Abstract
Background
Functional limitations have been operationally defined for studies of rehabilitation science through measures of physical performance and patient-reported function. Although conceived as representing similar concepts, differences between these 2 modes of measuring physical functioning have not been adequately characterized scientifically.
Objective
The purpose of this study was to compare the Short Physical Performance Battery (SPPB) with the function component of the Late-Life Function and Disability Instrument (LLFDI) with respect to their association with physiologic factors and other psychosocial and health factors potentially influencing rehabilitative care.
Design
This study was a cross-sectional analysis of baseline data from a sample of community-dwelling older adults (N=137) with mobility limitations enrolled in a randomized controlled trial of exercise.
Methods
A performance-based measure of function (the SPPB) and a self-report measure of function (the LLFDI) served as functional outcomes. Physiologic factors included measures of leg strength, leg velocity, and exercise tolerance test (ETT) duration, which served as a surrogate measure of aerobic capacity. Psychosocial and health factors included age, sex, height, body mass index, number of chronic conditions, depression, and falls efficacy.
Results
Separate multivariable regression models predicting SPPB and LLFDI scores described 33% and 42% of the variance in each outcome (R2), respectively. Leg velocity and ETT duration were positively associated with both performance-based and patient-reported functional measures. Leg strength and age were positively associated with SPPB scores, whereas number of chronic conditions, sex, and falls efficacy were associated with the LLFDI scores.
Limitations
This study included older adults with mobility limitations and may not generalize to other populations.
Conclusions
Performance-based and patient-reported measures of physical function appear to assess different aspects of an older person's functioning. The SPPB was associated with age and physiologic factors, whereas patient-reported function measured by the LLFDI was associated with these factors as well as with psychosocial and health factors.
Functional limitations measured through standardized observation of physical performance or patient-reported function have been recognized as important rehabilitation outcomes as well as a potentially important means of identifying individuals at risk for disability.1 For this reason, screening adults for functional limitation has been advocated as a geriatric “vital sign,” useful in many clinical settings.2 What is less clear is when one should use performance-based measures of function that can be highly standardized to provide a measure of a person's functional capacity in contrast to patient-reported measures of function, which can cover a much broader array of functions relevant to a person's daily life. The Short Physical Performance Battery (SPPB) and the Late-Life Function and Disability Instrument (LLFDI) both represent measures of physical function that are advocated for use among older adults.3 Comparisons between the 2 measures have been drawn for the purpose of establishing validity and highlighting their similarities.4 They are different, however, in that the SPPB is a measure of observed physical performance, whereas the LLFDI is a patient-report measure. Observed and self-report measures have been compared with each other with respect to their psychometric properties and ability to predict disability,5 but to our knowledge no study has compared these 2 types of functional measures with respect to the types of physiologic and psychosocial factors that may be associated with each measure.
When screening patients deemed at risk for disability, rehabilitation clinicians focus on those physiologic attributes that, when insufficient, manifest as impairments and are most responsible for limitations in physical function or disability. Optimal rehabilitative care addresses these impairments while simultaneously taking into account other psychosocial and physical factors that may influence an individual's functional status and future prognosis. Because the manifestation of impairments may vary among individuals with mobility problems, an ideal mobility screening tool would be associated with a wide variety of impairments, while not being overly influenced by the presence of any single impairment. Impairments relevant to mobility include such attributes as strength, velocity of movement, and aerobic capacity.6 Although these impairments have previously been evaluated separately in relation to the SPPB,7–9 their association with measures of patient-reported function such as the LLFDI has not been adequately explored.
To better understand the potential implications of using performance-based versus patient-report measures of function in rehabilitative care, we investigated what physiologic factors were most associated with SPPB scores and scaled scores on the function component of the LLFDI. Using baseline data from a sample of older adults with mobility limitations who had enrolled in a randomized controlled trial, we hypothesized that similar physiologic factors would be associated with function as measured by the SPPB and the LLFDI, but that patient-reported function (using the LLFDI) also would be associated with psychosocial and health factors such as self-efficacy.
