Abstract
Interindividual variability in protein expression of organic anion-transporting polypeptides (OATPs) OATP1B1, OATP1B3, OATP2B1, and multidrug resistance-linked P-glycoprotein (P-gp) or ABCB1 was quantified in frozen human livers (n = 64) and cryopreserved human hepatocytes (n = 12) by a validated liquid chromatography tandem mass spectroscopy (LC-MS/MS) method. Membrane isolation, sample workup, and LC-MS/MS analyses were as described before by our laboratory. Briefly, total native membrane proteins, isolated from the liver tissue and cryopreserved hepatocytes, were trypsin digested and quantified by LC-MS/MS using signature peptide(s) unique to each transporter. The mean ± S.D. (maximum/minimum range in parentheses) protein expression (fmol/µg of membrane protein) in human liver tissue was OATP1B1- 2.0 ± 0.9 (7), OATP1B3- 1.1 ± 0.5 (8), OATP2B1- 1 1.7 ± 0.6 (5), and P-gp- 0.4 ± 0.2 (8). Transporter expression in the liver tissue was comparable to that in the cryopreserved hepatocytes. Most important is that livers with SLCO1B1 (encoding OATP1B1) haplotypes *14/*14 and *14/*1a [i.e., representing single nucleotide polymorphisms (SNPs), c.388A > G, and c.463C > A] had significantly higher (P < 0.0001) protein expression than the reference haplotype (*1a/*1a). Based on these genotype-dependent protein expression data, we predicted (using Simcyp) an up to ∼40% decrease in the mean area under the curve of rosuvastatin or repaglinide in subjects harboring these variant alleles compared with those harboring the reference alleles. SLCO1B3 (encoding OATP1B3) SNPs did not significantly affect protein expression. Age and sex were not associated with transporter protein expression. These data will facilitate the prediction of population-based human transporter-mediated drug disposition, drug-drug interactions, and interindividual variability through physiologically based pharmacokinetic modeling.
Introduction
Hepatic transporters, present at the sinusoidal or canalicular membrane, can determine the plasma concentration of drugs by affecting their metabolic or biliary clearance (Backman et al., 2002; Schneck et al., 2004; Shitara et al., 2004, 2006; Giacomini et al., 2010; Schipani et al., 2012). Consequently, these transporters can affect the efficacy (Bailey et al., 2010; Tomlinson et al., 2010) and toxicity (Alexandridis et al., 2000; Bosch Rovira et al., 2001; Marsa Carretero et al., 2002) of drugs by modulating their exposure to the target sites (Harwood et al., 2013). Hence, it is important to delineate the role of hepatic transporters in drug disposition and local tissue drug exposure, particularly because plasma drug concentrations are generally used as a surrogate measure of tissue concentrations to describe pharmacokinetic-pharmacodynamic relationships and to predict drug-drug interactions (DDIs) or drug-gene interactions (Lon et al., 2012; Harwood et al., 2013). To achieve these goals on a population basis, physiologically based pharmacokinetic (PBPK) models (e.g., Simcyp) are increasingly being used in drug development and pharmaceutical research (Varma et al., 2012, 2013). For drugs where transporters are involved in their disposition, successful use of PBPK models requires critical information on the tissue localization and expression of the transporters, including the effect of covariates, like genotype, age, and sex, on transporter expression (Deo et al., 2012; Chu et al., 2013; Harwood et al., 2013; Prasad et al., 2013). However, such data are currently not available. Here we report protein quantification data on the hepatic transporters as a start to fill this crucial knowledge gap.
Recent US Food and Drug Administration draft guidance on pharmacokinetic DDIs (http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm292362.pdf) has highlighted the clinical importance of hepatic organic anion-transporting polypeptide transporters (OATPs), ABC drug transporter ABCB1 or P-glycoprotein (P-gp), and breast cancer resistant protein (BCRP or ABCG2) because of their broad substrate specificity and the potential to be involved in DDIs. We (Deo et al., 2012; Prasad et al., 2013) and others (Balogh et al., 2012; Bi et al., 2012; Kimoto et al., 2012; Ohtsuki et al., 2012; Schaefer et al., 2012; Tucker et al., 2012) have reported data on the expression of some of these hepatic transporters. Here we extended these studies to determine 1) the interindividual variability in expression of OATP1B1 (SLCO1B1), OATP1B3 (SLCO1B3), OATP2B1 (SLCO2B1), and P-gp (ABCB1) in a large set (n = 64) of human liver samples; and 2) the influence of genotype, age, and sex on such expression.
Materials and Methods
Chemicals and Reagents.
The ProteoExtract native membrane protein extraction kit was procured from Calbiochem (Temecula, CA). The protein quantification bicinchoninic acid (BCA) kit and the in-solution trypsin digestion kit were purchased from Pierce Biotechnology (Rockford, IL). Synthetic signature peptides (Table 1) for OATP1B1, OATP1B3, OATP2B1, and P-gp were obtained from New England Peptides (Boston, MA). The corresponding stable isotope-labeled (SIL) internal standards were obtained from Thermo Fisher Scientific (Rockford, IL). High-performance liquid chromatography–grade acetonitrile was purchased from Fischer Scientific (Fair Lawn, NJ), and formic acid was purchased from Sigma-Aldrich (St. Louis, MO). All reagents were analytical grade.
