Abstract
Parkinson's disease (PD) is a common disorder, and the diagnosis of Parkinson's disease is clinical and relies on the presence of characteristic motor symptoms. The accuracy of the clinical diagnosis of PD is still limited. Functional neuroimaging using SPECT technique is helpful in patients with first signs of parkinsonism. The changes detected may reflect the disease process itself and/or compensatory responses to the disease, or they may arise in association with disease- and/or treatment-related complications. This paper addresses the value of SPECT in early differential diagnosis of PD and its potential as a sensitive tool to assess the pathophysiology and progression, as well as the therapeutic efficacy of PD.
1. Introduction
PD is a common neurodegenerative disorder characterized by the motor features of rigidity, tremors, akinesia, and changes in speech and gait which are associated with the loss of dopaminergic neurons in the substantia nigra pars compacta and the subsequent deficiency in striatal dopaminergic system. It has prevalence of 1-2 per 1,000 among the general population and of up to 2% among people aged over 65 years. Parkinson's causes are unknown but genetics, aging, and toxins are being researched. The pathophysiological hallmark of PD is a slow, progressive degeneration of the nigrostriatal dopaminergic system. The widely accepted subcellular factor which underlies PD neuropathology is the presence of Lewy bodies [1] with characteristic inclusions of aggregated alpha-synuclein [2–4]. A recent study revealed that PD specific brain pathology extends far beyond the nigrostriatal dopaminergic system and affects widespread brain areas, including the olfactory system, autonomic and gain setting brainstem nuclei, and the cerebral cortex [5]. Physiological imaging techniques such as positron emission tomography (PET) or SPECT provide the means for detecting in vivo metabolic and neurochemical changes of PD.
Motor symptoms such as tremor at rest, akinesia, rigidity, and postural instability are the cardinal signs in PD [6]. The type and severity of symptoms experienced by a person with PD vary with each individual and the stage of the disease. PD is the most common cause of parkinsonism. There are also many nonmotor features of PD including behavioral and psychiatric problems such as dementia [7], fatigue [8], anxiety [9] and depression [10], autonomic dysfunction [11], addiction and compulsion [12], psychosis [13], olfactory dysfunction [14], and cognitive impairment [10]. These clinical features also occur in other neurodegenerative diseases and by dopamine receptor antagonist drugs, which means that with this main clinical application it is hard to diagnose patients with mild, incomplete, or uncertain parkinsonism [15]. The United Kingdom Parkinson's Disease Society Brain Bank clinical diagnostic criteria can improve diagnostic accuracy [16]; still, the diagnosis and management of PD can be a challenge.
The diagnosis of PD is based on clinical criteria, but misdiagnosis is as high as 25% of cases as confirmed by anatomic-pathologic studies. Because the diagnosis of PD is entirely clinical, the diagnosis and treatment may be delayed for years until functional disability occurs. SPECT is an aid that can help diagnosing the disease earlier.
2. Imaging Agent of SPECT for PD
The ligands used for SPECT belong to a group of compounds derived from cocaine that bind to the dopamine transporter and include IPT, TRODAT-1, and FP-CIT tagged with either iodine-123 (T1/2 = 13.2 h) or technetium-99 m (T1/2 = 6 h) radioisotopes. Tracers used for SPECT imaging of PD patients are presented in Table 1.
Table 1.
The tracer used for SPECT in Parkinson's disease.
| Biological variable | Radiotracer |
|---|---|
| Dopamine reuptake (dopamine transport) |
123I-β-CIT, 123I-FP-β-CIT, 123I-IPT (presynaptic dopamine transporter), 123I-Altropane, 123I-β-PE2I 99Tcm-TRODAT-1 |
|
| |
| D2 dopamine receptor |
123I-Iodospiperone, 123I-Iodobenzamide (123I-IBZM), (postsynaptic dopamine D2 receptor) 123I-Iodolisuride, 123I-IBF, 123I-Epidepride (extrastriatal DA receptors) |
Specific SPECT ligands for DAT (FP-CIT, beta-CIT, IPT, TRODAT-1) imaging provide a marker for presynaptic neuronal degeneration [17]. Postsynaptic receptor density is explored with dopamine receptor ligands, notably of the D2 type [18].
Unlike PET, there is no need for an on-site cyclotron or for radiochemistry facilities due to a longer half-life. SPECT studies have the advantage of using an industrial production of tracers. The reduced cost of radiotracer synthesis permits the investigation of a larger number of patients by SPECT than by PET.
123I-β-CIT —
123I-β-CIT is a radiotracer which binds with nanomolar affinity to the serotonin transporter. It has a protracted period of striatal uptake enabling imaging 14–24 hours after injection for stable quantitative measures of dopamine transporters [19].
123I-FP-CIT —
123I-FP-CIT is an analogue of 123I-β-CIT. It has been shown to achieve peak tracer uptake in the brain within hours after injection and to provide greater selectivity for the dopamine transporter. 123I-FP-CIT washed out from striatal tissue is 15–20 times faster than that of 123I-β-CIT [19]. A clear decline in 123I-FP-CIT binding was found with aging, amounting to 9.6%/decade in the control group [20].
123I-IPT —
123I-IPT is a new cocaine analogue which allows the presynaptic dopamine transporters to be imaged with SPECT as early as 1-2 h after injection [21].
125I/123I-PE21 —
PE2I, a cocaine derivative, has good affinity for the DAT. 125I-PE2I has revealed very intense and selective binding in the basal ganglia [22]. It is a highly potent inhibitor of cloned DAT compared with GBR 12935 and provided a useful tool for further investigations in cells transfected with cDNA encoding the DAT [23]. PE2I is a relatively new radioligand that has about 10-fold higher in vitro selectivity for the DAT than for the serotonin transporter (SERT) compared to 123I-FP-CIT [24]. Further, 123I-PE2I has faster kinetics than 123I-FP-CIT. It is currently to be considered the best radioligand for imaging the DAT in the human brain with SPECT.
99Tcm-TRODAT-1 —
99Tcm-TRODAT-1 is a recently developed radiotracer that selectively binds to the dopamine transporters, which are significant because loss of these transporters corresponds with a loss of dopaminergic neurons. It is a potential agent for DAT SPECT [25].
123I-IBZM —
123I-IBZM is a central nervous system (CNS) D-2 dopamine receptor imaging agent, and it has a high concentration in basal ganglia of brain [26].
123I-IBF —
123I-IBF is an IBZM analogue. This agent concentrated in the striatum region and displayed a remarkably high target-to-nontarget ratio [27] and early time of peak uptake [28]. A study using P450 gene expression systems indicates that 123I-IBF is enzymatically metabolized in the liver and rapidly excreted in the urine [29]. It is a potential agent for imaging D-2 dopamine receptors [30].
3. The Use of SPECT Molecular Imaging in PD
3.1. The Course and the Pathogenesis of PD
Brain SPECT imaging of DAT with specific radioligands provides a useful tool of in vivo investigation of the pathogenesis of PD, and it is a sensitive method for examining the integrity of the presynaptic dopaminergic system [15]. Cerebral and extracranial Lewy-body-type degeneration in PD does not develops independently from each other but develop in a strongly coupled manner. The cerebral and extracranial changes are driven by at least similar pathomechanisms [31]. Patients with PD have markedly reduced DAT levels in striatum, which correlated with disease severity and disease progression [32], whereas postsynaptic striatal D2 receptors are upregulated [33]. Similarly, another study reported that the mean 123I-IBZM striatal-occipital ratio of binding was significantly higher in PD patients than in controls. In PD patients, higher values were found contralateral to the clinically most affected side, suggesting D2 receptor upregulation and the reverse was seen using 123I-FP-CIT SPECT [34]. Dual isotope imaging using 99Tcm-TRODAT-1 and 123I-IBZM is also a useful means in evaluating the changes of both pre- and postsynaptic dopamine system in a primate model of parkinsonism [35].
There was a significant association of visually analyzed shapes of the striatum in FP-CIT SPECT and clinical PD subtype. It suggested that factors other than nigrostriatal degeneration may contribute to disease severity [36]. One study including 122 patients confirmed neuropathological models for reduced dopaminergic projection to the dorsal putamen in akinetic-rigid patients as well as the lateral putamen and caudate nucleus in tremor-dominant patients in vivo [37], and the serotonergic system is suggested to be implicated in PD [38]. Furthermore, another study showed that SERT-dependent 123I-FP-CIT uptake may allow a more comprehensive assessment of neurochemical disturbances in degenerative parkinsonisms [39]; this study suggested that the neurodegenerative process extends beyond nigrostriatal system and affects serotoninergic neurons in parkinsonisms.
3.2. Early Diagnosis of PD
Since the in vivo molecular imaging techniques using SPECT have been introduced, the diagnosis of PD became more reliable by assessing dopaminergic and even nondopaminergic systems. SPECT is a very sensitive technique to detect nigrostriatal degeneration in PD. Various radiotracers have been used in the diagnosis of PD. DAT imaging is abnormal even in the earliest clinical presentation of PD [15]. A study using 123I-β-CIT found that the relative uptake reduction in the hemi-PD patients was greater in the putamen than in the caudate in patients with early PD and suggested that it may be useful in identifying individuals with developing dopaminergic pathology before onset of motor symptoms [40].