Method
This study was a cross-sectional analysis of baseline data from a sample of older adults with limited mobility who were enrolled in a randomized controlled study of exercise.10
Conceptual Paradigm
For the purpose of this investigation, we evaluated disablement outcomes using the paradigm originally established by Nagi.11 In this paradigm: (1) impairments are defined as deficits at the level of the organ system (eg, muscle weakness), (2) functional limitations are defined as alterations in the performance of a functional task (eg, mobility performance), and (3) disability is defined as the inability of an individual to perform his or her social and environmental roles.10 This investigation specifically focused on attributes that, when deficient, can be targeted in rehabilitative care. For the purpose of this investigation, we have characterized these attributes as either physiologic factors or psychosocial and health factors.
Recruitment and Screening of Participants
Initially, 590 inquiries were elicited via advertising in newspapers, direct mailings, referrals from primary care providers, and telephone screenings. Of these, 260 people were identified as potentially eligible and attended an initial screening assessment at our facility. On completion of the initial screening, 92 people could not participate in the study due to exclusion criteria, and 30 people chose not to commit to the study, leaving 138 participants. Testing for the intervention study was completed over 1 to 2 subsequent visits depending on participant availability. Measures used for this analysis were all completed within the first 2 visits, which were scheduled within 1 week of each other. A total of 137 participants were included in this analysis because one participant did not complete all the baseline measurements.
Participants included in the study were community-dwelling older adults (age ≥65 years) with SPPB scores between 4 and 10 on the initial screening visit who were able to climb a flight of stairs independently or using a device such as a cane. Exclusion criteria were unstable acute or chronic disease, a score of <23 on the Folstein Mini-Mental State Examination,12 a neuromusculoskeletal impairment (eg, severe osteoarthritis, hip replacement with recurrent dislocation) limiting participation in further testing, or an exercise tolerance test with positive findings for symptomatic cardiovascular disease.
After providing informed consent, participants underwent a comprehensive history and physical examination that was conducted by the principal investigator (J.F.B.). At the completion of the physical examination, we recorded the total number of medical conditions defined as either: (1) a condition for which a participant was actively receiving treatment or (2) a condition requiring medical treatment within the previous year. Medical records were requested from participants' primary care physicians to corroborate these findings. A subsequent evaluation was conducted within 1 to 2 weeks, at which time the SPPB was repeated, leg strength and leg velocity were evaluated, and the LLFDI was administered.
Physiologic Factors
Leg strength and leg velocity were measured with a pneumatic double leg press resistance machine using reliable and valid methods.13 Strength refers to the maximum force production of the muscle group tested. Leg power is defined as the product of leg force and leg velocity. Leg velocity is the attribute that distinguishes leg strength from leg power. In order to be able to distinguish the unique contributions of these 2 attributes, they were evaluated as separate factors. Briefly, the 1-repetition maximum (1-RM) was determined by progressively increasing the resistance for successive repetitions until the participant could no longer move the lever arm one time through the full range of motion. Peak leg power was measured as the best of 5 repetitions performed at 40% of the 1-RM, during which participants performed the concentric action of one repetition as quickly as possible. Leg velocity was obtained by dividing the peak leg power by leg strength and normalizing for an individual's weight in kilograms as previously described.14
Participants underwent exercise tolerance testing on a treadmill. For safety purposes, they were required to hold on to the treadmill support bar with at least one arm at all times. All exercise stages were 3 minutes in duration. The first 3 stages were tested at the participant's habitual gait speed at 0%, 5%, and 10% grades of inclination, respectively. Thereafter, treadmill speed was increased by 25% at 12% grade, increasing the grade by 2% increments in each subsequent stage until test termination. At the end of each stage, blood pressure was recorded, and perceived exertion was measured using the Borg Scale.15 Testing was terminated when a participant had achieved a Borg Scale rating of 17 or greater.15 Testing was stopped prior to this point of time if a participant experienced significant fatigue or any adverse symptoms during the test. Aerobic capacity was operationally defined as the measured duration of the exercise tolerance test in minutes.