TABLE 1.
Multiple reaction monitoring parameters of peptides selected for targeted analysis of OATP1B1, OATP1B3, OATP2B1, and P-gp
Labeled amino acid residues are shown in bold and italic.
| Transporter | Peptide | Residues | Parent Ion (z = 2) | Product Ions |
(z = 1) |
Frag (V) | CE (eV) | |
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||||
| OATP1B1 (Peptide 1) | NVTGFFQSFK | 321–330 | 587.9 | 961.4 | 860.5 | 803.2 | 125 | 13 |
| NVTGFFQSFK | 591.9 | 969.5 | 868.5 | 811.2 | 125 | 14 | ||
| OATP1B1 (Peptide 2) | YVEQQYGQPSSK | 362–373 | 707.5 | 766.5 | 418.3 | 1152.5 | 155 | 22 |
| YVEQQYGQPSSK | 711.5 | 774.5 | 426.3 | 1160.5 | 155 | 22 | ||
| OATP1B3 (Peptide 1) | NVTGFFQSLK | 321–330 | 570.8 | 927.5 | 826.3 | 622.3 | 130 | 14 |
| NVTGFFQSLK | 574.8 | 935.6 | 834.3 | 630.3 | 130 | 14 | ||
| OATP1B3 (Peptide 2) | IYNSVFFGR | 615–623 | 551.8 | 826.5 | 712.5 | 526.6 | 135 | 13 |
| IYNSVFFGR | 556.8 | 836.6 | 635.2 | 536.6 | 135 | 13 | ||
| OATP2B1 (Peptide 1) | VLAVTDSPAR | 314–323 | 514.8 | 816.4 | 846.4 | 745.3 | 130 | 13 |
| VLAVTDSPAR | 519.9 | 826.4 | 856.4 | 755.3 | 125 | 13 | ||
| OATP2B1 (Peptide 2) | SSPAVEQQLLVSGPGK | 687–702 | 799.0 | 712.3 | 1026.3 | 1155.3 | 180 | 20 |
| SSPAVEQQLLVSGPGK | 803.0 | 1163.3 | 1034.3 | 715.9 | 180 | 20 | ||
| P-gp (Peptide 1) | NTTGALTTR | 809–817 | 467.8 | 618.3 | 719.4 | 820.5 | 125 | 12 |
| NTTGALTTR | 472.8 | 628.3 | 729.5 | 830.5 | 125 | 12 | ||
| P-gp (Peptide 2) | IATEAIENFR | 896–905 | 582.3 | 749.5 | 678.5 | 979.5 | 130 | 16 |
| IATEAIENFR | 587.3 | 759.5 | 688.5 | 989.5 | 130 | 16 | ||
CE, collision energy; Frag, fragmentor; OATP, organic anion-transporting polypeptide; P-gp, P-glycoprotein.
Human Liver Samples and Hepatocytes.
Sixty-four liver tissue samples from the human liver bank of the School of Pharmacy, University of Washington (UW), were used. Most of the subjects were Caucasian [except one Asian male (HL165) and three Black males not of Hispanic origin (HL104, 105, and 137)]; the subjects’ ages ranged from 7 to 70 years and comprised 30 females and 34 males. Procurement (approved by the UW Human Subjects Division), characteristics, and storage of these samples have been previously described (Paine et al., 1997), and additional details are provided in Supplemental Table 1. Most of these livers were obtained from organ donors who met with accidental death (e.g., trauma from vehicular accidents, subarachnoid hemorrhage, cerebrovascular accident) and were harvested from breathing donors who were perfused with UW solution for organ transplant purposes. Most of the subjects were not taking any chronic medication but did receive medication in the intensive care unit before tissue harvest. Cryopreserved human hepatocytes (seven batches of individual and five batches of pooled hepatocytes) (Table 2) were procured commercially from Celsis IVT (London, UK), Xenotech (Lenexa, KS), Life Technologies (Carlsbad, CA), and BD Gentest (San Jose, CA).
TABLE 2.