It was reported that 123I-β-CIT SPECT was 100% sensitive and specific for the diagnosis in younger patients (age <55 years). In older patients (age >55 years), specificity was substantially lower (68.5%) [41]. More recently, a prospective, longitudinal study using 123I-FP-CIT had investigated 99 patients with tremor and/or parkinsonism over 3 years, and the results showed a mean sensitivity of 78% and a specificity of 97% [42]. A 2-year followed-up SPECT study using 99Tcm-TRODAT-1 was performed in patients with clinically unclear Parkinsonian syndromes (CUPSs) and found that the rate of disagreement of SPECT in the patients was of 20%. The sensitivity of this technique was 100%, and specificity was 70%. It indicated that TRODAT-1 helps the diagnosis of patients with CUPS [43]. DAT SPECT is sensitive enough to detect a loss of nigrostriatal neurons in vivo even in preclinical phases of sporadic PD.
123I-FP-CIT SPECT has been successfully used to detect the loss of dopaminergic nigrostriatal neurons in Parkinson's disease at an early stage. But the results reported were controversial. Tissingh et al. reported that striatal 123I-FP-CIT uptake is markedly decreased in PD, more in the putamen than in the caudate nucleus, and the mean reduction in the putamen and caudate nucleus was 57% and 29% of the control mean, respectively. However, no significant correlations were found between striatal 123I-FP-CIT binding ratios and disease severity [20]. Spiegel et al. found that the striatal FP-CIT binding correlated significantly with the motor part of the unified Parkinson's disease rating scale (UPDRS) but not with age, disease duration, or gender [44]. Another study indicated that in patients with PD, the striatum, caudate, and putamen uptake was correlated with disease severity assessed by UPDRS and duration of disease [36]. More studies are needed to confirm these findings.
99Tcm-TRODAT-1 study including 29 patients with early PD and 38 healthy volunteers found that compared to controls, the uptake in caudate and anterior and posterior putamen values were significantly decreased in PD patients (Figure 1). Using the posterior putamen as the main region of interest resulted in the greatest accuracy sensitivity 79% and specificity 92% [45]. Patients with unilateral PD showed a bilateral loss of striatal DA transporters [46]. A study using semiquantitative 123I-FP-CIT SPECT detected a bilateral dopaminergic deficit in early PD with unilateral symptoms and preclinical DAT loss in the ipsilateral striatal binding, corresponding to the side not yet affected by motor signs. It suggested that semi-quantitative analysis may be used to diagnose PD at early stage as well as to identify individuals developing bilateral dopaminergic damage [47]. The decrease of striatal uptake contralateral to the more affected side of the body was more prominent compared to the ipsilateral side [48]. Moreover, another study showed a significant loss of putaminal uptake ipsilateral to the symptoms was found in the stage I group compared with the healthy volunteers [49]. The mean reduction of binding was found in the order of putamen and caudate nucleus.
Figure 1.
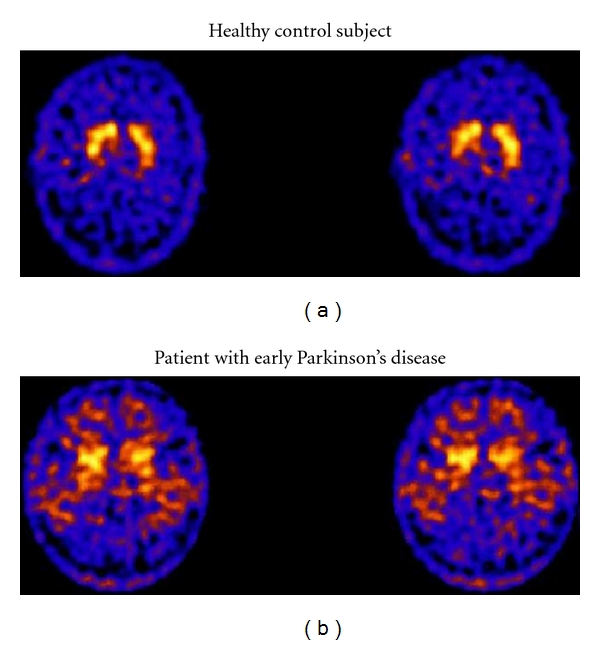
TRODAT-1 SPECT images of a healthy control (a) and a patient with early PD (b). The patient with early PD shows decreased TRODAT-1 uptake in the striatum compared to the control, particularly in the posterior putamen [45].
DAT imaging is a sensitive method to detect presynaptic dopamine neuronal dysfunction. Normal DAT-SPECT can be used to exclude underlying true nigrostriatal dysfunction [50].
SPECT also contributes to the assessment of the nonmotor symptoms of PD. MIBG was used in the diagnosis of damaged tissue of the heart. However, Sawada et al. [43] found that a reduction in MIBG cardiac accumulation reflects the systemic pathological process of the disease. Both early and delayed images showed that the heart to mediastinum ratios were significantly lower in the PD group than in the non-PD group [51].
Sakakibara et al. [52] first reported the correlation of urinary dysfunction with nigrostriatal dopaminergic deficit in PD, which was studied by 123I-β-CIT SPECT. The tracer uptake in patients with urinary dysfunction was significantly reduced than in those without urinary dysfunction
3.3. Differential Diagnosis of PD
Clinical features of PD may be shared with other disorders; thus, the differential diagnosis of PD is extensive. Idiopathic Parkinson's disease is associated with Lewy body degeneration of nigrostriatal dopaminergic neurons [53]. Atypical parkinsonian syndromes (APSs) such as multiple system atrophy (MSA), progressive supranuclear palsy (PSP), and corticobasal degeneration are characterized by poor response to antiparkinsonian medication and rapid clinical deterioration, which one often confused with PD. Other diseases, for example, drug-induced parkinsonism (DIP), essential tremor (ET), vascular parkinsonism (VP), or Dementia with Lewy bodies (DLBs) may also share common features with PD.
ET is a slowly progressive neurological disorder. DIP is developed when patients are treated with neuroleptic or dopamine receptor blocking agents. In most patients, Parkinsonism is reversible upon stopping the offending drug, though it may take several months to resolve fully but in some patients it may even persist. The differentiation between PD and DIP is difficult to assess on clinical grounds alone.
Functional imaging of the DAT defines integrity of the dopaminergic system, and a normal scan suggests an alternative diagnosis such as ET, VP (unless there is focal basal ganglia infarction), DIP, or psychogenic parkinsonism [17, 54]. Furthermore, a semiquantitative analysis with a cut-off of striatal asymmetry index greater than 14.08 could differentiate PD from VP with a 100% specificity [55]. 123I-FP-CIT SPECT images demonstrate that SPECT imaging with DAT ligands is useful to determine whether parkinsonism is entirely drug induced [56] and showed high levels of accuracy [57]. Cuberas-Borrós et al. performed FP-CIT images in 3 different groups of ET, DIP, and PD patients. Lower uptake was found in the PD group in comparison with the ET and DIP groups both in the putamen and in the caudate nucleus, but the differences between DIP and ET populations were only found in the putamen. There was an optimal discrimination threshold value between the reference population and the pathologic population for the putamen ratio by using volumes of interests, (VOIs) analysis [58].
SERT-dependent 123I-FP-CIT imaging showed a mild decrease in SERT levels in PD compared to ET and health control, and reduced to undetectable levels of SERT in PSP and DLB patients were displayed markedly [39]. To improve diagnostic accuracy, non-DAT tracers (i.e., D2 dopamine receptors) are necessary together with long-term clinical follow-up and rescans [59].
MSA is a neurodegenerative disorder characterized by neuropathologic demonstration of CNS alpha-synuclein-positive glial cytoplasmic inclusions with neurodegenerative changes in striatonigral or olivopontocerebellar structures [60]. Clinically, MSA is characterized by autonomic dysfunction and/or urinary dysfunction which may be associated with parkinsonian symptoms in 80% of patients (MSA-P) or with cerebellar ataxia in 20% of patients (MSA-C). It is difficult to differentiate it from other movement disorders, particularly in the early course of disease. Voxel wise analysis of 123I-β-CIT SPECT revealed more widespread decline of monoaminergic transporter availability in MSA-P compared with idiopathic Parkinson's disease (IPD) [61], matching the underlying pathological features. They suggest that the quantification of midbrain DAT signal should be included in the routine clinical analysis of 123I-β-CIT SPECT in patients with uncertain parkinsonism.
A combined 99mTc-ECD/123I-FP-CIT brain SPECT protocols have been proven to improve the differential diagnosis of IPD and MSA as well as corticobasal degeneration and PSP [62]. SPECT with the tracer 123I-Ioflupane can also give an accurate and highly sensitive measure of dopamine degeneration [63].