Functional Outcome Measures
The SPPB is a well-established, reliable, and valid measure of functional performance.16,17 Testing involves an assessment of standing balance, the timed 4-m walk test, and the timed test of 5 repetitions of rising from a chair and sitting down. All times are measured to the nearest 0.01 second using a stopwatch. Each of the 3 aforementioned tests is scored between 0 and 4 and summed (maximum score=12), with higher scores representing better functioning. Scores on the SPPB have been found to predict disability over 1 to 6 years in several older populations.16,17 Testing was completed over a subsequent visit, at which point a second SPPB was performed. Although the initial SPPB was the test that determined eligibility, some participants scored differently on the subsequent SPPB test. Therefore, the average of the 2 SPPB scores was used in this analysis.
The LLFDI4,18,19 function component assesses patient-reported difficulty in performing 32 functional tasks covering a wide variety of life tasks, including: personal maintenance, mobility and travel, exchange of information, social, community and civic activities, home life, paid or volunteer work, and involvement in economic activities (Appendix). The LLFDI also assesses 2 disability domains addressing the frequency of performing life tasks and the limitation in an individual's capacity to perform those tasks. Raw scores for the function domain are transformed to scaled scores, based on a single-parameter Rasch model to allow each domain score to be on a similar metric and easier to interpret. Participants were scored on a transformed scale of 1 to 100, where higher numbers denoted higher levels of function.19 Based upon the aims of our investigation, we evaluated only the function component of the LLFDI.
Psychosocial and Health Factors
From among the available measures, potential psychosocial and health variables were selected based upon the previous literature and their clinical association with the predictors and outcomes. They included: age, sex, height, body mass index (BMI), number of chronic conditions, depression as manifested by a Center for Epidemiological Studies Depression Scale (CES-D) score of ≥16,20 and falls efficacy as measured by the Falls Efficacy Scale.21,22 A falls efficacy score of ≥20 is considered clinically worse.21,22 Height and weight were measured during the initial physical examination using a calibrated scale and stadiometer. Body mass index was calculated by the formula: mass (kg)/height (m)2. Body mass status was characterized using standard National Heart Lung and Blood Institute cutpoints23: normal=BMI <25 kg/m2, overweight=BMI ≥25 kg/m2 to <30 kg/m2, and obese=BMI ≥30 kg/m2.
Data Analysis
Descriptive statistics were calculated, including frequency and proportions for categorical variables and means and standard deviations for continuous variables. The correlations among the respective outcomes were examined. We created separate multivariable regression models predicting the SPPB total score and the scaled score on the LLFDI function component using an analytic approach advocated by Sun et al.24 This approach overcomes weaknesses of relying solely on bivariable selection or automated procedures. We included all psychosocial and health factors and physiologic factors in a stepwise backward regression model using a criterion of P=.10 for model inclusion. Then, each eliminated variable was manually reintroduced into the model, including those that were suspected of collinearity on the basis of prior literature, clinical experience, and statistical criteria (change in standard error ≥20%).25 Final statistical significance was determined using an alpha level of .05. A partial R2 value was calculated for each independent variable. We did not include any balance measure in our primary analyses. We felt that it might confound our findings for 2 reasons. First, the SPPB includes balance as a component of its total score and would be overly sensitive to the influence of a balance measure. Second, both leg strength and leg velocity have been shown to be associated with balance performance,25 and thus their influence on the outcomes might be mitigated by including a balance measure in the multivariable models. All analyses were conducted using SAS/STAT software, version 9.0 (SAS Institute Inc, Cary, North Carolina).26
Results
As shown in Table 1, the mean age of the participants was 75.3 years, 69% were female, and 64% were overweight or obese. They had an average of 5.5 chronic conditions, with 14% manifesting depression and 7% having a falls efficacy score of >20. They had a mean SPPB score of 8.7 out of 12 and a mean LLFDI function component score of 64.3. The correlation between the SPPB and LLFDI function component scores was r=.34 (P<.001).
Table 1.