Characteristics of cryopreserved hepatocytes purchased from commercial sources
| Lot No. | Source | Sex | Age (yr) | Race | No. of subjects |
|---|---|---|---|---|---|
| AZL | Celsis IVT | NA | 33–88 | 18 C, 1 B, 1 H | 20 |
| PQP | Celsis IVT | 10 M, 10 F | 17-75 | 16 C, 2 B, 2 H | 20 |
| OFY | Celsis IVT | 17–65 | 8 C, 1 B, 1 H | 10 | |
| IRK | Celsis IVT | 5 M, 5 F | 19–80 | 9 C, 1 B | 10 |
| UMJ | Celsis IVT | 5 M, 5 F | 2–76 | 9 C, 1 H | 10 |
| Hu4193 | Invitrogen | M | 42 | C | 1 |
| 4524339002 | BD Gentest | F | 64 | C | 1 |
| 305 | BD Gentest | M | 67 | C | 1 |
| 4535888003 | BD Gentest | M | 14 | C | 1 |
| 4534583002 | BD Gentest | M | 11 (mo) | H | 1 |
| 512 | Xenotech | F | 62 | C | 1 |
| 706 | Xenotech | F | 53 | C | 1 |
B, Black; C, Caucasian; F, female; H, Hispanic; IVT, In Vitro Technology; M, male; NA, not available.
Membrane Protein Extraction and Total Protein Quantification.
The liver tissue (∼100 mg) was processed, as we have described before, to isolate total membrane proteins (Calbiochem) (Deo et al., 2012; Prasad et al., 2013). Briefly, the tissue was homogenized in 2 ml of extraction buffer I (ProteoExtract native membrane protein extraction kit) containing protease inhibitor cocktail (10 µl) of the kit and incubated with gentle shaking for 10 minutes. The resultant homogenate was centrifuged at 16,000g for 15 minutes, and the supernatant was discarded. The pellet was resuspended in 1 ml of extraction buffer II of the kit with 10 µl of protease inhibitor cocktail. The latter was incubated with gentle shaking for 30 minutes at 4°C followed by centrifugation at 16,000g for 15 minutes at 4°C. Total isolated membrane protein concentration (i.e., the supernatant) was determined using the BCA protein assay kit. The supernatant was diluted to a working concentration of 2 µg of protein per microliter or lower. Similar to the tissues, the pellet of cryopreserved hepatocytes (2–5 × 106 cells) were processed as discussed except the cells were washed twice with washing solution of the kit before the addition of 2 ml of extraction buffer I. The remaining procedure was the same as described for the liver tissue.
Purification of Human Pgp.
Human Pgp from crude membranes of High Five insect cells was purified as described previously (Sauna et al., 2006) with some modifications. Briefly, the crude membranes were solubilized with n-dodecyl-β-d-maltoside (DDM) (1.00% w/v) in the presence of 20% glycerol. Solubilized proteins were subjected to metal affinity chromatography (Ni-NTA resin; Qiagen Inc, Valencia, CA) in the presence of 0.51 mM DDM; purified P-gp was eluted with 200 mM imidazole. The eluate was further purified by gel filtration chromatography using Superdex S-200 column to remove imidazole. The fractions containing P-gp were then concentrated using Amicon ultrafiltration concentrators with 100 KDa cutoff (EMD Millipore, Billerica, MA) to ∼0.5–1.5 mg/ml and stored at −70°C. The protein concentration was quantified using the BCA protein assay kit as per the manufacturer’s instructions.
Peptide Selection, Trypsin Digestion of Membrane Proteins, and Sample Preparation.
Two unique signature peptides (not present in any other known protein) were selected for quantification of each transporter (Table 1) based on previously reported criteria (Kamiie et al., 2008) and literature reports (Zhang et al., 2011; Balogh et al., 2012). Briefly, peptides with transmembrane regions, single nucleotide polymorphisms (SNPs), posttranslational modifications, or those susceptible to degradation were not selected. Continuous R and K sequences (RR, RK, KR, and KK) were excluded to avoid the miscleavages by trypsin. The length of selected peptides was between 9 and 16 amino acid residues. Selected signature peptides were NVTGFFQSFK/YVEQQYGQPSSK (OATP1B1), NVTGFFQSLK/ IYNSVFFGR (OATP1B3), VLAVTDSPAR/SSPAVEQQLLVSGPGK (OATP2B1), and NTTGALTTR/IATEAIENFR (P-gp). The corresponding peptides containing labeled [13C615N2]-lysine and [13C615N4]-arginine residues were used as the internal standards.
Trypsin digestion conditions were optimized for time (24 hours) and protein:trypsin ratio (25:1; w/w), and 20 µl of 2.0 µg/µl (or lower concentration) of tissue membrane preparation was incubated with 4 µl of dithiothreitol (100 mM) and 4 µl of iodoacetamide (200 mM) in 10 µl of ammonium bicarbonate digestion buffer (50 mM, pH 7.8). The protein samples were digested by trypsin in a final volume of 60 µl at 37°C for 24 hours, and the reaction was quenched by 20 µl of SIL peptide internal standard cocktail (prepared in 70% acetonitrile in water containing 0.1% formic acid) and 10 µl of the neat quenching solvent. The samples were centrifuged at 4000g for 5 minutes. For calibration standards, the working solution (10 µl) of the standard cocktail was added in the last step instead of the neat quenching solvent.
Analytical Method Parameters.