A study showed that the degree of loss was higher in putamen than caudate in both PD and MSA patients. However, MSA patients showed a more symmetric loss (ipsilateral versus contralateral side) of striatal DAT in both caudate and putamen than PD patients (Figure 2) [64]. It was also reported that patients with a side-to-side difference of reduced striatal 123I-β-CIT binding greater than 15% are likely to suffer from IPD, while the patients with the difference between 5% and 15% are more likely to have MSA [65]. Another study showed that mean distribution volume ratios (DVRs) in the basal ganglia of MSA patients were significantly less than in controls, but generally higher than in PD patients. Furthermore, the MSA patients had significantly increased DVRs in the posterior putamen (mean 0.49 ± 0.30) compared with PD patients (0.74 ± 0.25) [66].
Figure 2.
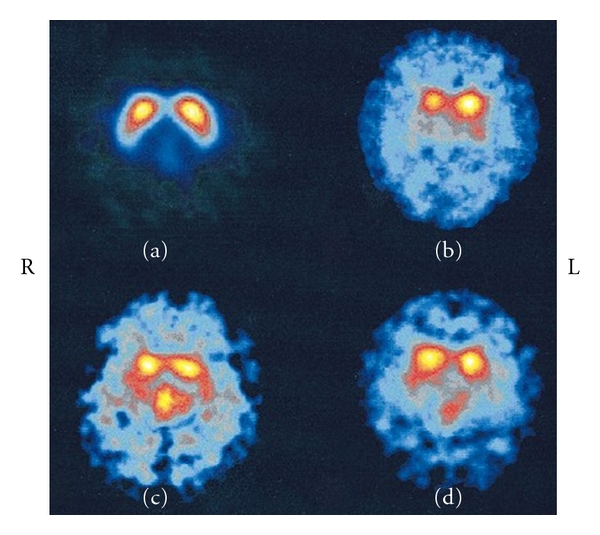
Transverse 123I-β-CIT images. (a) The image from a healthy control. (b) in PD patient the uptake is markedly reduced, with putamen more affected than caudate, and the right striatum (opposite to the side of more severe symptoms) showing the largest dopamine transporter (DAT) loss. (c) In MSA-striatonigral degeneration (MSA-SND) patient, the uptake is significantly reduced in both caudate and putamen and indicates more symmetric loss of DAT. (d) In the MSA-Shy-Drager syndrome (SDS) patient, the uptake is also significantly reduced, with putamen more affected than caudate; the loss of DAT appears to be symmetric [64].
Another study which used both 123I-β-CIT (for DAT) and 123I-IBF (for D2) reported that DAT binding in the posterior putamen was markedly reduced in all patients. However, D2 binding in posterior putamen was significantly increased in dopa-untreated PD, and it was significantly reduced in MSA. These findings suggested that DAT SPECT may be useful in differentiating parkinsonism from controls and D2 SPECT in further differentiating MSA from PD [67]. IBZM SPECT using recently introduced three dimensional automated quantification method calculating the Striatal/frontal cortex binding ratios [68] and voxel-by-voxel binding potential parametric imaging also can discriminate among extrapyramidal diseases such as PD and PSP [69].
123I-IBZM SPECT is an effective diagnostic tool in the establishment of the differential diagnosis in patients with PD and Parkinson-plus syndromes. Quantification of these studies had limited utility since the overlapping of index values between normal and pathological restricts their use in individual cases [70]. Vlaar et al. reported that FP-CIT SPECT is accurate to differentiate patients with IPD from those with ET, and IPD from VP and DIP, but the accuracy of both FP-CIT and IBZM SPECT scans to differentiate between IPD and APS is low [54]. However, a study suggested that using multidimensional combination of FP-CIT, IBZM, and MIBG scintigraphy was likely to significantly increase test accuracy (94%) in differentiating PD from APS [71]. More recently, a study using 123I-PE21 indicated that dopamine transporter scan has a high sensitivity and specificity in distinguishing between patients with and without striatal neurodegeneration. Calculation of the striatal anterior-posterior ratio can assist in differentiating between idiopathic PD and APS [72]. Moreover, study with 123I-FP-CIT in165 patients with a clinical diagnosis of PD (n = 120) or APS (n = 45) suggested that a global and severe degeneration pattern had a high positive predictive value of APS within the first 5 years of the disease [73].
A 123I-FP-CIT and 123I-IBZM SPECT study, in which seven subjects were all from a Spanish family with G309D mutation in the PINK1 gene, showed that striatal DAT binding was reduced in all three PARK6 patients. But in two of the siblings, DAT binding was markedly increased. It suggested that the increased DAT binding may be an early preclinical finding [74]. SPECT is also useful for distinguishing PD from Dopa responsive dystonia (DRD), or for assessing the integrity of the nigrostriatal dopaminergic pathway in atypical cases of postural tremor or iatrogenic parkinsonian syndromes. The imaging with 99Tcm-TRODAT-1/123I-IBZM in a 39-year-old woman with a 24-year history of DRD indicated that 99Tcm-TRODAT-1 is helpful in differentiating DRD from early-onset idiopathic parkinsonism and the 123I-IBZM SPECT is also helpful in differentiating these two conditions in the later clinical course [75].
In IPD, two different clinical phenotypes are usually distinguished: a tremor-dominant variant (TD) and an akinetic-rigid type (ART). TD patients compared to ART patients are characterized by a slower disease progression and a minor cognitive impairment. For different phenotypes of PD, 123I-FP-CIT SPECT has indicated that the dopaminergic system in ART patients is more involved compared to that in the TD patients and that this kind of difference is present from the initial stage of the disease [76–78]. There was a significantly higher FP-CIT uptake in contralateral putamen and a higher but not statistically significant uptake in all the other striatal regions in TD patients when compared to ART patients [77]. Similarly, Spiegel et al. reported a greater impairment in ART patients in all striatal regions analyzed [78]. These results suggest that further systems besides the nigrostriatal dopaminergic system may contribute to generation of parkinsonian tremor.
3.4. Monitoring the Progression of the PD
Pathologic studies investigating the rate of PD progression have been limited to patients with severe illness of long duration and rely entirely on cross-sectional data. The UPDRS or other functional clinical endpoints are used to monitor disease progression. It makes it difficult to isolate clinical change solely due to disease progression [79].
The rate of progression of dopaminergic degeneration is much faster in PD than in normal aging [80]. Patients with PD present first with unilateral symptoms that gradually progress to involve both sides [6]. Clinical progression has been investigated with SPECT, which could prove to be an objective tool for monitoring the disease progression.
123I-β-CIT SPECT imaging of the dopamine transporter is a sensitive biomarker of PD onset and severity. A group of 50 early-stage PD patients was examined [81]. Two SPECT imaging series were obtained 12 months apart. The average decrease in 123I-β-CIT binding ratios was about 8% in the whole striatum, 8% in the putaminal region, and 4% in the caudate region. This finding supported the feasibility of using 123I-β-CIT in the evaluation of disease progression in PD [82]. Moreover, sequential SPECT scans using 123I-β-CIT in PD subjects demonstrated a decline in striatal uptake of approximately 11.2%/year from the baseline scan, compared with 0.8%/year in the healthy controls [79]. Another SPECT study with 123I-β-CIT demonstrated a rapid decline of striatal binding in patients with APS, exceeding the reduction in PD, and the dopaminergic degeneration in PD slows down during the course of the disease [83].
Combined 123I-β-CIT and 123I-IBZM SPECT studies have demonstrated that postsynaptic dopamine receptor upregulation contralateral to the presenting side occurs in untreated unilateral PD and disappears in untreated bilateral (asymmetric) PD despite a greater loss of dopamine transporter function [84]. This may be helpful in monitoring the progression of nigrostriatal dysfunction in early PD. Tatsch et al. [21] found that specific 123I-IPT uptake in the caudate and putamen, and putamen to caudate ratios, decreased with increasing Hoehn and Yahr stage (H-Y). These findings indicated that 123I-IPT SPECT also may be a useful technique to estimate the extent of nigrostriatal degeneration in PD patients.
Tissingh et al. reported that disease severity correlated negatively and highly significantly with the 123I-β-CIT binding in patients with early PD. Tremor ratings did not correlate with the 123I-β-CIT uptake, whereas rigidity and bradykinesia did [46]. The striatal 123I-β-CIT uptake in a large cohort of PD subjects significantly correlated with severity of PD as measured by UPDRS [79]. The mean reduction of 99Tcm-TRODAT-1 uptake was found in the order of putamen (contralateral side, −81%; ipsilateral side, −67%) and caudate nucleus (contralateral side, −46%; ipsilateral side, −40%), and it correlated negatively with the UPDRS and H-Y staging [85].
Winogrodzka et al. [80] used 123I-FP-CIT SPECT for the assessment of the rate of dopaminergic degeneration in PD. The mean annual decrease in striatal binding ratios in PD patients was found to be about 8% of the baseline mean, indicating that 123I-FP-CIT SPECT was applicable to investigate the progression of dopaminergic degeneration. The specific to nonspecific 123I-FP-CIT uptake ratios were calculated for striatum, caudate, and putamen, all of which were correlated with disease severity assessed by UPDRS and the duration of disease, suggesting that tremor may origins from other systems instead of the dopamine transporter system. Meanwhile, these ratios correlated with the bradykinesia subscore but not with rigidity or tremor subscore. It suggested that factors other than nigrostriatal degeneration may contribute to disease severity [36].
