforin and analyzed for death of GFP+ K562 cells. Antibodies used included CD56 (B159), CD3 (UCHT1), perforin (δG9), granzyme A (CB9) and CD107a (H4A3) (all BD Biosciences). Gating for perforin was set on the appropriate isotype control and gating for CD107a (i.e. degranulation) was set from control wells of effectors without targets. Perforin expression in cultures with targets was measured from CD107a+CD56bright NK cells that had released their granules in culture. Absolute numbers were again acquired using fluorescent beads for normalization.
Statistics
To compare therapy samples to baseline samples and in vitro proliferation data, we analyzed our data using one way RM ANOVA unless otherwise indicated. We used the Friedman one way RM ANOVA on Ranks to analyze in vitro cytotoxicity data using increasing cytokine levels and paired t-test for the IL-2 consumption assay. All differences listed in the text are changes in the median values. In figures, p<0.05 is annotated as *, p<0.01 is marked with ** and p<0.001 is marked with ***. Statistical analyses were performed with SigmaStat software version 3.5.
Results
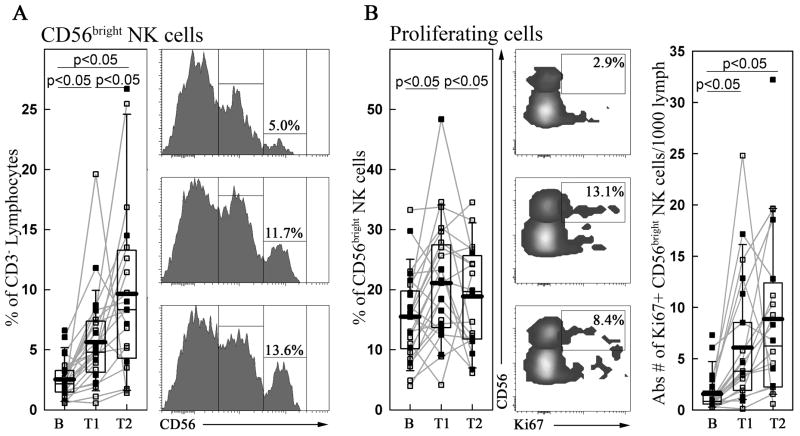
Daclizumab therapy causes increased proliferation of CD56bright NK cells
As previously reported (5, 17), CD56bright NK cells expand upon daclizumab therapy. Our results again illustrate the significant in vivo expansion of CD56bright NK cells that continues between early and late therapy time-points (B→T1: 115.6%; p<0.01 and T1→T2: 78.9%; p<0.001) (Fig. 1A). This expansion was at least partially driven by enhanced in vivo proliferation of CD56bright NK cells as demonstrated by an early increase in cells positive for Ki67, a chromosomal marker of cells undergoing mitosis (B→T1: 34.1%; p<0.01). However, the proliferation of CD56bright NK cells plateau as CD56bright NK cells expanded, as the proportion of proliferating CD56bright NK cells decreased slightly between T1 and T2 (T1→T2: −8.8%; Fig. 1B). Nevertheless, the absolute numbers of proliferating CD56bright NK cells remained significantly higher than at baseline during the entire daclizumab treatment (B→T1: +303.1%; B→T2: +591.5%; p<0.05; Fig. 1B right panel).
Figure 1. Ex vivo CD56bright NK cell proliferation.
Cryopreserved PBMCs were stained prior to permeabilization for NK cell marker CD56, T cell marker CD3 (A) and following permeabilization, stained for intranuclear proliferation marker Ki67 (B) at baseline and treatment time points (B, T1 & T2). Ki67 gating was set individually on CD56bright NK cells only. Both proportion (left panel) and absolute numbers of proliferating CD56bright NK cells per 1000 gated lymphocytes (right panel) are depicted. Patients from the monotherapy trial are indicated by open squares and patients from the combination therapy trial are indicated by black squares. Means are marked with a thick black line. Raw data FACS plots are taken from a representative patient.
In this case we observed differences between the patients in the daclizumab monotherapy trial versus those that took daclizumab as an add-on therapy to IFN-β during the first 6 months of treatment (i.e. combination therapy trial; please see methods for a detailed explanation of the differences between the two trials). At baseline, patients from the combination therapy trial had significantly higher numbers of CD56bright NK cells (55.4%, p<0.05: Mann-Whitney Rank Sum test) than patients from the monotherapy trial. Accordingly, the decrease in the proportion of Ki67+ proliferating CD56bright NK cells from T1 to T2 was almost entirely driven by patients from the combination therapy trial (−46.0% in combination therapy patients versus −5.7% in monotherapy patients; p<0.05; t-test). Daclizumab treatment did not the affect number of CD56dim NK cells (−6.6% from B to T2; ns).
FoxP3+ T regulatory cell populations decrease after therapy and proliferate at lower rates
We hypothesized that the observed expansion and enhanced proliferation of CD56bright NK cells was due to higher in vivo availability of IL-2, because daclizumab inhibited IL-2 consumption by T cells. However, in vivo IL-2 production generally occurs at sites of immune activation, such as in lymphoid organs or inflamed tissues, which are not amenable to ex vivo testing. Therefore, we utilized FoxP3+ Tregs as a surrogate marker for in vivo IL-2 consumption by T cells, because FoxP3+ Tregs are known to constitutively express CD25 and are dependent on IL-2 for their proliferation and survival. Intranuclear staining for transcription factor FoxP3 (example of raw data in Supplementary Fig. 1) revealed that there was a statistically significant decrease in Treg populations induced by daclizumab therapy (B→T1: −39.1%; B→T2: −40.4%; p<0.001; Fig. 2A). Staining for Ki67 identified a proportion of proliferating Tregs, which decreased between B and T1 (B→T1: −24%; p<0.05), but apparently returned to baseline at T2 (B→T2: −1.5%; ns; Fig. 2B). However, when analyzing the number of proliferating Tregs per 1000 lymphocytes (Fig. 2C), it became clear that the absolute numbers of proliferating Tregs remained significantly below baseline values for both T1 and T2 (B→T1: −62.2%; B→T2: −58.4%; p<0.001; Fig. 2C).