Agilent 6460A triple-quadrupole mass spectrometer coupled to Agilent 1290 Infinity LC system (Agilent Technologies, Santa Clara, CA) operated in electrospray ionization positive ionization mode was used for liquid chromatography-tandem mass spectroscopy (LC-MS/MS) analysis of the signature peptides. Approximately 2 µg or less of the trypsin digest (5 µl) was injected onto the column (Kinetex 2.6 µm, C18, 100 × 3 mm, Phenomenex, Torrance, CA) and eluted at 0.4 ml/min. The mobile-phase gradient conditions were 97% A (water containing 0.1% v/v formic acid) and 3% B (acetonitrile containing 0.1% v/v formic acid) held for 4 minutes, followed by seven steps of linear gradient of mobile phase B concentration of 3%–12.5%, 12.5%–18%, 18%–19.5%, 19.5% –20%, 20%–35%, 35%–50%, and 50%–90% over 4–8 minutes, 8–11 minutes, 11–13.5 minutes, 13.5–16 minutes, 16–18 minutes, 18–18.4 minutes, and 18.4–18.6 minutes, followed by the washing step using 90% mobile phase B for 1.6 minutes, and re-equilibration for 4.8 minutes. The doubly charged parent to singly charged product transitions for the analyte peptides and their respective SIL peptides were monitored using optimized LC-MS/MS parameters (Table 1).
The calibration curve standards were prepared by spiking peptide standards into the extraction buffer II of the membrane protein extraction kit. Seven calibration concentrations ranging from ∼0.2 to 20.0 fmol (on column) were used. The analytical method was validated for accuracy, interday and intraday precision, and stability (freeze and thaw, bench-top, and autosampler conditions) as we have described previously (Prasad et al., 2013). The quality control samples prepared by spiking extraction buffer II or pooled human liver membrane were quantified after every 12–15 samples. In addition, the reliability of surrogate peptide-based LC-MS/MS protein quantification was validated using the only purified transporter available to us, namely P-gp. Four different concentrations of P-gp protein standard (2.2, 4.4, 17.7, and 35.3 fmol, on-column) were prepared as quality control samples and were then processed, as were the membrane extracts of the liver tissues. The data were processed by integrating the peak areas generated from the reconstructed ion chromatograms for the analyte peptides and their respective internal standards using the MassHunter software (Agilent Technologies). For quantification of samples or standards, peak response from the two transitions from each peptide was averaged.
Genotyping and Genotype-Dependent Changes on Protein Expression.
Genotyping data were kindly provided by Dr. Yvonne Lin, Department of Pharmaceutics, University of Washington. Briefly, genomic DNA was extracted from liver tissues. The genotype analysis was done using Affymetrix DMET Plus Array (Santa Clara, CA) according to the manufacturer’s protocol. Individual genotypes were resolved, and the minor allele frequencies were determined using the Affymetrix DMET Plus console (version 1.1) using the Dynamic Genotype Boundaries algorithm. Unpaired t test was used to compare protein expression observed in two genotypic groups. When comparing protein expression in three or more groups, the Bonferroni multiple comparison correction was applied.
PBPK Simulations.
The effect of SLCO1B1 polymorphism on the pharmacokinetics of OATP1B1 substrates rosuvastatin and repaglinide was predicted using the population-based ADME simulator of Simcyp (version 12.0, SimCYP Ltd, Sheffield, UK). The rosuvastatin and repaglinide parameters of Simcyp library file were used as such except that the relative expression factor (see Supplemental Table 2) of OATP1B1 was varied for a given genotype or haplotype compared with the default SimcyP value for wild-type (set at 1). The 90% confidence intervals (CIs) of mean relative expression factors were used to estimate population variability in each group (see Supplemental Table 2). Expression of other transporters (i.e., OATP1B3, OATP2B1, BCRP, and sodium-taurocholate cotransporting polypeptide (NTCP)) was assumed constant for all simulations. Data for 16 subjects (70 kg; age 18–65 years, proportion of females: 0.5) given a single dose of rosuvastatin (20 mg) or repaglinide (0.50 mg) were simulated (four trials × 4 subjects).
Results
Analytical Methods.
The calibration curves were linear across the calibration range ∼0.2–20.0 fmol (on column). The lower limit of quantification was between 0.1 and 0.3 fmol (on-column) for all the peptides (except YVEQQYGQPSSK, which had a lower limit of quantification of 1.2 fmol). Accuracy and precision in the quantification of the quality control samples were acceptable (CV <25%) at three different concentrations. Trypsin digestion of the transporters was maximized by monitoring the time at which there was no further increment in the yield of the peptide (data not shown). All the peptides were stable during sample preparation (i.e., when exposed to three cycles of freeze and thaw, at bench-top for 6 hours, and in an autosampler for 48 hours).