3.5. Evaluation of the Treatment Effect of PD
Current therapies include drug therapy, surgical procedures, and stem cell transplantation. Drug therapy such as DA replacement therapy with levodopa fails to prevent the progression of the disease process and only alleviates the clinical symptoms. Once the diagnosis is made, the neurologist with the patient must decide whether to institute treatment at the time of diagnosis or when functional disability occurs [86]. To evaluate the effectiveness of treatment, it is critical to develop methods that can reliably measure the progression of dopaminergic degeneration.
Postsynaptic imaging has been helpful in predicting therapeutic response to dopaminergic medication early in the course of Parkinson's disease. Studies have demonstrated that PD patients receiving treatment do better than those who do not, and those receiving treatment earlier do better in long term [87]. Schwarz et al. performed a follow-up study of 2–4 years including 55 patients with parkinsonism and prior dopaminomimetic therapy and found that IBZM-SPECT accurately predicted the response to apomorphine and levodopa, The sensitivity/specificity was 96.3%/64.7%, and 100%/75% [88]. Thus, 123I-IBZM can be used routinely to identify which PD patients will benefit from dopaminergic medication [89]. Another study including 20 PD patients who undergone short-term levodopa test and SPECT imaging found there was a relationship between responsiveness to levodopa and asymmetry detected with 123I-FP-CIT. This technique can predict dopaminergic responsiveness in patients with PD [90].
Recently, a 99Tcm-TRODAT-1 SPECT indicated that levodopa did not interfere with DAT binding, suggesting that differences between clinical assessment and radiotracer imaging in clinical trials may not be specifically related to levodopa treatment [91]. Similarly, the effect of subchronic treatment on striatal DAT was examined in patients who were not currently being treated with these medications. These results suggested that typical clinical doses of levodopa/carbidopa and L-selegiline did not induce significant occupancy of the 123I-β-CIT binding site and that 4–6 weeks of treatment caused no significant modulation of DAT levels. These results supported the validity of measuring DAT levels with 123I-β-CIT without the need to withdraw patients from medication treatment [92]. 123I-β-CIT SPECT imaging provides a quantitative biomarker for the progressive nigrostriatal dopaminergic degeneration in PD. As new protective and restorative therapies for PD are developed, dopamine transporter imaging offers the potential to provide an objective endpoint for these therapeutic trials [79, 80].
Hwang et al. found that the PD patients with fluctuating levodopa response showed a significant decrease in 123I-IBZM uptake (D2 receptor densities) than early levodopa-naive PD and chronic PD with stable levodopa response [93], which contributed to the development of motor fluctuation.
4. Discussion
It has been reported that PET using 18F-dopa represents a useful tool for detecting a reduction of dopaminergic activity in PD patients at a very early stage [94, 95]. But the uptake might be upregulated in the early phase of the disease whereas expression of DATs might be down-regulated. SPECT imaging combining both pre- and postsynaptic study as well as clinical criteria improves the diagnosis of early Parkinson's disease. The quantitative combination of presynaptic DAT and postsynaptic D2 receptor binding demonstrated higher diagnostic accuracy in the differentiation of patients with PD from patients with nonidiopathic parkinsonian syndromes than the established approach based on striatal D2 receptor binding alone [96].
The imaging of DAT with 99Tcm-TRODAT-1 SPECT has been recently proposed to be a valuable and feasible means of assessment of the integrity of dopamine neurons [45]. 123I-FP-CIT also has been successfully used to detect the loss of dopaminergic nigrostriatal neuron in PD at an early stage [47]. The sensitivity and specificity of this technique were 100% in discriminating PD patients from healthy subjects in the age-specific (>50 y) groups [85]. A bilateral loss of striatal DA transporters in patients with unilateral PD suggests that it may identify subjects in the preclinical phase of the disease.
There was a continuous reduction in specific striatal uptake especially for the putaminal uptake of 99Tcm-TRODAT-1 with increasing disease severity in Parkinson's disease patients. In PD patients, presynaptic neurodegeneration may affect the putamen and caudate with different severity [20]; however, there were no significant correlations between striatal 123I-FP-CIT binding ratios and disease severity as were established earlier with 99Tcm-TRODAT-1. Further research is necessary to interpret these findings.
The putaminal uptake contralateral to the more affected limbs was significantly reduced compared with the ipsilateral sides and the difference became greater when the posterior putaminal uptakes were compared [49], and the discriminant function analysis of both the ipsilateral and contralateral putamen classified 100% of their patients correctly, whereas analysis using only the contralateral putamen classified 92% of cases correctly [46]. PET imaging using 18F-DOPA also demonstrated a significant abnormality in the posterior putamen of PD patients [97]. In conclusion, the analysis using the mean of the ipsilateral and contralateral posterior putamen may result in the greatest accuracy.
The study confirms asymmetric D2 receptor upregulation in PD. However, the sensitivity of contralateral higher striatal 123I-IBZM binding is only not so obvious, therefore, PD cannot be excluded in patients with parkinsonism and no contralateral upregulation of D2 receptors [34]. The exact diagnostic accuracy of this technique in parkinsonian syndromes remains controversial.
MSA and PD patients are difficult to differentiate from each other. Imaging studies using different dopamine transporters in MSA patients have reported same results: DAT binding was significantly decreased in all regions in both IPD and MSA patients as compared with healthy subjects. A study by using 123I-β-CIT SPECT demonstrated that the posterior putamen is more involved than the caudate in MSA [67]. Another study using 99Tcm-TRODAT-1 showed MSA patients had significantly higher tracer uptake particularly in the posterior putamen compared with PD patients and significantly lower uptake compared with controls. The result suggested that the two neurodegenerative diseases have different pathophysiological processes [66].
A large retrospective study [54] on the diagnostic value of the FP-CIT and IBZM SPECT scan in patients with parkinsonian symptoms of unknown origin concluded that FP-CIT SPECT is accurate to differentiate patients with IPD from those with ET, and IPD from VP and DIP, but the two scans had low accuracy to differentiate between IPD and APS.
Age is the largest risk factor for the development and progression of PD [98]. PD may reflect a failure of the normal cellular compensatory mechanisms in vulnerable brain regions, and this vulnerability is increased by ageing. PD is one of the best examples of an age-related disease. Presynaptic imaging has demonstrated the ability to objectively measure the progression of Parkinson's disease. Although the rate of progression of the dopaminergic terminal loss in patients with PD was correlated with clinical severity, the annual percentage loss of 123I-β-CIT striatal uptake did not correlate with the annual loss in measures of clinical function [79]. Striatal 123I-IPT uptake was closely related to the stage of PD. The binding ratios decreased markedly from H-Y stage I to stage IV; in addition, this imaging technique has a special advantage that data can be acquired within a few hours after injection [21]. The rate of progression may be faster in APS than in PD [83]. To interprete the results well, caution must be paid in the studies in which therapeutic effects in Parkinson's disease were also monitored by serial imaging of nigrostriatal neurons [99].
For different phenotype of PD, FP-CIT striatal uptake values significantly correlated with bradykinesia and rigidity but not with tremor [78], putaminal relative sparing in TD patients could partially contribute to the slower disease progression. This fact could explain the different disease progression with a more benign course in TD group. A widespread degeneration of the nigrostriatal dopaminergic pathway might be necessary for the development of parkinsonian tremor at rest [100].
Early Parkinson's disease is dominated by a motor syndrome called parkinsonism, but as the disease develops motor complications and nonmotor problems may occur as well [6].
The results of imaging of dopamine-D2 receptors with the improvement in motor signs by the injection of apomorphine and oral dopaminomimetic therapy were compared [88]. It can be concluded that normal IBZM binding is a useful predictor of a good response to dopaminergic drugs in PD patients and a questionable response to previous dopaminomimetic therapy. However, reduced IBZM binding seems to exclude a diagnosis of PD but suggests another disorder of the basal ganglia.
To evaluate effect of treatment with drugs on striatal DAT, the imaging was performed before treatment, while on medication, and following withdrawal from medication in each patient. Thus, the results provided a measurement of DAT levels and drug occupancy following subchronic drug treatment and drug occupancy of the tracer binding site [92].
Semiquantification of striatal uptake is more correct than visual reading, but it is also time consuming and prone to error, particularly if the VOIs are positioned manually. There is a critical need to create a new technique to solve this problem. A new software tool (“IBZM tool”) was presented for fully automated and standardized processing, evaluating and documenting the 123I-IBZM SPECT scans [101].
MIBG may be a peripheral biological marker of PD including triplication of the a-synuclein gene. Although diagnostic accuracy of cardiac MIBG scintigram in PD is high, the sensitivity is insufficient in patients with short duration [43]. Because of its relatively lower sensitivity, cardiac 123I-MIBG scintigraphy is of limited value in the diagnosis of early PD. However, because of its high specificity, it may assist in the diagnosis of PD [51]. Furthermore, Fukuyama [102] analyzed the reports about MIBG imaging in PD, and suggested that it should not be regarded as the first and best choice of diagnostic aid for PD, especially in the early stages, and careful attention should be paid for diagnosis of PD or diffused Lewy body disease.