Baseline Characteristics of Sample of Community-Dwelling Older Adults With Mobility Limitations (N=137)a
BMI=body mass index, CES-D=Center for Epidemiological Studies Depression Scale, SPPB=Short Physical Performance Battery, ETT=exercise tolerance test, LLFDI=Late-Life Function and Disability Instrument, N/A=not applicable.
b Higher score reflects worse falls efficacy.
c Higher score reflects better performance.
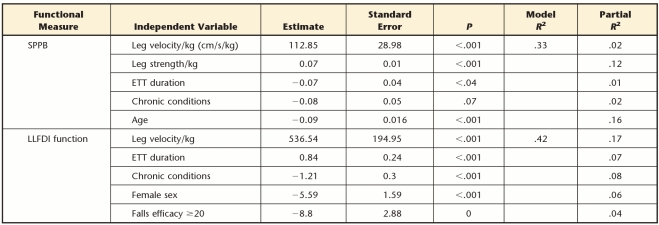
The multivariable models predicting performance on both the SPPB and the LLFDI function component were statistically significant (P<.001), describing 33% and 42% of the variance (R2), respectively. With respect to the SPPB, leg velocity, leg strength, and exercise tolerance test (ETT) duration were all significantly associated, describing 2%, 12%, and 1%, of the variance (partial R2), respectively. Age was an additional factor associated with SPPB performance, describing 16% of the variance. The number of chronic illnesses was a psychosocial and health variable in the final model, but did not achieve statistical significance. In the model predicting LLFDI function, leg velocity and aerobic capacity were positively associated, having partial R2 values of .17 and .07, respectively. Additionally, chronic conditions (partial R2=.08), female sex (partial R2=.06), and falls efficacy (partial R2=.04) accounted for 18% of the variance. Strength was not a factor significantly associated with LLFDI function. (Tab. 2)
Table 2.
Final Multivariable Linear Regression Models Predicting Functional Capacity as Measured by the Short Physical Performance Battery (SPPB) and the Function Component of the Late-Life Function and Disability Instrument (LLFDI), Presenting Independent Variables With Partial R2≥.02a
Higher score reflects better performance. Both models, P<.001. ETT=exercise tolerance test.
Discussion
Our study of older adults with mobility limitations revealed that performance-based and patient-report measures of function were not strongly related to each other and that important differences between the SPPB and the LLFDI were observed with respect to the attributes associated with each measure. In this study, the impairments of leg strength, leg velocity, and ETT duration, along with age, were associated with our performance-based function. In contrast, a much broader array of attributes (leg velocity, aerobic capacity, the number of chronic conditions, sex, and falls efficacy) were associated with patient-reported function.
These similarities and differences have a variety of implications. As opposed to a comparison of psychometric qualities of the outcomes, our investigation contributes to the literature by providing empirical evidence suggesting that these 2 measures of function do not provide equivalent information about a patient's functional status. This finding may have important implications as to the settings or situations in which one may choose to use the SPPB versus the LLFDI. If, for example, an intervention was being evaluated that emphasized strength and velocity of movement among older adults, a strong case could be made that the SPPB would be an exceptionally good outcome measure. In contrast, if a more comprehensive intervention were under investigation involving a patient's aerobic capacity, disease burden, or self-efficacy, the LLFDI may be a more suitable functional outcome tool. In contrast, this decision may be even more relevant if balance training were a component of an intervention, given that balance is a measured component of the SPPB and might overstate the benefits of the balance intervention on physical function in general. Another difference between the 2 measures is the duration of testing. In settings that are more constrained for time, the SPPB, being the quicker of the 2 measures to administer, may be more convenient. However, this time concern may be mitigated in the future, as computer-adapted versions of the LLFDI are being developed.27 Lastly, it is important to note that the SPPB includes items addressing functional tasks that primarily depend upon the lower limbs, whereas the LLFDI includes tasks that place demands on both the upper and lower limbs. Not only might these differences affect outcome choice, but they may account, in part, for our observed differences.