Using the purified P-gp, our peptide-based LC-MS/MS approach was able to recover the concentration of P-gp in the quality control samples with an accuracy of 124.0% ± 11.2% and 74.7% ± 4.1% using the P-gp surrogate peptides 1 and 2 (Table 1), respectively. For the remaining transporters, since purified protein standards are not available, the analytical method was based on the assumption that the proteins are completely digested by trypsin to their corresponding peptides and there is a complete extraction of membrane proteins from the tissue homogenate. Although we used two peptides to quantify each protein, only one peptide for OATP1B1, peptide 1, was detectable with acceptable sensitivity. For the remaining transporters, we observed a minor (up to 1.5-fold) but systematic difference (P < 0.05, paired t test, Table 3) in protein quantification between the two different signature peptides. We assume that this difference was due to different degrees of trypsin digestion. Therefore, the results reported here are based on the peptides that yielded higher protein expression, namely, NVTGFFQSFK (OATP1B1), NVTGFFQSLK (OATP1B3), VLAVTDSPAR (OATP2B1), and NTTGALTTR (P-gp). Nevertheless, our final conclusions about the effect of genotype, age, and sex on transporter expression were the same irrespective of the peptide used (see later).
TABLE 3.
Mean ± S.D. (range, i.e., maximum/minimum in parentheses) protein expression in human livers and human hepatocytes observed in this study (bolded) or reported by others
| No. of Samples | OATP1B1 | OATP1B3 | OATP2B1 | P-glycoprotein | Reference |
|---|---|---|---|---|---|
| Liver tissue (fmol/µg membrane protein) | |||||
| 64 (Peptide 1) | 2.0 ± 0.9 (7) | 1.1 ± 0.5 (8) | 1.7 ± 0.6 (5) | 0.4 ± 0.2 (8) | This study |
| 64 (Peptide 2) | NQ | 0.9 ± 0.4 (8) | 1.5 ± 0.6 (6) | 0.3 ± 0.2 (7) | This study |
| 17 | 2.7 ± 3.7* | 1.7 ± 0.5 | 0.5 ± 0.9 | 1.5 ± 0.4 | (Ohtsuki et al., 2012) |
| 9 | 9.7 ± 4.3 | 6.3 ± 2.8 | 3.7 ± 1.4 | NQ | (Kimoto et al., 2012) |
| 13 | NQ | NQ | NQ | 0.7 ± 0.3 | (Tucker et al., 2012) |
| 12 | 7.2 ± 0.3 | 6.3 ± 0.4 | 4.0 ± 0.4 | NQ | (Karlgren et al., 2012) |
| 4 | 10.6 ± 4.6 | 5.9 ± 3.8 | 2.9 ± 1.3 | NQ | (Balogh et al., 2012) |
| Cryopreserved suspended hepatocytes | |||||
| 12$ | 2.4 ± 0.5 (2) | 0.9 ± 0.5 (5) | 1.7 ± 0.5 (3) | 0.5 ± 0.1 (4) | This study |
| 12 | NQ | 0.7 ± 0.3 (4) | 1.3 ± 0.5 (3) | 0.4 ± 0.1 (4) | This study |
| 14 | 4.9 ± 1.9 | 1.7 ± 0.6 | 1.6 ± 0.5 | NQ | (Kimoto et al., 2012) |
| 1 | 5.8 | 5.8 | 4.1 | NQ | (Ji et al., 2012) |
| 1 | 3.4 | 1.5 | 1.8 | NQ | (Bi et al., 2012) |
| Sandwich-cultured hepatocytes | |||||
| 3 | 5.4 ± 1.0 | 4.3 ± 0.2 | 2.9 ± 2.5 | 13.9 ± 11.8 | (Schaefer et al., 2012) |
| 5 | 5.8 ± 3.3 | 0.8 ± 0.3 | 1.0 ± 0.2 | NQ | (Kimoto et al., 2012) |
| 1 | 5.3 | 0.9 | 1.2 | NQ | (Bi et al., 2012) |
NQ, not quantified.
OATP1B1 was detected in only eight liver tissue samples.
Seven batches of individual and five batches of pooled hepatocytes (see Table 2).
Interindividual Variability in Transporter Expression in Human Livers and Cryopreserved Human Hepatocytes.
Our yield of total membrane protein was 3.7 ± 1.1 mg/100 mg tissue. The expression of OATPs and P-gp in tissue samples was comparable to that observed in the cryopreserved hepatocytes (Table 3). Similar to human liver tissue, the expression of these transporters in hepatocytes were in the order of OATP1B1 > OATP2B1 > OATP1B3 > P-gp. Interindividual variability, calculated as the -fold range in transporter expression (i.e., maximum or minimum expression) was 5- to 8-fold (see Fig. 1). Expression of all the transporters was independent of age (Fig. 2) or sex (Fig. 3).
Fig. 1.
Interindividual variability and mean ± S.D. (last bar) in hepatic protein expression of OATP1B1 (A), OATP1B3 (B), OATP2B1 (C), or P-gp (D) in liver samples.
Fig. 2.
Hepatic protein expression of OATP1B1 (A), OATP1B3 (B), OATP2B1 (C), or P-gp (D) does not correlate with age (P < 0.05).
Fig. 3.