A study showed there is an association between urinary dysfunction and degeneration of the nigrostriatal dopaminergic cells in PD [52]. The results may promote further studies of dopaminergic drug treatments on urinary dysfunction in PD.
5. Perspective
SPECT imaging has proven to be a useful tool to investigate the many facets of PD in vivo. This technique helps understand the pathogenesis, the differential diagnosis, and the progression of the PD.
The disadvantage of SPECT compared to PET is that it is difficult to obtain a reliable quantification. Furthermore, the resolution of images is a limitation for the visualization of basal ganglia in PD. However, SPECT is more practical as a routine procedure than PET. In the future, the technique that provides high accuracy and new radiotracers needs to be developed to help understand the role of non-DA neurotransmitter systems in PD.
SPECT combined with other techniques such as transcranial sonography and olfaction test may have a higher accuracy in the diagnosis of PD. Imaging agents like dopamine transporter or D2 receptor ligands assess only part of aspects of the dopamine neurons. New tracers need to be synthesized to detect other aspects of dopamine neurons.
The SPECT imaging of the nigrostriatal dopaminergic pathway can be used to monitor therapeutic effects in Parkinson's disease. As new protective and restorative therapies for PD are developed, dopamine transporter imaging offers the potential to provide an objective endpoint for these therapeutic trials. Further studies are needed to evaluate the possible effects of the therapy, especially for the delayed-onset bilateral symptoms. Moreover, there is a pressing need to improve our understanding of the pathogenesis to enable development of disease modifying treatments.
Conflict of Interests
The authors declare that they have no conflict of interests.
Acknowledgments
This work is partly sponsored by Grants from the Zhejiang Provincial Natural Science Foundation of China (Z2110230), Health Bureau of Zhejiang Province (2010ZA075, 2011ZDA013), National Science Foundation of China (NSFC) (nos. 81101023, 81170306, 81173468), and Ministry of Science and Technology of China (2011CB504400, 2012BAI13B06).
Abbreviations
- SPECT:
Single-photon emission computed tomography
- DAT:
Dopamine transporter
- PD:
Parkinson's disease
- PET:
Positron emission tomography
- SERT:
Serotonin transporter
- CNS:
Central nervous system
- CUPS:
Clinically Unclear Parkinsonian Syndromes
- UPDRS:
United Parkinson's disease rating scale
- APS:
Atypical parkinsonian syndromes
- MSA:
Multiple system atrophy
- PSP:
Progressive supranuclear palsy
- DIP:
Drug induced parkinsonism
- ET:
Essential tremor
- VP:
Vascular Parkinsonism
- DLB:
Dementia with Lewy Bodies
- VOIs:
Volumes of interests
- IPD:
Idiopathic Parkinson's disease
- DVRs:
Distribution volume ratios
- DRD:
Dopa-responsive dystonia
- TD:
Tremor-dominant variant
- ART:
Akinetic-rigid type
- H-Y:
Hoehn and Yahr.
References
- 1.Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. Journal of Neurology Neurosurgery and Psychiatry. 1992;55(3):181–184. doi: 10.1136/jnnp.55.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruipérez V, Darios F, Davletov B. Alpha-synuclein, lipids and Parkinson’s disease. Progress in Lipid Research. 2010;49(4):420–428. doi: 10.1016/j.plipres.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Leong SL, Cappai R, Barnham KJ, Pham CLL. Modulation of α-synuclein aggregation by dopamine: a review. Neurochemical Research. 2009;34(10):1838–1846. doi: 10.1007/s11064-009-9986-8. [DOI] [PubMed] [Google Scholar]
- 4.Bellucci A, Collo G, Sarnico I, Battistin L, Missale C, Spano P. Alpha-synuclein aggregation and cell death triggered by energy deprivation and dopamine overload are counteracted by D2/D3 receptor activation. Journal of Neurochemistry. 2008;106(2):560–577. doi: 10.1111/j.1471-4159.2008.05406.x. [DOI] [PubMed] [Google Scholar]
- 5.Braak H, Del Tredici K, Rüb U, de Vos RAI, Jansen Steur ENH, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiology of Aging. 2003;24(2):197–211. doi: 10.1016/s0197-4580(02)00065-9. [DOI] [PubMed] [Google Scholar]
- 6.Larsen JP, Beiske AG, Bekkelund SI, et al. Motor symptoms in Parkinson’s disease. Tidsskrift for den Norske Laegeforening. 2008;128(18):2068–2071. [PubMed] [Google Scholar]
- 7.Peppard RF, Martin WRW, Carr GD, et al. Cerebral glucose metabolism in Parkinson’s disease with and without dementia. Archives of Neurology. 1992;49(12):1262–1268. doi: 10.1001/archneur.1992.00530360060019. [DOI] [PubMed] [Google Scholar]
- 8.Kummer A, Scalzo P, Cardoso F, Teixeira AL. Evaluation of fatigue in Parkinson’s disease using the Brazilian version of Parkinson’s Fatigue Scale. Acta Neurologica Scandinavica. 2011;123(2):130–136. doi: 10.1111/j.1600-0404.2010.01364.x. [DOI] [PubMed] [Google Scholar]
- 9.Prediger RDS, Matheus FC, Schwarzbold ML, Lima MMS, Vital MABF. Anxiety in Parkinson's disease: a critical review of experimental and clinical studies. Neuropharmacology. 2012;62(1):115–124. doi: 10.1016/j.neuropharm.2011.08.039. [DOI] [PubMed] [Google Scholar]
- 10.Aarsland D, Brønnick K, Larsen JP, Tysnes OB, Alves G. Cognitive impairment in incident, untreated parkinson disease: the norwegian parkwest study. Neurology. 2009;72(13):1121–1126. doi: 10.1212/01.wnl.0000338632.00552.cb. [DOI] [PubMed] [Google Scholar]
- 11.Magerkurth C, Schnitzer R, Braune S. Symptoms of autonomic failure in Parkinson’s disease: prevalence and impact on daily life. Clinical Autonomic Research. 2005;15(2):76–82. doi: 10.1007/s10286-005-0253-z. [DOI] [PubMed] [Google Scholar]
- 12.O'Sullivan SS, Wu K, Politis M, et al. Cue-induced striatal dopamine release in Parkinson's disease-associated impulsive-compulsive behaviours. Brain. 2011;134, part 4:969–978. doi: 10.1093/brain/awr003. [DOI] [PubMed] [Google Scholar]
- 13.Morgante L, Colosimo C, Antonini A, et al. Psychosis associated to Parkinson's disease in the early stages: relevance of cognitive decline and depression. Journal of Neurology, Neurosurgery and Psychiatry. 2012;83(1):76–82. doi: 10.1136/jnnp-2011-300043. [DOI] [PubMed] [Google Scholar]
- 14.Berendse HW, Roos DS, Raijmakers P, Doty RL. Motor and non-motor correlates of olfactory dysfunction in Parkinson's disease. Journal of the Neurological Sciences. 2011;310(1-2):21–24. doi: 10.1016/j.jns.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 15.Cohenpour M, Golan H. Nuclear neuroimaging of dopamine transporter in Parkinsonism—role in routine clinical practice. Harefuah. 2007;146(9):698–702. [PubMed] [Google Scholar]
- 16.Meara J, Bhowmick BK, Hobson P. Accuracy of diagnosis in patients with presumed Parkinson’s disease. Age and Ageing. 1999;28(2):99–102. doi: 10.1093/ageing/28.2.99. [DOI] [PubMed] [Google Scholar]
- 17.Marshall V, Grosset D. Role of dopamine transporter imaging in routine clinical practice. Movement Disorders. 2003;18(12):1415–1423. doi: 10.1002/mds.10592. [DOI] [PubMed] [Google Scholar]
- 18.Thobois S, Guillouet S, Broussolle E. Contributions of PET and SPECT to the understanding of the pathophysiology of Parkinson’s disease. Neurophysiologie Clinique. 2001;31(5):321–340. doi: 10.1016/s0987-7053(01)00273-8. [DOI] [PubMed] [Google Scholar]
- 19.Seibyl JP, Marek K, Sheff K, et al. Iodine-123-β-CIT and iodine-123-FPCIT SPECT measurement of dopamine transporters in healthy subjects and Parkinson’s patients. Journal of Nuclear Medicine. 1998;39(9):1500–1508. [PubMed] [Google Scholar]