Figure 2. Ex vivo Treg proliferation and CD127 expression.
Cryopreserved PBMCs were stained for intranuclear transcription factor FoxP3 (A) and proliferation marker Ki67 (B&C) at baseline and treatment time points (B, T1 & T2). Prior to permeabilization, they were stained for CD25 (D) and CD127 (E) expression, displayed here by mean fluorescence intensity (MFI) of the FoxP3+ Treg population. Furthermore, the MFI of Foxp3 expression on CD4+ CD25+ Tregs is displayed (F) for baseline and subsequent treatment time points. Patients from the monotherapy trial are indicated by open squares and patients from the combination therapy trial are indicated by black squares. * denotes p<0.05, ** denotes p<0.01, *** denotes p<0.001 and means are marked with a thick black line. FACS plots are taken from a representative patient.
The establishment of a new balance between absolute numbers of Tregs and their in vivo cycling indicated some type of functional adaptation of Tregs to the lack of high affinity IL-2 signaling induced by the blockade of CD25 by daclizumab (Fig. 2D). Because Tregs can utilize other γc-signaling cytokines (especially IL-7) for their development and survival (24), we investigated the changes in IL-7Rα expression (CD127) on Tregs. We observed a progressive increase in the level of expression of CD127 induced by daclizumab treatment (B→T1: +16%; p<0.01 and B→T2: +32.9%; p<0.01; Fig. 2E). The increased expression of CD127 in FoxP3+ CD4+ T cells may be seen in recently activated T cells, which lack suppressive function (25). However, it is unlikely that our gating included activated T cells, because the level of CD127 expression on the FoxP3+ CD4+ T cells remained significantly below the levels of CD127 expression on FoxP3− CD4+ T cells (MFI 198.5 vs. 803.8; p<0.001; Rank Sum Test) during the entire treatment period. Because another in vivo marker of the lack of IL-2 signaling on Tregs is their decreased expression of FoxP3 (24), we analyzed the level of FoxP3 expression on Tregs under daclizumab therapy (Fig. 2F) and observed that daclizumab induced a sustained decrease in FoxP3 MFI (B→T1: −12.6%; B→T2: −14.5%; p<0.001).
Signaling dynamics following the blocking of CD25
In order to examine how daclizumab therapy altered IL-2 signaling, we analyzed the phosphorylation of STAT5 on T cell and NK cell subsets in PBMCs by flow cytometry in response to exogenously added IL-2 (50–100 IU/ml).
IL-2-induced STAT5 phosphorylation on T cells (CD4+ T cells are depicted as a representative T cell subset; Fig. 3) was significantly inhibited by daclizumab therapy in comparison to baseline samples (B→T1: −40.2%; p<0.001, B→T2: −28%; p<0.001; Fig. 3A). We observed no changes in total STAT5 protein induced by daclizumab therapy (Supplementary Fig 2). There was additionally an early decrease by CD8+ T cells in STAT5 phosphorylation to IL-2 (B→T1: −36.8%; p<0.001; data not shown), but phosphorylation rebounded at the later timepoint (B→T2: 5.3%; p<0.05; data not shown). If cells were further incubated in vitro with daclizumab (10μg/ml) prior to IL-2 pulsing, signaling was completely abrogated at all time points (data not shown). As a signaling control we selected IL-7, because it also phosphorylates STAT5 and because we observed an upregulation of CD127 (the α-chain of the IL-7 receptor) on FoxP3+ Tregs. Surprisingly, we observed an increase in signaling to IL-7 by CD4+ T cells (B→T2: 35.6%; p<0.05; Fig. 3B) and CD8+ T cells (B→T2: 36.7%; p<0.001; data not shown).
Figure 3. Ex vivo IL-2 and IL-7 signaling.
Cryopreserved PBMCs from baseline and therapy time points (B, T1 & T2) were thawed and rested for an hour at 37°C in X-vivo media. They were subsequently pulsed with IL-2 (A&C) or IL-7 (B) for 10 minutes and then fixed in formaldehyde, washed, and permeabilized with methanol. They were then stained for surface markers and phosphorylated STAT5 (pSTAT5). Gating was set from control wells pulsed with X-vivo media lacking additional cytokines. For CD56bright NK cells (C), both the proportion (left panel) and absolute numbers (calculated per 1000 lymphocytes; right panel) of pSTAT5+ cells are displayed. Again, patients from the monotherapy trial are indicated by open squares and patients from the combination therapy trial are indicated by black squares. Means are marked with a thick black line. Raw data FACS plots are taken from a representative patient.
In contrast to the effect of daclizumab therapy on IL-2 signaling on T cells, we observed no inhibition of IL-2 signaling on CD56bright NK cells. In fact, there was an upward, non-significant trend in the proportion of CD56bright NK cells that phosphorylated STAT5 in response to IL-2 throughout the treatment course (Fig 3C). Due to daclizumab-induced expansion of CD56bright NK cells, this resulted in a highly significant increase in the absolute numbers of IL-2-induced pSTAT5+ CD56bright NK cells during daclizumab therapy (B→T1: +165.7%, B→T2: +407.0%; p<0.001; Fig 3C; right panel). We observed no significant changes in IL-7 induced STAT5 phosphorylation on CD56bright NK cells (data not shown).