Hepatic protein expression of OATP1B1 (A), OATP1B3 (B), OATP2B1 (C), or P-gp (D) is not dependent on sex.
Effect of Genotype on Hepatic Transporter Protein Expression.
Reported SNPs of all transporters (except SLCO2B1) were observed in our liver bank (Table 4). Among the OATPs, only OATP1B1 expression was genotype-dependent. When analyzed individually (without regard to haplotypes), livers homozygous for the nonsynonymous SLCO1B1 SNPs, c.388A>G or c.463C>A, or the synonymous SNP, c.597C>T, expressed 1.8-, 2.1-, and 1.7-fold higher OATP1B1 protein than those with the corresponding wild-type allele, respectively (P < 0.0001) (Fig. 4). Moreover, livers that were heterozygous for c.463CA had higher OATP1B1 expression than the wild-type livers (P < 0.0001), and the expression in the former was comparable to that in homozygous livers, c.463AA (Fig. 4). The expression of OATP1B1 in livers carrying a single c.388AG, c.597CT, c.571TT, c.571TC, or -1187GA allele was not significantly different from the wild-type livers. Only one liver in our tissue bank was homozygous for the functionally relevant SNP c.521T>C. The expression of OATP1B1 in livers with c.521TT versus 521TC was not significantly different (Fig. 4).
TABLE 4.
Frequency of OATP1B1, OATP1B3, and P-gp SNPs detected in the University of Washington (UW) liver bank
| Marker ID | Variant | Change for Variant | Frequency in UW liver Bank |
||
|---|---|---|---|---|---|
| Homozygous Variant | Heterozygous Variant | Wild-Type | |||
| OATP1B1 | |||||
| rs4149015 | −11187G>A | Promoter | 0 | 9 | 53 |
| rs2306283 | 388A>G | N130D | 10 | 30 | 22 |
| rs11045819 | 463C>A | P155T | 4 | 9 | 49 |
| rs4149056 | 521T>C | V174A | 1 | 21 | 40 |
| rs4149057 | 571T>C | L191L | 16 | 34 | 12 |
| rs2291075 | 597C>T | F199F | 10 | 33 | 19 |
| OATP1B3 | |||||
| rs4149117 | 334G>T | A112S | 0 | 45 | 17 |
| rs7311358 | 699A>G | I233M | 0 | 45 | 17 |
| rs2053098 | 1557G>A | A519A | 0 | 45 | 17 |
| rs3764006 | 1833A>G | G611G | 0 | 42 | 20 |
| P-gp | |||||
| rs2214102 | −1G>A | 5′UTR | 0 | 6 | 56 |
| rs2235015 | 287-25G>T | Intron | 0 | 19 | 43 |
| rs10276036 | IVS9-44A>G | Intron | 19 | 31 | 12 |
| rs1128503 | 1236C>T | G412G | 18 | 33 | 11 |
| rs2032588 | 1350+44C>T | Intron | 0 | 7 | 55 |
| rs2235033 | 1554+24C>T | Intron | 22 | 32 | 8 |
| rs2235013 | 1725+38A>G | Intron | 21 | 33 | 8 |
| rs9282564 | 61A>G | N21D | 7 | 11 | 45 |
| rs2235040 | 2481+24G>A | Intron | 0 | 12 | 50 |
| rs2032582 | 2677G>T, 2677G>A | A893S, A893T | 17 | 32 | 13 |
| rs3213619 | −129T>C | 5′UTR | 0 | 4 | 58 |
| rs1045642 | 3435C>T | I1145I | 22 | 30 | 10 |
| rs17064 | *89A>T | 3′UTR | 0 | 7 | 55 |
| rs3842 | *193A>G | 3′UTR | 0 | 18 | 44 |
OATP, organic anion-transporting polypeptide; P-gp, P-glycoprotein; SNP, single nucleotide polymorphisms; UW, University of Washington.
OATP2B1 SNPs, rs59305495, rs72559740, rs1109407, rs1621378, and rs2306167 were not found in the UW liver bank. All other SNPs available in the Affymetrix DMET Plus array for OATP1B1, OATP1B3, and P-gp were not observed.
Fig. 4.
OATP1B1 protein expression based on individual alleles (% frequencies in parentheses). Horizontal line: median; +: mean value; boxes: 25th–75th percentiles; whiskers: nonoutlier range. Same letters indicate significant difference; P < 0.0001 (a, b), P < 0.005 (c).