- 20.Tissingh G, Booij J, Bergmans P, et al. Iodine-123-N-ω-fluoropropyl-2/β-carbomethoxy3β-(4-iodophenyl)tropane SPECT in healthy controls and early-stage, drug-naive Parkinson’s disease. Journal of Nuclear Medicine. 1998;39(7):1143–1148. [PubMed] [Google Scholar]
- 21.Tatsch K, Schwarz J, Mozley PD, et al. Relationship between clinical features of Parkinson’s disease and presynaptic dopamine transporter binding assessed with [123I]IPT and single-photon emission tomography. European Journal of Nuclear Medicine. 1997;24(4):415–421. doi: 10.1007/BF00881814. [DOI] [PubMed] [Google Scholar]
- 22.Emond P, Guilloteau D, Chalon S. PE2I: a radiopharmaceutical for in vivo exploration of the dopamine transporter. CNS Neuroscience and Therapeutics. 2008;14(1):47–64. doi: 10.1111/j.1527-3458.2007.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Page G, Chalon S, Emond P, Maloteaux JM, Hermans E. Pharmacological characterisation of (E)-N-(3-iodoprop-2-enyl)-2β-carbomethoxy-3β-(4′-methylphenyl)nortropane (PE2I) binding to the rat neuronal dopamine transporter expressed in COS cells. Neurochemistry International. 2002;40(2):105–113. doi: 10.1016/s0197-0186(01)00086-9. [DOI] [PubMed] [Google Scholar]
- 24.Ziebell M. Evaluation of the superselective radioligand [123I]PE2I for imaging of the dopamine transporter in SPECT. Danish Medical Bulletin. 2011;58(5) Article ID B4279. [PubMed] [Google Scholar]
- 25.Huang WS, Chiang YH, Lin JC, Chou YH, Cheng CY, Liu RS. Crossover study of (99m)Tc-TRODAT-1 SPECT and 18F-FDOPA PET in Parkinson’s disease patients. Journal of Nuclear Medicine. 2003;44(7):999–1005. [PubMed] [Google Scholar]
- 26.Kung HF, Pan S, Kung MP, et al. In vitro and in vivo evaluation of [123I]IBZM: a potential CNS D-2 dopamine receptor imaging agent. Journal of Nuclear Medicine. 1989;30(1):88–92. [PubMed] [Google Scholar]
- 27.Kung MP, Kung HF, Billings J, Yang Y, Murphy RA, Alavi A. The characterization of IBF as a new selective dopamine D-2 receptor imaging agent. Journal of Nuclear Medicine. 1990;31(5):648–654. [PubMed] [Google Scholar]
- 28.Al-Tikriti MS, Baldwin RM, Zea-Ponce Y, et al. Comparison of three high affinity SPECT radiotracers for the dopamine D2 receptor. Nuclear Medicine and Biology. 1994;21(2):179–188. doi: 10.1016/0969-8051(94)90007-8. [DOI] [PubMed] [Google Scholar]
- 29.Matsumoto H, Tanaka A, Suzuki N, Kondo S, KatoAzuma M, Yonekura Y. Metabolism of 123I-IBF in humans. Kakuigaku. 1999;36(2):169–177. [PubMed] [Google Scholar]
- 30.Murphy RA, Kung HF, Kung MP, Billings J. Synthesis and characterization of iodobenzamide analogues: potential D-2 dopamine receptor imaging agents. Journal of Medicinal Chemistry. 1990;33(1):171–178. doi: 10.1021/jm00163a029. [DOI] [PubMed] [Google Scholar]
- 31.Spiegel J, Hellwig D, Jost WH, et al. Cerebral and extracranial neurodegeneration are strongly coupled in Parkinson's disease. The Open Neurology Journal. 2007;1:1–4. doi: 10.2174/1874205X00701010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seibyl JP, Marchek KL, Quinlan D, et al. Decreased single-photon emission computed tomographic [123I]β-CIT striatal uptake correlates with symptom severity in Parkinson’s disease. Annals of Neurology. 1995;38(4):589–598. doi: 10.1002/ana.410380407. [DOI] [PubMed] [Google Scholar]
- 33.Ichise M, Kim YJ, Ballinger JR, et al. SPECT imaging of pre- and postsynaptic dopaminergic alterations in L-dopa-untreated PD. Neurology. 1999;52(6):1206–1214. doi: 10.1212/wnl.52.6.1206. [DOI] [PubMed] [Google Scholar]
- 34.Verstappen CCP, Bloem BR, Haaxma CA, Oyen WJG, Horstink MWIM. Diagnostic value of asymmetric striatal D2 receptor upregulation in Parkinson’s disease: an [123I]IBZM and [123I]FP-CIT SPECT study. European Journal of Nuclear Medicine and Molecular Imaging. 2007;34(4):502–507. doi: 10.1007/s00259-006-0258-4. [DOI] [PubMed] [Google Scholar]
- 35.Ma KH, Huang WS, Chen CH, et al. Dual SPECT of dopamine system using [(99m)Tc]TRODAT-1 and [123I]IBZM in normal and 6-OHDA-lesioned formosan rock monkeys. Nuclear Medicine and Biology. 2002;29(5):561–567. doi: 10.1016/s0969-8051(02)00303-7. [DOI] [PubMed] [Google Scholar]
- 36.Benamer HTS, Patterson J, Wyper DJ, Hadley DM, Macphee GJA, Grosset DG. Correlation of Parkinson’s disease severity and duration with 123I-FP-CIT SPECT striatal uptake. Movement Disorders. 2000;15(4):692–698. doi: 10.1002/1531-8257(200007)15:4<692::aid-mds1014>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 37.Eggers C, Kahraman D, Fink GR, Schmidt M, Timmermann L. Akinetic-rigid and tremor-dominant Parkinson's disease patients show different patterns of FP-CIT Single photon emission computed tomography. Movement Disorders. 2011;26(3):416–423. doi: 10.1002/mds.23468. [DOI] [PubMed] [Google Scholar]
- 38.Kish SJ, Tong J, Hornykiewicz O, et al. Preferential loss of serotonin markers in caudate versus putamen in Parkinson’s disease. Brain. 2008;131, part 1:120–131. doi: 10.1093/brain/awm239. [DOI] [PubMed] [Google Scholar]
- 39.Roselli F, Pisciotta NM, Pennelli M, et al. Midbrain SERT in degenerative parkinsonisms: a 123I-FP-CIT SPECT study. Movement Disorders. 2010;25(12):1853–1859. doi: 10.1002/mds.23179. [DOI] [PubMed] [Google Scholar]
- 40.Marek KL, Seibyl JP, Zoghbi SS, et al. [123I] β-CIT/SPECT imaging demonstrates bilateral loss of dopamine transporters in hemi-Parkinson’s disease. Neurology. 1996;46(1):231–237. doi: 10.1212/wnl.46.1.231. [DOI] [PubMed] [Google Scholar]
- 41.Eerola J, Tienari PJ, Kaakkola S, Nikkinen P, Launes J. How useful is [123I]β-CIT SPECT in clinical practice? Journal of Neurology, Neurosurgery and Psychiatry. 2005;76(9):1211–1216. doi: 10.1136/jnnp.2004.045237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marshall VL, Reininger CB, Marquardt M, et al. Parkinson’s disease is overdiagnosed clinically at baseline in diagnostically uncertain cases: a 3-year European multicenter study with repeat [123I]FP-CIT SPECT. Movement Disorders. 2009;24(4):500–508. doi: 10.1002/mds.22108. [DOI] [PubMed] [Google Scholar]
- 43.Sawada H, Oeda T, Yamamoto K, et al. Diagnostic accuracy of cardiac metaiodobenzylguanidine scintigraphy in Parkinson disease. European Journal of Neurology. 2009;16(2):174–182. doi: 10.1111/j.1468-1331.2008.02372.x. [DOI] [PubMed] [Google Scholar]
- 44.Spiegel J, Möllers MO, Jost WH, et al. FP-CIT and MIBG scintigraphy in early Parkinson’s disease. Movement Disorders. 2005;20(5):552–561. doi: 10.1002/mds.20369. [DOI] [PubMed] [Google Scholar]
- 45.Chou KL, Hurtig HI, Stern MB, et al. Diagnostic accuracy of [(99m)Tc]TRODAT-1 SPECT imaging in early Parkinson’s disease. Parkinsonism and Related Disorders. 2004;10(6):375–379. doi: 10.1016/j.parkreldis.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 46.Tissingh G, Bergmans P, Booij J, et al. Drug-naive patients with Parkinson’s disease in Hoehn and Yahr stages I and II show a bilateral decrease in striatal dopamine transporters as revealed by [123I]β-CIT SPECT. Journal of Neurology. 1998;245(1):14–20. doi: 10.1007/s004150050168. [DOI] [PubMed] [Google Scholar]
- 47.Filippi L, Manni C, Pierantozzi M, et al. 123I-FP-CIT semi-quantitative SPECT detects preclinical bilateral dopaminergic deficit in early Parkinson’s disease with unilateral symptoms. Nuclear Medicine Communications. 2005;26(5):421–426. doi: 10.1097/00006231-200505000-00005. [DOI] [PubMed] [Google Scholar]