In vitro model of IL-2 driven proliferation of CD56bright NK cells
So far our data indicate that daclizumab therapy inhibits IL-2 driven STAT5 phosphorylation by T cells, but does not affect IL-2 signaling on NK cells and that CD56bright NK cells proliferate more vigorously in vivo after initiation of daclizumab treatment. Activated T cells are the main producers of IL-2 in vivo and we have previously reported (5) that daclizumab treatment does not inhibit IL-2 secretion by activated T cells. Therefore, we wanted to examine if daclizumab limits the consumption of IL-2 by T cells and as a consequence, if the resultant excess of T cell-derived IL-2 can drive proliferation of CD56bright NK cells.
To this end, we performed an IL-2 consumption assay (Fig. 4A) where T cells were polyclonally activated for 3 days, then extensively washed and re-seeded in the presence of daclizumab or M-A251 control anti-CD25 Ab (10μg/ml each) and exogenously added IL-2 (20 IU/ml). Because the IL-2 production by T cells lasts 24–48h post-stimulation, and the CD25 expression peaks 72h post-stimulation (data not shown), the 72h time point was selected as optimal to measure IL-2 consumption. As demonstrated in Fig. 4A, activated T cells treated with M-A251 had almost completely consumed all exogenously added IL-2 (90.7%; p<0.05; paired t-test) in 24h. However daclizumab-treated activated T cells had consumed only 17% (ns; paired t-test) of exogenously added IL-2.
Figure 4. In vitro NK proliferation.
(A) IL-2 consumption by T cells was measured by ELISA from supernatants of activated T cells cultured with either daclizumab (Dac) or an anti-CD25 control Ab which does not bind to the IL-2 binding tac epitope (M-A251): T cells were polyclonally stimulated for 3 days, extensively washed and reseeded in equal numbers with exogenously added IL-2 (20 IU/ml) and Dac or M-A251 Ab (10μg/ml each). Supernatants were collected in 24–48h and the amount of IL-2 remaining was measured by ELISA. Samples were taken from 4 patients (2 patients with purified (negatively-selected) T cells and 2 with NK-depleted PBMC). (B) CFSE dilution of NK cells was measured after 5 days in culture with increasing ratios of daclizumab-treated CD3/CD28 stimulated T cells (n=4). (C & D) Transwell experiments: Negatively-selected T cells (or NK-depleted PBMC) were polyclonally activated for 24–72h and 1×106 activated T cells were seeded in the lower compartment of transwells in the presence of control Ab M-A251, daclizumab (Dac), IL-2-neutralizing Ab (α-IL-2) or 20IU IL-2. Autologous NK cells were negatively selected from either fresh or cryopreserved apheresis samples 24 hours before co-culture with activated T cells, they were CFSE stained and rested overnight before adding 1×105 NK cells into the transwell inserts. In 3–5 days, NK cell proliferation was assessed by CFSE dilution and their absolute numbers were proportionally enumerated between conditions by normalizing per 1000 fluorescent beads added prior to acquisition by flow cytometry. Because we observed that activated NK cells were able to migrate through 3μm pores in the transwell inserts to the T cell compartment, we present total cultures from both the upper compartment of the transwell (top row) and the lower compartment of the transwell (bottom row): (C) Representative raw data FACS plots (with numbers indicating absolute numbers of CD56bright (red) and CD56dim (blue) NK cells) and (D) enumeration of proportion and absolute numbers of proliferating CD56bright NK cells. Data are representative of 4 independent patients/experiments (2 for both purified T cells and 2 for NK-depleted PBMCs). (E & F) Supernatant-transfer experiments: Negatively-selected T cells were polyclonally activated for 24–72h in the presence/absence of control Ab M-A251, daclizumab or IL-2-neutralizing Ab (α-IL-2). Supernatant from these cultures were collected 24–48 hours post-activation and cryopreserved until testing. NK cells were isolated by negative selection from fresh or cryopreserved apheresis samples, CFSE stained and cultured for 3 days with collected supernatant from activated T cells: (E) FACS plots representative of NK cell proliferation (absolute numbers of CD56bright and CD56dim NK cells are depicted in the gates) and (F) enumeration of proportion and absolute numbers of proliferating CD56bright NK cells. Data are representative of 2 independent patients/experiments. * denotes p<0.05, *** denotes p<0.001.
Next, we evaluated the proliferation of CD56bright NK cells in co-culture with increasing numbers of T cells polyclonally activated in the presence of daclizumab (Fig. 4B). We observed that CD56bright NK cells in culture with larger numbers of T cells proliferated more vigorously compared to CD56bright NK cells cultured with fewer T cells (1:1→2.5:1: 66%; p<0.001, 2.5:1→5:1: 31.4%; p<0.001and 1:1→5:1: 116.6%; p<0.001).