Leg strength and leg velocity together described 14% of the variance in SPPB performance. This finding is consistent with a previous investigation of the InCHIANTI data set, which evaluated leg power and the combination of leg strength and leg power. In that analysis, it was observed that in a multivariable linear regression model, leg power described 28% of the variance in SPPB performance.5 A relationship between the LLFDI and measures of leg strength and leg power also has been reported by Puthoff and Nielsen8 for a smaller sample of older adults with a higher level of functioning. It is interesting to note that ETT duration described only 1% of the variance in SPPB scores and 7% of the variance in LLFDI function component scores. The function component of the LLFDI does include a much broader range of tasks (Appendix), and a number of these items may be more dependent upon an individual's aerobic capacity than the relatively short-duration components of the SPPB. The absence of an association of strength with LLFDI function is somewhat surprising. It contrasts with the findings of previous studies with smaller samples8 and should be confirmed in subsequent investigations.
It is worthwhile to emphasize that leg velocity was a significant predictor of both performance-based and patient-report measures of functioning. We do not view these findings as an indication to de-emphasize the importance of strength in clinical care. Rather, although leg strength is commonly prioritized in rehabilitative care for mobility problems, clinical experience suggests that leg velocity is rarely emphasized.7 Our findings add to the growing evidence that enhancement of leg velocity may be important for optimizing mobility status.10
Body mass index was not associated with either measure. This finding is in contrast to the study by McAuley et al,28 who found that BMI was associated with LLFDI function in older women. In their study, however, McAuley and colleagues did not evaluate the influence of physiologic attributes such as strength and power, which likely mediate the influence of BMI on LLFDI function. This conclusion is supported by a previous report evaluating physiologic attributes and health factors that predict high SPPB performance in the InVEST study.7
Patient-reported function also is influenced by other factors such as number of chronic illnesses and falls efficacy. Self-efficacy is recognized as an important factor mediating disablement outcomes, and its association with the LLFDI is confirmed by recent reports.29,30 Our findings suggest that the LLFDI may allow for a broader functional measure, which is representative of not only physical attributes, but also health and psychosocial factors.
The significant influence of self-efficacy on patient-reported function and not on the SPPB also may represent inherent differences between self-report, a more subjective process, and observed performance.30 These concepts were considered by Fried and colleagues5 when they attempted to explain the relevance of task modification as a differentiating factor between self-report function and observed performance. They defined task modification as a patient reporting modification in performing a selected task due to underlying health problems. They highlighted task modification as an intermediate step between the manifestation of impairments and disability and concluded that this attribute is best obtained via self-report.5,31 It is likely that self-efficacy is very influential on whether a person chooses to modify or avoid a given task. The relationship among self-efficacy, task modification. and the rehabilitation process is clearly worthy of future investigation, as has been recently emphasized.32 In a recent review on this topic that recognized the inherent differences between performance-based and self-report measures, it was emphasized that studies should use combinations of both outcomes.3 Our findings reinforce this conclusion.
Our study did have limitations. We conducted an investigation among elderly volunteers with mobility limitations who were participating in a randomized controlled trial of exercise, and our findings may not generalize to other populations. Additionally, our investigation was limited in scope and did not broadly evaluate cognitive and behavioral factors that are theorized to influence measures of functional limitation.33 It should be recognized that the SPPB does not address nearly as broad a view of physical function as does the function domain of the LLFDI. Thus, direct comparisons might be challenging. However, both modes of measurement are considered measures of functional limitation, and both are advocated outcomes of this domain within geriatric clinical research.3
In summary, our investigation has broadened our understanding of the role of performance-based functional measurement versus patient-reported functioning as measured by the SPPB and the LLFDI, respectively. The SPPB is associated with leg strength and leg velocity, whereas patient-reported function as measured by the LLFDI may be more representative of not only important impairment domains but also psychosocial factors such as self-efficacy. These differences have direct relevance to clinicians and investigators considering the use of either measure. We believe that our thorough evaluation of impairments of interest to rehabilitation clinicians is unique, and our analysis with these 2 methods of measuring functioning augments the current literature. Future studies should consider these associations prospectively using a broader range of physical, cognitive, and behavioral factors among a population-based cohort.