In agreement with other studies (Kalliokoski et al., 2008a; Nies et al., 2013), we observed significant linkage disequilibrium among the above SNPs. Therefore, we examined the expression of OATP1B1 based on SLCO1B1 haplotypes of the three previously described key variants (c.388A>G, c.463C>A, and 521T>C; Fig. 5A). Hepatic OATP1B1 protein expression was significantly higher (P < 0.0001) in livers with SLCO1B1 haplotypes *14/*1a and *14/*14 compared with those harboring the reference allele (i.e., *1a/*1a), *15/*1a or *1b/*1a (Fig. 5B). The carriers of haplotypes *14/*1a and *14/*14 had, respectively, 1.9- and 2.2-fold higher OATP1B1 expression than those carrying the reference allele. Furthermore, livers homozygous for c.388A>G independently increased OATP1B1 protein expression even when carriers of both 463AC and 463AA were excluded (Fig. 5C). SNPs c.388A>G and c.521T>C show the opposite effect on the pharmacokinetics of a number of drugs (Niemi et al., 2004; Kameyama et al., 2005; Hartkoorn et al., 2010; Rodrigues et al., 2011; Schipani et al., 2012; Sortica et al., 2012; Nies et al., 2013). In agreement with these observations, when homozygous alleles of 388A>G were excluded from analysis, we observed a modest but statistically significant (P < 0.05) decrease in OATP1B1 expression in individuals with c.521TC versus c.521TT (Fig. 5C). An independent effect of SNP c.521CC (*5) could not be examined because of its low frequency in our liver bank.
Fig. 5.
(A) SLCO1B1 haplotype classification based on the presence of the three previously described key variants. (B) Hepatic OATP1B1 protein expression is haplotype-dependent. SLCO1B1 haplotype (% frequencies in parentheses) are arranged by median OATP1B1 protein expression. (C) When carriers of c.388GG were excluded, OATP1B1 protein expression in livers harboring c.521TC allele was moderately but significantly lower than those harboring the TT allele. OATP1B1 protein expression in livers harboring c.388GG (but not SNP c.463CA or AA) was moderately but significantly higher than those harboring the AA allele. Horizontal line: median; +: mean; boxes: 25th–75th percentiles; whiskers: nonoutlier range. Same letters indicate significant difference; P < 0.0001 (a, b, c, d, e, f) and P < 0.05 (g).
Subjects harboring SLCO1B3 haplotype (c.334G>T, c.699A>G, c.1557G>A, and c.1833A>G) did not affect protein expression. Genotype-dependent protein expression could not be investigated for P-gp because of the large number of haplotypes, each with a limited sample size. Individually, none of the ABCB1 SNPs significantly affected protein expression (Table 4).
Quantitative Impact of OATP1B1 Polymorphism on Pharmacokinetics of Rosuvastatin and Repaglinide.
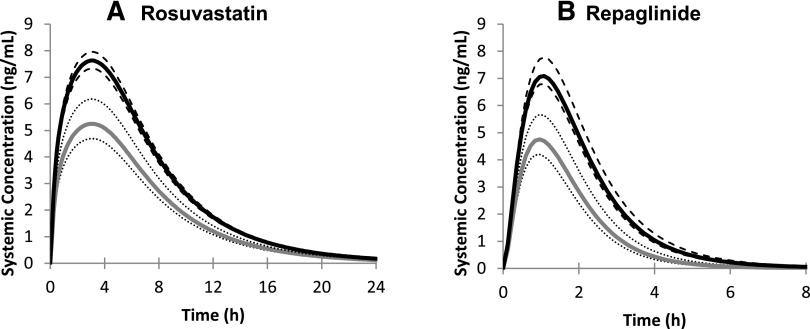
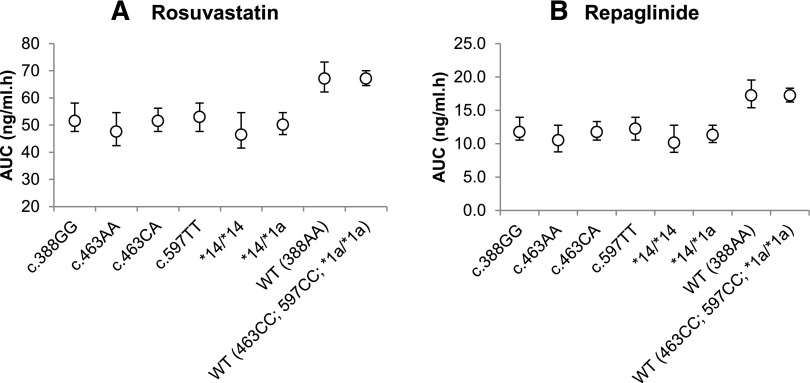
Utilizing the protein expression data (Figs. 4 and 5; see Supplemental Table 2), we predicted the impact of the SLCO1B1 genotypes on the human pharmacokinetics of OATP1B1 substrates rosuvastatin and repaglinide. In agreement with the expression data, the various genotypes and haplotypes of OATP1B1 had marked effects on the predicted plasma concentration-time profiles of the OATP1B1 substrates rosuvastatin and repaglinide (Fig. 6), translating into reductions in area under the curve (AUC) of up to 40% (Fig. 7) compared with the respective wild-type and reference allele.
Fig. 6.
Mean rosuvastatin (A) and repaglinide (B) plasma concentration-time profiles (po) in populations harboring OATP1B1 wild-type (*1a/*1a, black lines) or *14/*14 (gray lines) haplotypes. The 90% CIs around the mean are represented by the dashed and dotted lines respectively.