To investigate whether T cell to NK cell contact is necessary for the observed enhanced proliferation we utilized transwells to separate CFSE stained NK cells from polyclonally activated T cells (Fig. 4C & D). We observed significantly enhanced survival and proliferation of CD56bright NK cells in transwell inserts if T cells were activated in the presence of daclizumab in comparison to control Ab M-A251 (Fig. 4C; compare first and second panels). Furthermore, proliferation of CD56bright NK cells was almost completely abrogated in the presence of IL-2 neutralizing Ab (Fig. 4C & D). Addition of a low dose of IL-2 (20IU/ml) enhanced proliferation of CD56bright NK cells above the M-A251 condition, but did not reach levels observed in the daclizumab condition. We also observed that activated NK cells were able to migrate through 3 μm pores of the transwell to the lower compartment, likely due to a strong chemotactic gradient produced by activated T cells. Our set up purity checks demonstrated >95% NK cell purity in the upper compartment and >95% T cell purity in the lower compartment (Supplementary Fig. 3) at the beginning of transwell co-culture. Yet, consistently in every experiment we observed transmigration of activated NK cells through 3 μm semipermeable membrane and in fact significant enrichment of proliferating CD56bright NK cells in the lower compartment. Therefore, we provide both raw and analyzed data depicting CFSE-stained NK cells and CFSE-negative T cells in both compartments.
Finally, to confirm that activated T cells were driving the proliferation of CD56bright NK cells through soluble IL-2, we performed supernatant transfer experiments, where we collected supernatants from activated T cells cultured for 24–48h in the presence of M-A251 control Ab or daclizumab in the presence or absence of IL-2 blocking Ab. We isolated NK cells by negative selection from apheresis samples; CFSE stained them and cultured them in supernatants collected from activated T cells for 3 days (Fig. 4E & F). Again, we observed that supernatants from activated T cells cultured in the presence of daclizumab induced proliferation of CD56bright NK cells that was at least 2–3 fold higher than proliferation of CD56bright NK cells cultured with the media from M-A251 cultures. Blockade of IL-2 resulted in complete abrogation of survival and proliferation of CD56bright NK cells.
CD56bright NK cells exhibit greater cytotoxicity following daclizumab therapy
In addition to describing the expansion of the CD56bright cell population, we sought to define functional changes of CD56bright NK cells induced by daclizumab therapy. In order to do this, we used a flow cytometric killing assay with GFP transduced MHC-I deficient cancer cell line, K562, as a target cell and utilized the detection of transient surface expression of LAMP protein CD107a, normally expressed only intracellularly in cytotoxic granules, as identification of effector cells in complex PBMC cultures. While both CD56dim and CD56bright NK cells (but not CD8+ or CD4+ T cells) are cytotoxic in this assay, the proportion of CD56dim NK cells in PBMC cultures and their activation status was not affected by daclizumab therapy (5); therefore, we expected that the observed changes could be directly attributed to changes in CD56bright NK cell subsets. We confirmed validity of this assumption by evaluating changes in the degranulation of both NK cell subsets.
In baseline samples we observed on average 14.5% killing of K562 cells (Fig 5A). This baseline cytotoxicity increased by 139.4% (p<0.01) to 34.7% killing at T1 and further by 55.1% (p<0.001) between T1 and T2 (T2: 53.9% killing). This enhanced cytotoxicity was paralleled by a significant increase in the proportion of degranulating CD56bright NK cells as visualized by CD107a incorporation (B→T1 +44.9%; p<0.001, B→T2 +50.4%; p=0.001; Fig. 5B). Analysis of the absolute numbers of degranulating NK cell subsets demonstrated a highly significant increase in the degranulating CD56bright NK cells (B→T1 +207.9%; p<0.001, B→T2 +530.2%; p<0.001; Fig. 5C; left panel) which correlated with the observed enhanced killing (RSpearman = 0.38, p=0.001; Fig. 5D). No significant change in the numbers of degranulating CD56dim NK cells was observed (Fig. 5C; right panel).
Figure 5. Ex vivo cytotoxicity.
Cryopreserved PBMCs were thawed and incubated with GFP+ K562 target cells and CD107a PE-Cy5 Ab overnight at 37°C. Co-cultures were stained the following day for CD3/CD56 and analyzed for (A) killing and (B) CD107a incorporation indicative of degranulation. Killing was measured as the percentage of K562 cells that were lost based on a condition with target cells only (A, top left). CD107a gating was set with conditions lacking target cells. Left panels summarize group data while right panels correspond to a representative example. (C) The absolute numbers of degranulating (CD107a+) CD56bright and CD56dim NK cells per 1000 lymphocytes are depicted for each time point (B, T1 and T2). Patients from the monotherapy trial are indicated by open squares and patients from the combination therapy trial are indicated by black squares. (D) The absolute numbers of degranulating CD56bright NK cells are positively correlated with the target killing using Spearman’s correlation. * denotes p<0.05, ** denotes p<0.01 and *** denotes p<0.001. Means are marked with a thick black line.