- 48.Huang WS, Ma KH, Chou YH, Chen CY, Liu RS, Liu JC. (99m)Tc-TRODAT-1 SPECT in healthy and 6-OHDA lesioned parkinsonian monkeys: comparison with 18F-FDOPA PET. Nuclear medicine communications. 2003;24(1):77–83. doi: 10.1097/00006231-200301000-00018. [DOI] [PubMed] [Google Scholar]
- 49.Huang WS, Lin SZ, Lin JC, Wey SP, Ting G, Liu RS. Evaluation of early-stage Parkinson’s disease with (99m)Tc-TRODAT-1 imaging. Journal of Nuclear Medicine. 2001;42(9):1303–1308. [PubMed] [Google Scholar]
- 50.Kägi G, Bhatia KP, Tolosa E. The role of DAT-SPECT in movement disorders. Journal of Neurology, Neurosurgery and Psychiatry. 2010;81(1):5–12. doi: 10.1136/jnnp.2008.157370. [DOI] [PubMed] [Google Scholar]
- 51.Ishibashi K, Saito Y, Murayama S, et al. Validation of cardiac 123I-MIBG scintigraphy in patients with Parkinson’s disease who were diagnosed with dopamine PET. European Journal of Nuclear Medicine and Molecular Imaging. 2010;37(1):3–11. doi: 10.1007/s00259-009-1202-1. [DOI] [PubMed] [Google Scholar]
- 52.Sakakibara R, Shinotoh H, Uchiyama T, Yoshiyama M, Hattori T, Yamanishi T. SPECT imaging of the dopamine transporter with [123I]-β-CIT reveals marked decline of nigrostriatal dopaminergic function in Parkinson’s disease with urinary dysfunction. Journal of the Neurological Sciences. 2001;187(1-2):55–59. doi: 10.1016/s0022-510x(01)00521-4. [DOI] [PubMed] [Google Scholar]
- 53.Agid Y. Parkinson’s disease: pathophysiology. The Lancet. 1991;337(8753):1321–1324. doi: 10.1016/0140-6736(91)92989-f. [DOI] [PubMed] [Google Scholar]
- 54.Vlaar AMM, de Nijs T, Kessels AGH, et al. Diagnostic value of 123I-ioflupane and 123I-iodobenzamide SPECT scans in 248 patients with Parkinsonian syndromes. European Neurology. 2008;59(5):258–266. doi: 10.1159/000115640. [DOI] [PubMed] [Google Scholar]
- 55.Contrafatto D, Mostile G, Nicoletti A, et al. [123I]FP-CIT-SPECT asymmetry index to differentiate Parkinson's disease from vascular parkinsonism. Acta Neurologica Scandinavica. doi: 10.1111/j.1600-0404.2011.01583.x. In press. [DOI] [PubMed] [Google Scholar]
- 56.Loberboym M, Traves TA, Melamed E, Lampl Y, Hellman M, Djaldetti R. [123I]-EP/CIT SPECT imaging for distinguishing drug-induced Parkinsonism from Parkinson's disease. Movement Disorders. 2006;21(4):510–514. doi: 10.1002/mds.20748. [DOI] [PubMed] [Google Scholar]
- 57.Diaz-Corrales FJ, Sanz-Viedma S, Garcia-Solis D, Escobar-Delgado T, Mir P. Clinical features and 123I-FP-CIT SPECT imaging in drug-induced parkinsonism and Parkinson’s disease. European Journal of Nuclear Medicine and Molecular Imaging. 2010;37(3):556–564. doi: 10.1007/s00259-009-1289-4. [DOI] [PubMed] [Google Scholar]
- 58.Cuberas-Borrós G, Lorenzo-Bosquet C, Aguadé-Bruix S, et al. Quantitative evaluation of striatal I-123-FP-CIT uptake in essential tremor and parkinsonism. Clinical Nuclear Medicine. 2011;36(11):991–996. doi: 10.1097/RLU.0b013e3182291a7b. [DOI] [PubMed] [Google Scholar]
- 59.Felicio AC, Shih MC, Godeiro-Junior C, Andrade LAF, Bressan RA, Ferraz HB. Molecular imaging studies in Parkinson disease reducing diagnostic uncertainty. Neurologist. 2009;15(1):6–16. doi: 10.1097/NRL.0b013e318183fdd8. [DOI] [PubMed] [Google Scholar]
- 60.Gilman S, Wenning GK, Low PA, et al. Second consensus statement on the diagnosis of multiple system atrophy. Neurology. 2008;71(9):670–676. doi: 10.1212/01.wnl.0000324625.00404.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Scherfler C, Seppi K, Donnemiller E, et al. Voxel-wise analysis of [123I]β-CIT SPECT differentiates the Parkinson variant of multiple system atrophy from idiopathic Parkinson’s disease. Brain. 2005;128, part 7:1605–1612. doi: 10.1093/brain/awh485. [DOI] [PubMed] [Google Scholar]
- 62.El Fakhri G, Ouyang J. Dual-radionuclide brain SPECT for the differential diagnosis of parkinsonism. Methods in Molecular Biology. 2011;680:237–246. doi: 10.1007/978-1-60761-901-7_16. [DOI] [PubMed] [Google Scholar]
- 63.Antonini A, Benti R, de Notaris R, et al. 123I-Ioflupane/SPECT binding to striatal dopamine transporter (DAT) uptake in patients with Parkinson’s disease, multiple system atrophy, and progressive supranuclear palsy. Neurological Sciences. 2003;24(3):149–150. doi: 10.1007/s10072-003-0103-5. [DOI] [PubMed] [Google Scholar]
- 64.Varrone A, Marek KL, Jennings D, Innis RB, Seibyl JP. [123I]β-CIT SPECT imaging demonstrates reduced density of striatal dopamine transporters in Parkinson’s disease and multiple system atrophy. Movement Disorders. 2001;16(6):1023–1032. doi: 10.1002/mds.1256. [DOI] [PubMed] [Google Scholar]
- 65.Knudsen GM, Karlsborg M, Thomsen G, et al. Imaging of dopamine transporters and D2 receptors in patients with Parkinson’s disease and multiple system atrophy. European Journal of Nuclear Medicine and Molecular Imaging. 2004;31(12):1631–1638. doi: 10.1007/s00259-004-1578-x. [DOI] [PubMed] [Google Scholar]
- 66.Swanson RL, Newberg AB, Acton PD, et al. Differences in [(99m)Tc]TRODAT-1 SPECT binding to dopamine transporters in patients with multiple system atrophy and Parkinson’s disease. European Journal of Nuclear Medicine and Molecular Imaging. 2005;32(3):302–307. doi: 10.1007/s00259-004-1667-x. [DOI] [PubMed] [Google Scholar]
- 67.Kim YJ, Ichise M, Ballinger JR, et al. Combination of dopamine transporter and D2 receptor SPECT in the diagnostic evaluation of PD, MSA, and PSP. Movement Disorders. 2002;17(2):303–312. doi: 10.1002/mds.10042. [DOI] [PubMed] [Google Scholar]
- 68.Pöpperl G, Radau P, Linke R, Hahn K, Tatsch K. Diagnostic performance of a 3-D automated quantification method of dopamine D2 receptor SPECT studies in the differential diagnosis of parkinsonism. Nuclear Medicine Communications. 2005;26(1):39–43. doi: 10.1097/00006231-200501000-00007. [DOI] [PubMed] [Google Scholar]
- 69.Oyanagi C, Katsumi Y, Hanakawa T, et al. Comparison of striatal dopamine D2 receptors in Parkinson’s disease and progressive supranuclear palsy patients using [123I] iodobenzofuran single-photon emission computed tomography. Journal of Neuroimaging. 2002;12(4):316–324. doi: 10.1111/j.1552-6569.2002.tb00139.x. [DOI] [PubMed] [Google Scholar]
- 70.Poblete Garcíau VM, García Vicente A, Ruíz Solís S, et al. SPECT with 123I-IBZM: utility in differential diagnosis of degenerative Parkinsonisms and establishment of quantification method. Revista Espanola de Medicina Nuclear. 2005;24(4):234–243. doi: 10.1157/13076641. [DOI] [PubMed] [Google Scholar]
- 71.Südmeyer M, Antke C, Zizek T, et al. Diagnostic accuracy of combined FP-CIT, IBZM, and MIBG scintigraphy in the differential diagnosis of degenerative parkinsonism: a multidimensional statistical approach. Journal of Nuclear Medicine. 2011;52(5):733–740. doi: 10.2967/jnumed.110.086959. [DOI] [PubMed] [Google Scholar]
- 72.Ziebell M, Andersen BB, Thomsen G, et al. Predictive value of dopamine transporter SPECT imaging with [123I]PE2I in patients with subtle parkinsonian symptoms. European Journal of Nuclear Medicine and Molecular Imaging. 2012;39(2):242–250. doi: 10.1007/s00259-011-1976-9. [DOI] [PubMed] [Google Scholar]
- 73.Kahraman D, Eggers C, Schicha H, Timmermann L, Schmidt M. Visual assessment of dopaminergic degeneration pattern in 123I-FP-CIT SPECT differentiates patients with atypical parkinsonian syndromes and idiopathic Parkinson's disease. Journal of Neurology. 2011;259(2):251–260. doi: 10.1007/s00415-011-6163-1. [DOI] [PubMed] [Google Scholar]
- 74.Kessler KR, Hamscho N, Morales B, et al. Dopaminergic function in a family with the PARK6 form of autosomal recessive Parkinson’s syndrome. Journal of Neural Transmission. 2005;112(10):1345–1353. doi: 10.1007/s00702-005-0281-9. [DOI] [PubMed] [Google Scholar]