Appendix.
Appendix.
Questions Included in the Function Component of the Late-Life Function and Disability Instrument
Footnotes
All authors participated in preparation of the manuscript. Dr Bean provided study concept. Dr Bean, Dr Ölveczky, and Dr Jette provided study design. Ms LaRose provided data collection. Dr Bean, Dr Ölveczky, Mr Kiely, and Dr Jette provided data analysis and interpretation. The authors acknowledge Evelyn O'Neill for her assistance with aspects of data collection and Mary Alice Hanford for her assistance with preparation of the manuscript.
Aspects of this investigation were presented at the American Geriatrics Society Annual Meeting; May 2007; Seattle, Washington.
Dr Bean was funded by Dennis W. Jahnigen Scholars Career Development Award from the American Geriatrics Society/Hartford Foundation, a NIH Mentored Clinical Scientist Development Award (K23AG019663–01A2), and the Department of Physical Medicine and Rehabilitation, Harvard Medical School. Dr Jette's work was supported, in part, by the Boston Claude D. Pepper Older Americans Independence Center (grant 5P30AG031679).
The clinical trial from which this analysis was obtained is registered (registration no. NCT00158119).
References
- 1. Morley JE. Mobility performance: a high-tech test for geriatricians. J Gerontol A Biol Sci Med Sci. 2003;58:712–714 [DOI] [PubMed] [Google Scholar]
- 2. Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322 [DOI] [PubMed] [Google Scholar]
- 3. Gill TM. Assessment of function and disability in longitudinal studies. J Am Geriatr Soc. 2010;58(suppl 2):S308–S312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sayers SP, Jette AM, Haley SM, et al. Validation of the Late-Life Function and Disability Instrument. J Am Geriatr Soc. 2004;52:1554–1559 [DOI] [PubMed] [Google Scholar]
- 5. Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. J Gerontol A Biol Sci Med Sci. 2000;55:M43–M52 [DOI] [PubMed] [Google Scholar]
- 6. Bean JF, Vora A, Frontera WR. Benefits of exercise for community-dwelling older adults. Arch Phys Med Rehabil. 2004;85(7 suppl 3):S31–S42 [DOI] [PubMed] [Google Scholar]
- 7. Bean JF, Kiely DK, LaRose S, Leveille SG. Which impairments are most associated with high mobility performance in older adults: implications for a rehabilitation prescription. Arch Phys Med Rehabil. 2008;89:2278–2284 [DOI] [PubMed] [Google Scholar]
- 8. Puthoff ML, Nielsen DH. Relationships among impairments in lower-extremity strength and power, functional limitations, and disability in older adults. Phys Ther. 2007;87:1334–1347 [DOI] [PubMed] [Google Scholar]
- 9. Ritchie DM, Sipe CL, Lyle RM. The Relationship between the Late-Life Function and Disability Instrument (LLFDI) and Berg Balance Scale (BBS): 2296: Board #209 June 1 9:00 AM–10:30 AM. Med Sci Sports Exerc. 2007;39(5 suppl):S419 [Google Scholar]
- 10. Bean JF, Kiely DK, LaRose S, et al. Increased velocity exercise specific to task training versus the National Institute on Aging's strength training program: changes in limb power and mobility. J Gerontol A Biol Sci Med Sci. 2009;64:983–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nagi S. Some conceptual issues in disability and rehabilitation. In: Sussman M, ed. Sociology and Rehabilitation. Washington DC: American Sociological Society; 1965:100 [Google Scholar]
- 12. Folstein MF, Folstein SF, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198 [DOI] [PubMed] [Google Scholar]
- 13. Callahan D, Phillips E, Carabello R, et al. Assessment of lower extremity muscle power in functionally-limited elders. Aging Clin Exp Res. 2007;19:194–199 [DOI] [PubMed] [Google Scholar]