CD56bright NK cells respond to increases in IL-2 concentration by enhancing their cytotoxicity
While our data point to IL-2 as a central factor in the expansion and activation of CD56bright NK cells observed during daclizumab therapy, they do not rule out contributions of other factors that may be important in vivo, such as IL-15. Therefore, we next investigated whether IL-2 or IL-15 could induce changes in the function of CD56bright NK cells in vitro analogous to those observed after daclizumab therapy in vivo. Fresh NK cells were isolated by negative selection from healthy donor apheresis. These NK cells were stimulated overnight with varying amounts of IL-2 and IL-15 and subsequently examined for their ability to kill MHC-I negative targets. Intracellular cytokine staining following overnight activation revealed that all CD56bright NK cells expressed perforin, but increasing concentrations of IL-2 (Fig. 6A) and IL-15 (Fig. 6D) induced higher perforin expression (MFI) in NK cells that were cultured without targets. IL-2 was more effective in this regard, especially at lower concentrations (10IU/ml of IL-2 = 6.1 ng/ml increased perforin MFI by 61.3%; p=0.001, in comparison to 2ng/ml of IL-15, which increased perforin MFI by 26.9%; p<0.05). When NK cells were co-cultured with targets, they degranulated vigorously (Fig 6B and E), losing their intracellularly pre-formed perforin (Fig 6A and D; NK cells +target) as they killed GFP-tagged K562 cells (Fig. 6C and F). While both degranulation and K562 killing was again enhanced by IL-2 and IL-15; IL-2, especially at low doses, was significantly more effective in functional activation of CD56bright NK cells. Low dose IL-2 increased degranulation of CD56bright NK cells by 111.63% (Fig. 6B) in comparison to 35.94% induced by low dose IL-15 (Fig. 6D). Similarly, killing efficiency was enhanced by 32.8% (p<0.05; Fig. 6C) by low dose IL-2 and only by 2.36% (ns; Fig. 6F) by low dose IL-15. The loss of perforin MFI in CD56bright NK cells upon co-culture with targets (Δ perforin MFI −/+ target) was significantly greater when NK cells were pre-treated with IL-2 (+184.9% with IL-2 10IU/ml and +209.3% with IL-2 100IU/ml; p<0.05 for both; Fig 6A, right panel) as compared to IL-15 (+134.9% with IL-15 2ng/ml and +136.9% with IL-15 20ng/ml, both ns; Fig 6D, right panel). This cytokine-enhanced loss of perforin by CD56bright NK cells upon their co-culture with targets correlated strongly with enhanced efficacy of K562 killing (RSpearman = 0.718; p=0.00141; Supplementary Fig 4).
Figure 6. IL-2 enhances in vitro cytotoxicity.
NK cells were negatively isolated from healthy donor PBMCs and stimulated overnight with IL-2 (A–C) or IL-15 (D–F). They were measured for perforin expression both before (A&D, left panels) and after (A&D, right panels) culture with MHC-I deficient target K562 cells. Loss of perforin mean fluorescence intensity (MFI; Δ +/− target) was calculated as difference between perforin MFI measured in CD56bright NK cells cultured without- and with the targets. CD107a PE-Cy5 Ab was added prior to adding targets and 4 hours later the cultures were analyzed by flow cytometry for degranulation of gated CD56bright NK cells (B&E) and K562 killing (C&F). CD107a gating was set with conditions lacking target cells. Killing was measured as the percentage of K562 cells that were lost based on a condition with target cells only. * denotes p<0.05 and ** denotes p<0.01.
Discussion
In this study we present evidence that daclizumab increases the in vivo proliferation of CD56bright NK cells at the same time as it limits numbers and proliferation of IL-2-dependent FoxP3+ Tregs. Together with this increase in numbers, daclizumab therapy also enhances the ability of CD56bright NK cells to kill MHC-I-deficient targets, a function that can be mimicked in vitro by physiologically-achievable doses of IL-2, as well as less effectively by IL-15. Presented in vitro models indicate that daclizumab inhibits the consumption of IL-2 by activated T cells, leading to greater availability of this cytokine for signaling by CD56bright NK cells, which is paradoxically not inhibited, but rather enhanced by daclizumab treatment. While all these data are fully supportive of our hypothesis that daclizumab therapy leads to the paradoxical IL-2 driven activation and expansion of CD56bright NK cells, they do not exclude the possibility that other cytokines, such as e.g. IL-15 may also contribute to this effect in vivo. This is especially true because soluble IL-15, which we used in vitro, may not have the same effect as IL-15 transpresented in a complex bound to the IL-15 receptor α-chain (26) in vivo. However, while the IL-15/IL-15Rα complex activates human NK cells in vivo, it also induces differentiation of CD56bright NK cells into CD56dim NK cells (26), which we did not observe in association with daclizumab treatment. Collectively, our in vitro data supported by stated in vivo observations provide strong support for the role of IL-2 in the activation of CD56bright NK cells in daclizumab-treated subjects.
Our data do not contradict the possibility raised by Fehniger et al. (19) that IL-2 enhances differentiation of CD56bright NK cells from its precursors and inhibits apoptosis of these regulatory NK cells in vivo. In fact, we believe that both of these hypotheses are fully compatible. While Fehniger et al. did not observe increased proliferation of CD56bright NK cells expanded by IL-2 administration to cancer patients, these individuals were also treated with chemotherapeutic agents which could have inhibited cellular proliferation in vivo. Our Ki67 data clearly demonstrate that CD56bright NK cells proliferate more vigorously after initiation of daclizumab treatment in MS patients. The second difference between our study and the one performed by Fehniger et al. lies in the source of IL-2: while in one system IL-2 is provided exogenously, in our system, IL-2 is produced in the physiological environment (i.e. lymph node), most likely as a result of immune activation. As such, it is produced in a coordinated manner and likely in association with the production of other physiological factors (e.g. IL-15 by dendritic cells or activated monocytes/macrophages and IL-7 by stromal cells) which may further enhance the activation of CD56bright NK cells and their successful entry into the proliferation cycle. Our observation that as absolute numbers of CD56bright NK cells increase during daclizumab therapy, the proportion of proliferating CD56bright NK cells decreases (between T1 and T2 of daclizumab therapy) suggests that expanded NK cells compete for a limited source of IL-2 in vivo, thus ultimately leading to a plateau of CD56bright NK cells expansion during long-term daclizumab therapy.