- 75.Hwang WJ, Yao WJ, Wey SP, Ting G. Clinical and [(99m)Tc]TRODAT-1/[123I]IBZM SPECT imaging findings in dopa-responsive dystonia. European Neurology. 2004;51(1):26–29. doi: 10.1159/000074914. [DOI] [PubMed] [Google Scholar]
- 76.Schilaci O, Chiaravaloti A, Pierantozzi M, et al. Different patterns of nigrostriatal degeneration in tremor type versus the akinetic-rigid and mixed types of Parkinson's disease at the early stages: molecular imaging with 123I-FP-CIT SPECT. International Journal of Molecular Medicine. 2011;28(5):881–886. doi: 10.3892/ijmm.2011.764. [DOI] [PubMed] [Google Scholar]
- 77.Rossi C, Frosini D, Volterrani D, et al. Differences in nigro-striatal impairment in clinical variants of early Parkinson’s disease: evidence from a FP-CIT SPECT study. European Journal of Neurology. 2010;17(4):626–630. doi: 10.1111/j.1468-1331.2009.02898.x. [DOI] [PubMed] [Google Scholar]
- 78.Spiegel J, Hellwig D, Samnick S, et al. Striatal FP-CIT uptake differs in the subtypes of early Parkinson’s disease. Journal of Neural Transmission. 2007;114(3):331–335. doi: 10.1007/s00702-006-0518-2. [DOI] [PubMed] [Google Scholar]
- 79.Marek K, Innis R, van Dyck C, et al. [123I] β-CIT SPECT imaging assessment of the rate of Parkinson’s disease progression. Neurology. 2001;57(11):2089–2094. doi: 10.1212/wnl.57.11.2089. [DOI] [PubMed] [Google Scholar]
- 80.Winogrodzka A, Bergmans P, Booij J, van Royen EA, Janssen AG, Wolters EC. [123I]FP-CIT SPECT is a useful method to monitor the rate of dopaminergic degeneration in early-stage Parkinson’s disease. Journal of Neural Transmission. 2001;108(8-9):1011–1019. doi: 10.1007/s007020170019. [DOI] [PubMed] [Google Scholar]
- 81.Winogrodzka A, Bergmans P, Booij J, van Royen EA, Stoof JC, Wolters EC. [123I]β-CIT SPECT is a useful method for monitoring dopaminergic degeneration in early stage Parkinson’s disease. Journal of Neurology Neurosurgery and Psychiatry. 2003;74(3):294–298. doi: 10.1136/jnnp.74.3.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Seibyl JP, Marek K, Sheff K, et al. Test/retest reproducibility of iodine-123-βCIT SPECT brain measurement of dopamine transporters in Parkinson’s patients. Journal of Nuclear Medicine. 1997;38(9):1453–1459. [PubMed] [Google Scholar]
- 83.Pirker W, Djamshidian S, Asenbaum S, et al. Progression of dopaminergic degeneration in Parkinson’s disease and atypical parkinsonism: a longitudinal β-CIT SPECT study. Movement Disorders. 2002;17(1):45–53. doi: 10.1002/mds.1265. [DOI] [PubMed] [Google Scholar]
- 84.Wenning GK, Donnemiller E, Granata R, Riccabona G, Poewe W. 123I-β-CIT and 123I-IBZM-SPECT scanning in levodopa-naive Parkinson’s disease. Movement Disorders. 1998;13(3):438–445. doi: 10.1002/mds.870130311. [DOI] [PubMed] [Google Scholar]
- 85.Weng YH, Yen TC, Chen MC, et al. Sensitivity and specificity of (99m)Tc-TRODAT-1 SPECT imaging in differentiating patients with idiopathic Parkinson’s disease from healthy subjects. Journal of Nuclear Medicine. 2004;45(3):393–401. [PubMed] [Google Scholar]
- 86.Weiner WJ. Early diagnosis of Parkinson’s disease and initiation of treatment. Reviews in Neurological Diseases. 2008;5(2):46–53. quiz 54-55. [PubMed] [Google Scholar]
- 87.Lyons KE, Pahwa R. Diagnosis and initiation of treatment in Parkinson's disease. International Journal of Neuroscience. 2011;121, supplement 2:27–36. doi: 10.3109/00207454.2011.620197. [DOI] [PubMed] [Google Scholar]
- 88.Schwarz J, Tatsch K, Gasser T, Arnold G, Oertel WH. [123I]IBZM binding predicts dopaminergic responsiveness in patients with parkinsonism and previous dopaminomimetic therapy. Movement Disorders. 1997;12(6):898–902. doi: 10.1002/mds.870120610. [DOI] [PubMed] [Google Scholar]
- 89.Hertel A, Weppner M, Baas H, et al. Quantification of IBZM dopamine receptor SPET in de novo Parkinson patients before and during therapy. Nuclear Medicine Communications. 1997;18(9):811–822. doi: 10.1097/00006231-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 90.Contrafatto D, Mostile G, Nicoletti A, et al. Single photon emission computed tomography striatal asymmetry index may predict dopaminergic responsiveness in Parkinson disease. Clinical Neuropharmacology. 2011;34(2):71–73. doi: 10.1097/WNF.0b013e318211f945. [DOI] [PubMed] [Google Scholar]
- 91.Fernagut PO, Li Q, Dovero S, et al. Dopamine transporter binding is unaffected by L-DOPA administration in normal and MPTP-treated monkeys. PLoS ONE. 2010;5(11) doi: 10.1371/journal.pone.0014053. Article ID e14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Innis RB, Marek KL, Sheff K, et al. Effect of treatment with L-dopa/carbidopa or L-selegiline on striatal dopamine transporter SPECT imaging with [123I]β-CIT. Movement Disorders. 1999;14(3):436–442. doi: 10.1002/1531-8257(199905)14:3<436::aid-mds1008>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 93.Hwang WJ, Yao WJ, Wey SP, Shen LH, Ting G. Downregulation of striatal dopamine D2 receptors in advanced Parkinson’s disease contributes to the development of motor fluctuation. European Neurology. 2002;47(2):113–117. doi: 10.1159/000047962. [DOI] [PubMed] [Google Scholar]
- 94.Morrish PK, Sawle GV, Brooks DJ. Regional changes in [18F]dopa metabolism in the striatum in Parkinson’s disease. Brain. 1996;119, part 6:2097–2103. doi: 10.1093/brain/119.6.2097. [DOI] [PubMed] [Google Scholar]
- 95.Ito K, Morrish PK, Rakshi JS, et al. Statistical parametric mapping with 18F-dopa PET shows bilaterally reduced striatal and nigral dopaminergic function in early Parkinson’s disease. Journal of Neurology Neurosurgery and Psychiatry. 1999;66(6):754–758. doi: 10.1136/jnnp.66.6.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Koch W, Hamann C, Radau PE, Tatsch K. Does combined imaging of the pre- and postsynaptic dopaminergic system increase the diagnostic accuracy in the differential diagnosis of parkinsonism? European Journal of Nuclear Medicine and Molecular Imaging. 2007;34(8):1265–1273. doi: 10.1007/s00259-007-0375-8. [DOI] [PubMed] [Google Scholar]
- 97.Morrish PK, Sawle GV, Brooks DJ. Clinical and [(18F)]dopa PET findings in early Parkinson’s disease. Journal of Neurology Neurosurgery and Psychiatry. 1995;59(6):597–600. doi: 10.1136/jnnp.59.6.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hindle JV. Ageing, neurodegeneration and Parkinson’s disease. Age and Ageing. 2010;39(2):156–161. doi: 10.1093/ageing/afp223. [DOI] [PubMed] [Google Scholar]
- 99.Booij J, Berendse HW. Monitoring therapeutic effects in Parkinson's disease by serial imaging of the nigrostriatal dopaminergic pathway. Journal of the Neurological Sciences. 2011;310(1-2):40–43. doi: 10.1016/j.jns.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 100.Isaias IU, Benti R, Cilia R, et al. [123I]FP-CIT striatal binding in early Parkinson’s disease patients with tremor vs. akinetic-rigid onset. NeuroReport. 2007;18(14):1499–1502. doi: 10.1097/WNR.0b013e3282ef69f9. [DOI] [PubMed] [Google Scholar]
- 101.Buchert R, Berding G, Wilke F, et al. IBZM tool: a fully automated expert system for the evaluation of IBZM SPECT studies. European Journal of Nuclear Medicine and Molecular Imaging. 2006;33(9):1073–1083. doi: 10.1007/s00259-006-0067-9. [DOI] [PubMed] [Google Scholar]
- 102.Fukuyama H. Is 123I-MIBG cardiac scintigraphy a surrogate marker for Parkinson’s disease? European Journal of Nuclear Medicine and Molecular Imaging. 2010;37(1):1–2. doi: 10.1007/s00259-009-1215-9. [DOI] [PubMed] [Google Scholar]