- 14. Bean JF, Kiely DK, LaRose S, et al. Is stair climb power a clinically relevant measure of leg power impairments in at-risk older adults? Arch Phys Med Rehabil. 2007;88:604–609 [DOI] [PubMed] [Google Scholar]
- 15. Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2:92–98 [PubMed] [Google Scholar]
- 16. Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guralnik JM, Simonsick EM, Ferucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol A Biol Sci Med Sci. 1994;49:M85–M94 [DOI] [PubMed] [Google Scholar]
- 18. Dubuc N, Haley S, Ni P, et al. Function and disability in late life: comparison of the Late-Life Function and Disability Instrument to the Short-Form-36 and the London Handicap Scale. Disabil Rehabil. 2004;26:362–370 [DOI] [PubMed] [Google Scholar]
- 19. Haley SM, Jette AM, Coster WJ, et al. Late Life Function and Disability Instrument: II; development and evaluation of the function component. J Gerontol A Biol Sci Med Sci. 2002;57:M217–M222 [DOI] [PubMed] [Google Scholar]
- 20. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84 [PubMed] [Google Scholar]
- 21. Harada N, Chiu V, Damron-Rodriguez J, et al. Screening for balance and mobility impairment in elderly individuals living in residential care facilities. Phys Ther. 1995;75:462–469 [DOI] [PubMed] [Google Scholar]
- 22. Jorstad EC, Hauer K, Becker C, et al. Measuring the psychological outcomes of falling: a systematic review. J Am Geriatr Soc. 2005;53:501–510 [DOI] [PubMed] [Google Scholar]
- 23. Kuczmarski RJ, Flegal KM. Criteria for definition of overweight in transition: background and recommendations for the United States. Am J Clin Nutr. 2000;72:1074–1081 [DOI] [PubMed] [Google Scholar]
- 24. Sun GW, Shook TL, Kay GL. Inappropriate use of bivariable analysis to screen risk factors for use in multivariable analysis. J Clin Epidemiol. 1996;49:907–916 [DOI] [PubMed] [Google Scholar]
- 25. Mayson DJ, Kiely DK, LaRose SI, Bean JF. Leg strength or velocity of movement: which is more influential on the balance of mobility limited elders? Am J Phys Med Rehabil. 2008;87:969–976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. SAS Institute Inc SAS/STAT User's Guide, Version 9.0. Cary, NC: SAS Institute Inc; 2005 [Google Scholar]
- 27. Jette AM, Haley SM, Ni P, et al. Creating a computer adaptive test version of the late-life function and disability instrument. J Gerontol A Biol Sci Med Sci. 2008;63:1246–1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McAuley E, Konopack JF, Motl RW, et al. Measuring disability and function in older women: psychometric properties of the late-life function and disability instrument. J Gerontol A Biol Sci Med Sci. 2005;60:901–909 [DOI] [PubMed] [Google Scholar]
- 29. McAuley E, Konopack JF, Morris KS, et al. Physical activity and functional limitations in older women: influence of self-efficacy. J Gerontol B Psychol Sci Soc Sci. 2006;61:P270–P277 [DOI] [PubMed] [Google Scholar]
- 30. McAuley E, Morris KS, Doerksen SE, et al. Effects of change in physical activity on physical function limitations in older women: mediating roles of physical function performance and self-efficacy. J Am Geriatr Soc. 2007;55:1967–1973 [DOI] [PubMed] [Google Scholar]
- 31. Fried LP, Young Y, Rubin G, et al. Self-reported preclinical disability identifies older women with early declines in performance and early disease. J Clin Epidemiol. 2001;54:889–901 [DOI] [PubMed] [Google Scholar]
- 32. Weiss CO, Hoenig HM, Fried LP. Compensatory strategies used by older adults facing mobility disability. Arch Phys Med Rehabil. 2007;88:1217–1220 [DOI] [PubMed] [Google Scholar]
- 33. Keysor JJ, Jette AM. Have we oversold the benefit of late-life exercise? J Gerontol A Biol Sci Med Sci. 2001;56:M412–M423 [DOI] [PubMed] [Google Scholar]