As would be expected from its efficient blockage of the IL-2-binding tac epitope on CD25, daclizumab therapy inhibits the ability of T cells to phosphorylate STAT5 in response to 50–100 IU of exogenous IL-2. However, daclizumab does not inhibit STAT5 phosphorylation to the same dose of exogenously added IL-2 on CD56bright NK cells, despite the fact that a proportion of these cells (10–80% depending on the donor) express CD25 ex vivo. 50 IU/ml is a marginal dose (~2nM) for intermediate affinity IL-2R; indeed we have observed that decreasing this dose further to 10–20 IU/ml (<1nM) abrogates signaling also on NK cells (data not shown), consistent with published data that Kd for IL-2 binding to intermediate affinity receptor is 1nM (12). However, the fact that CD56bright NK cells still phosphorylate STAT5 to 50–100IU/ml of IL-2 in the presence of daclizumab while T cells do not, indicates that there is a wider range of IL-2 concentrations that can trigger signaling through the intermediate affinity IL-2R and that the final effective concentration likely depends on the expression levels of IL-2Rβ (CD122) and -γc (CD132) chains. We have previously demonstrated that CD56bright NK cells have 10-fold higher expression of CD122 in comparison to CD56dim NK cells and 100-fold higher expression of CD122 in comparison to T cells (5), a finding that likely underlies the differences we observed in the current study in the ability of CD56bright NK cells versus T cells to utilize intermediate affinity IL-2R for signaling.
When comparing baseline numbers and proliferation of CD56bright NK cells in patients participating in the daclizumab monotherapy trial, versus those that were enrolled in the daclizumab add-on trial to IFN-β, we observed significantly higher numbers of CD56bright NK cells in patients who were on IFN-β therapy in comparison to untreated patients. This observation is in agreement with the recent report of an expanded number of CD56bright NK cells in IFN-β-treated patients (27) and supports our previously-stated conclusion that IFN-β and daclizumab have an additive effect in the treatment of MS (17). Nevertheless, even in patients who participated in the daclizumab with IFN-β combination therapy trial, the numbers of CD56bright NK cells and their cytotoxicity further increased after withdrawal of IFN-β (i.e. between T1 and T2), indicating that daclizumab is significantly more potent than IFN-β in expanding and activating CD56bright NK cells in vivo.
Another unexpected finding in our study was the observation that the daclizumab-induced decrease in STAT5 phosphorylation to IL-2 was associated with a compensatory increase in IL-7 signaling on T cells. Both IL-2 and IL-7 (in addition to IL-4, -9, -15 and -21) utilize the common-γ chain (γc; CD132) as a part of their signaling complex. Animal data suggest that a hierarchy exists in the preferential recruitment of γc to IL-15R (and likely also IL-2R) as opposed to the IL-7 receptor (28). Furthermore, IL-2 signaling inhibits IL-7Rα chain (CD127) expression in activated T cells (29), indicating that while there is a partial overlap in the effects of these two cytokines on T cells (e.g. promoting T cell survival), the IL-2 signal is dominant under physiological conditions. A daclizumab-induced blockade of this physiological dominance of IL-2 signaling likely enhanced the availability of γc for IL-7 signaling. One apparent consequence of this compensatory increase in IL-7 signaling on CD4+ T cells is the stabilization of FoxP3+ Treg numbers and their in vivo proliferation during prolonged daclizumab treatment (i.e. between T1 and T2). Indeed, it was in this particular population of CD4+ T cells where we observed an increase in IL-7Rα (CD127) expression induced by daclizumab treatment. Animal studies indicate that some γc-signaling cytokines (specifically IL-7, and to a much lesser degree IL-15 but not IL-21) are able to enhance viability and upregulate FoxP3 expression in Tregs (24, 30), although not to the point that they can fully rescue the phenotype of IL-2 deficient mice. We observed stabilization of Treg numbers but also their levels of FoxP3 expression between T1 and T2 therapy time-points, at levels that represented 86% (MFI) to 60% (number of Tregs) of baseline values. Our data represent to our knowledge the first in vivo evidence that such a compensatory function of IL-7 on Tregs survival and proliferation also occurs in humans. Furthermore, these data present evidence for in vivo cross-regulation between CD25 and CD127-mediated signaling, which, based on genetic data (11), may play important role for development of human autoimmunity.
CD56bright NK cells are emerging as an important regulatory population in MS; however, it remains unclear whether they exert an immunoregulatory role on T cell responses predominantly in the lymphoid organs or whether they gain access to the CNS compartment. We believe that expansion of CD56bright NK cells occurs predominantly in lymph nodes, where IL-2 is produced under physiological conditions in healthy immune system (31). Indeed, several patients treated with daclizumab developed generalized lymphadenopathy with biopsy-proven expansion of CD56bright NK cells (unpublished observations). While current study focused on determining mechanism of daclizumab-induced expansion of CD56bright NK cells, follow-up studies will be required to expand our understanding how exactly these cells contribute to the inhibition of CNS inflammation in MS patients.
In conclusion, this current study significantly expands our knowledge about the pleiotrophic effects of this CD25-targeting therapy on the human immune system. Perhaps the most striking results in this regard are the vastly different effects of daclizumab therapy on two populations of CD25-expressing immunoregulatory cells: FoxP3+ Tregs and CD56bright NK cells. Proliferation of FoxP3+ Tregs cells is inhibited and their numbers are contracted, while proliferation of CD56bright NK cells is induced and their numbers are significantly expanded by CD25 blockade. We provide evidence that the main reason for this discrepancy lies in the differential ability of the intermediate affinity IL-2R expressed on T cells versus CD56bright NK cells to respond to physiological doses of IL-2. Thanks to a compensatory in vivo increase in IL-7 signaling, the quantitative decline in FoxP3+ Tregs under daclizumab therapy is significantly smaller (~30–40%) than the prominent increase in CD56bright NK cell numbers (>300%), proliferation (>400%) and their functional activity (~180%). As it is likely that different immunoregulatory cell populations have overlapping in vivo functions, perhaps this is the main reason why daclizumab therapy is generally well tolerated and has not been associated so far with the induction of lymphoproliferation and autoimmunity that has been observed in CD25-deficient animals.
Supplementary Material
Acknowledgments
The authors would like to thank Azita Kashani for expert blood processing. Also we thank Dr. Richard Morgan of the Surgery Branch, NCI, NIH for the generous donation of plasmids for the eGFP transduction of K562 cells.
Abbreviations
- CD25
IL-2Rα
- CD107a/LAMP1
Lysosomal-associated membrane protein-1
- CD122
IL-2Rβ, CD127
- FoxP3
Forkhead box P3, IL-7Rα
- CD132
common γ chain
- EAE
experimental autoimmune encephalomyelitis
- iDC
immature dendritic cells
- IL-2R
IL-2 receptor
- KIR2DL4
Killer cell immunoglobulin-like receptor 2DL4
- MOG
myelin oligodendrocyte glycoprotein
- MRI
magnetic resonance imaging
- MS
multiple sclerosis
- Treg
T regulatory cells
Footnotes
This research was supported by the Intramural Research Program of the NIH, NINDS.
References
- 1.Caligiuri MA. Human natural killer cells. Blood. 2008;112:461–469. doi: 10.1182/blood-2007-09-077438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cooper MA, Fehniger TA, Turner SC, Chen KS, Ghaheri BA, Ghayur T, Carson WE, Caligiuri MA. Human natural killer cells: a unique innate immunoregulatory role for the CD56 (bright) subset. Blood. 2001;97:3146–3151. doi: 10.1182/blood.v97.10.3146. [DOI] [PubMed] [Google Scholar]
- 3.Bratke K, Kuepper M, Bade B, Virchow JC, Jr, Luttmann W. Differential expression of human granzymes A, B, and K in natural killer cells and during CD8+ T cell differentiation in peripheral blood. Eur J Immunol. 2005;35:2608–2616. doi: 10.1002/eji.200526122. [DOI] [PubMed] [Google Scholar]
- 4.Della Chiesa M, Vitale M, Carlomagno S, Ferlazzo G, Moretta L, Moretta A. The natural killer cell-mediated killing of autologous dendritic cells is confined to a cell subset expressing CD94/NKG2A, but lacking inhibitory killer Ig-like receptors. Eur J Immunol. 2003;33:1657–1666. doi: 10.1002/eji.200323986. [DOI] [PubMed] [Google Scholar]
- 5.Bielekova B, Catalfamo M, Reichert-Scrivner S, Packer A, Cerna M, Waldmann TA, McFarland H, Henkart PA, Martin R. Regulatory CD56bright natural killer cells mediate immunomodulatory effects of IL-2R{alpha}-targeted therapy (daclizumab) in multiple sclerosis. PNAS. 2006;103:5941–5946. doi: 10.1073/pnas.0601335103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benczur M, Petranyl GG, Palffy G, Varga M, Talas M, Kotsy B, Foldes I, Hollan SR. Dysfunction of natural killer cells in multiple sclerosis: a possible pathogenetic factor. Clin Exp Immunol. 1980;39:657–662. [PMC free article] [PubMed] [Google Scholar]
- 7.Kastrukoff LF, Lau A, Wee R, Zecchini D, White R, Paty DW. Clinical relapses of multiple sclerosis are associated with ‘novel’ valleys in natural killer cell functional activity. J Neuroimmunol. 2003;145:103–114. doi: 10.1016/j.jneuroim.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 8.Zhang B, Yamamura T, Kondo T, Fujiwara M, Tabira T. Regulation of experimental autoimmune encephalomyelitis by natural killer (NK) cells. J Exp Med. 1997;186:1677–1687. doi: 10.1084/jem.186.10.1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Segal BM. The role of natural killer cells in curbing neuroinflammation. J Neuroimmunol. 2007;191:2–7. doi: 10.1016/j.jneuroim.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi FD, Van Kaer L. Reciprocal regulation between natural killer cells and autoreactive T cells. Nat Rev Immunol. 2006;6:751–760. doi: 10.1038/nri1935. [DOI] [PubMed] [Google Scholar]
- 11.Hafler DA, Compston A, Sawcer S, Lander ES, Daly MJ, De Jager PL, de Bakker PI, Gabriel SB, Mirel DB, Ivinson AJ, Pericak-Vance MA, Gregory SG, Rioux JD, McCauley JL, Haines JL, Barcellos LF, Cree B, Oksenberg JR, Hauser SL. Risk alleles for multiple sclerosis identified by a genomewide study. N Engl J Med. 2007;357:851–862. doi: 10.1056/NEJMoa073493. [DOI] [PubMed] [Google Scholar]
- 12.Wang X, Rickert M, Garcia KC. Structure of the quaternary complex of interleukin-2 with its alpha, beta, and gammac receptors. Science. 2005;310:1159–1163. doi: 10.1126/science.1117893. [DOI] [PubMed] [Google Scholar]
- 13.Waldmann TA. The IL-2/IL-15 receptor systems: targets for immunotherapy. J Clin Immunol. 2002;22:51–56. doi: 10.1023/a:1014416616687. [DOI] [PubMed] [Google Scholar]
- 14.Nussenblatt RB, Fortin E, Schiffman R, Rizzo L, Smith J, Van Veldhuisen P, Sran P, Yaffe A, Goldman CK, Waldmann TA, Whitcup SM. Treatment of noninfectious intermediate and posterior uveitis with the humanized anti-Tac mAb: a phase I/II clinical trial. Proc Natl Acad Sci U S A. 1999;96:7462–7466. doi: 10.1073/pnas.96.13.7462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bielekova B, Richert N, Howard T, Blevins G, Markovic-Plese S, McCartin J, Wurfel J, Ohayon J, Waldmann TA, McFarland HF, Martin R. Humanized anti-CD25 (daclizumab) inhibits disease activity in multiple sclerosis patients failing to respond to interferon {beta} Proc Natl Acad Sci U S A. 2004;101:8705–8708. doi: 10.1073/pnas.0402653101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rose JW, Watt HE, White AT, Carlson NG. Treatment of multiple sclerosis with an anti-interleukin-2 receptor monoclonal antibody. Ann Neurol. 2004;56:864–867. doi: 10.1002/ana.20287. [DOI] [PubMed] [Google Scholar]
- 17.Bielekova B, Howard T, Packer AN, Richert N, Blevins G, Ohayon J, Waldmann TA, McFarland HF, Martin R. Effect of anti-CD25 antibody daclizumab in the inhibition of inflammation and stabilization of disease progression in multiple sclerosis. Arch Neurol. 2009;66:483–489. doi: 10.1001/archneurol.2009.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rose JW, Burns JB, Bjorklund J, Klein J, Watt HE, Carlson NG. Daclizumab phase II trial in relapsing and remitting multiple sclerosis: MRI and clinical results. Neurology. 2007;69:785–789. doi: 10.1212/01.wnl.0000267662.41734.1f. [DOI] [PubMed] [Google Scholar]
- 19.Fehniger TA, Bluman EM, Porter MM, Mrozek E, Cooper MA, VanDeusen JB, Frankel SR, Stock W, Caligiuri MA. Potential mechanisms of human natural killer cell expansion in vivo during low-dose IL-2 therapy. J Clin Invest. 2000;106:117–124. doi: 10.1172/JCI6218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oh U, Blevins G, Griffith C, Richert N, Maric D, Lee CR, McFarland H, Jacobson S. Regulatory T cells are reduced during anti-CD25 antibody treatment of multiple sclerosis. Arch Neurol. 2009;66:471–479. doi: 10.1001/archneurol.2009.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Setoguchi R, Hori S, Takahashi T, Sakaguchi S. Homeostatic maintenance of natural Foxp3+ CD25+ CD4+ regulatory T cells by interleukin (IL)-2 and induction of autoimmune disease by IL-2 neutralization. J Exp Med. 2005;201:723–735. doi: 10.1084/jem.20041982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perez OD, Nolan GP. Phospho-proteomic immune analysis by flow cytometry: from mechanism to translational medicine at the single-cell level. Immunol Rev. 2006;210:208–228. doi: 10.1111/j.0105-2896.2006.00364.x. [DOI] [PubMed] [Google Scholar]
- 23.Alter G, Malenfant JM, Altfeld M. CD107a as a functional marker for the identification of natural killer cell activity. Journal of immunological methods. 2004;294:15–22. doi: 10.1016/j.jim.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 24.Bayer AL, Lee JY, de la Barrera A, Surh CD, Malek TR. A function for IL-7R for CD4+CD25+Foxp3+ T regulatory cells. J Immunol. 2008;181:225–234. doi: 10.4049/jimmunol.181.1.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michel L, Berthelot L, Pettre S, Wiertlewski S, Lefrere F, Braudeau C, Brouard S, Soulillou JP, Laplaud DA. Patients with relapsing-remitting multiple sclerosis have normal Treg function when cells expressing IL-7 receptor alpha-chain are excluded from the analysis. J Clin Invest. 2008 doi: 10.1172/JCI35365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huntington ND, Legrand N, Alves NL, Jaron B, Weijer K, Plet A, Corcuff E, Mortier E, Jacques Y, Spits H, Di Santo JP. IL-15 trans-presentation promotes human NK cell development and differentiation in vivo. J Exp Med. 2009;206:25–34. doi: 10.1084/jem.20082013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saraste M, Irjala H, Airas L. Expansion of CD56Bright natural killer cells in the peripheral blood of multiple sclerosis patients treated with interferon-beta. Neurol Sci. 2007;28:121–126. doi: 10.1007/s10072-007-0803-3. [DOI] [PubMed] [Google Scholar]
- 28.Smyth CM, Ginn SL, Deakin CT, Logan GJ, Alexander IE. Limiting {gamma}c expression differentially affects signaling via the interleukin (IL)-7 and IL-15 receptors. Blood. 2007;110:91–98. doi: 10.1182/blood-2006-11-055442. [DOI] [PubMed] [Google Scholar]
- 29.Xue HH, Kovanen PE, Pise-Masison CA, Berg M, Radovich MF, Brady JN, Leonard WJ. IL-2 negatively regulates IL-7 receptor alpha chain expression in activated T lymphocytes. Proc Natl Acad Sci U S A. 2002;99:13759–13764. doi: 10.1073/pnas.212214999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wuest TY, Willette-Brown J, Durum SK, Hurwitz AA. The influence of IL-2 family cytokines on activation and function of naturally occurring regulatory T cells. J Leukoc Biol. 2008;84:973–980. doi: 10.1189/jlb.1107778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Joffre O, Nolte MA, Sporri R, Reis e Sousa C. Inflammatory signals in dendritic cell activation and the induction of adaptive immunity. Immunol Rev. 2009;227:234–247. doi: 10.1111/j.1600-065X.2008.00718.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.