Fig. 7.
Simcyp predicted mean AUC of rosuvastatin (A) or repaglinide (B) in virtual populations harboring different SLCO1B1 genotypes or haplotypes. Error bars show 90% CIs around the mean.
Discussion
We quantified the interindividual variability in hepatic expression of OATP1B1, OATP1B3, OATP2B1, and P-gp in human livers (n = 64) and cryopreserved hepatocytes (n = 12) by LC-MS/MS. OATP and P-gp expression was measureable in all samples. Consistent with data published by others (Nies et al., 2013), the expression of none of the studied transporters in our liver bank was age (7–70 years) or sex dependent. Since primary human hepatocyte suspension is used to predict the contribution of OATPs to hepatic uptake of drugs in humans, it is interesting to note that the expression of OATPs in human livers was similar to that in cryopreserved hepatocytes (Table 3). However, the expression of MRP2 and BCRP was significantly different (1.54 ± 0.64 vs. 0.56 ± 0.21 and 0.14 ± 0.04 vs. 0.70 ± 0.22 fmol/µg membrane protein, respectively; P < 0.0001) (Deo et al., 2012; Prasad et al., 2013). Collectively, our transporter data are comparable or modestly lower than those reported previously in a much smaller sample size (Balogh et al., 2012; Bi et al., 2012; Karlgren et al., 2012; Kimoto et al., 2012; Ohtsuki et al., 2012; Tucker et al., 2012). Based on Western blotting, interindividual variability in OATP1B1, OATP1B3, OATP2B1, and P-gp expression have been reported to be 19, 85, 17 (n = 117), and 20-fold (n = 110), respectively (Meier et al., 2006; Nies et al., 2013). Possible reasons for the differences in absolute expression values are differences in the method of tissue procurement (organ donors vs. resections from diseased livers), subject demographics, the membrane fractionation method used, the protein quantification method used (LC-MS/MS vs. immunoblotting), peptides quantified, sample preparation, or variation in trypsin digestion efficiencies. Since pure protein standards of the transporters measured are not readily available, the limitation of the peptide-based LC-MS/MS quantification methods of assuming 100% trypsin digestion could be an additional factor. However, since we validated our P-gp expression values using purified human P-gp, these values are not confounded by any issues regarding methods.
In agreement with clinical data on the effect of genotypes on in vivo activity of OATP1B1 (Mwinyi et al., 2004; Niemi et al., 2004; Voora et al., 2009; Rodrigues et al., 2011; Schipani et al., 2012; Sortica et al., 2012), we observed that protein expression of OATP1B1 was genotype dependent. SNP c.463C>A is reported to increase lopinavir clearance by 2-fold, possibly as a result of increased OATP1B1 activity (Hartkoorn et al., 2010). Consistent with this observation, we noted that livers homozygous or heterozygous for this variant contained 2-fold higher amounts of OATP1B1 than livers with wild-type alleles. Similarly, SNP c.388A>G increased OATP1B1 expression in human livers compared with the wild-type alleles. Clinically, this variant not only increases the clearance of OATP1B1 substrate drugs (e.g., statins) (Mwinyi et al., 2004; Nies et al., 2013) but also increases the efficacy (Rodrigues et al., 2011; Sortica et al., 2012) and reduces the toxicity of statins (Donnelly et al., 2011).
The preceding analysis did not take into consideration the high degree of linkage disequilibrium between OATP1B1 SNPs. Nies and colleagues recently reported that SLCO1B1 haplotype *14/*14 is correlated with 28% decrease in atorvastatin AUC relative to the reference allele (*1a/*1a); OATP1B1 protein levels were 2-fold higher in individuals with the *14/*1a haplotype (Nies et al., 2013). Consistent with this report, we observed that OATP1B1 expression in livers with the *14/*14 haplotype was 2.2-fold higher than that in livers with the reference haplotype (*1a/*1a). Similarly, consistent with previous data (Nies et al., 2013), livers with haplotype *14/*1a resulted in 1.9-fold higher protein expression. We found that the change in OATP1B1 expression was more pronounced with the 388GG allele versus the AG allele (Figs. 4 and 5). The presence of c.388GG, but not c.463AA or AC, resulted in a modestly higher OATP1B1 expression than the reference allele (*1a/*1a) despite the presence of c.521TC allele, which is known to reduce OATP activity and expression (Fig. 5).
OATP1B1 SNP c.521T>C variant is linked to decreased clearance of OATP1B1 substrates (Niemi et al., 2004; Kalliokoski et al., 2008b; Hartkoorn et al., 2010) and is associated with statin-mediated myopathy (Link et al., 2008; Voora et al., 2009). In vitro cell surface biotinylation experiments by Tirona et al. (2001) showed that the altered transport activity of the c.521T>C variant, for estrone-3-sulfate or estradiol-17-d-glucuronide, was due to decreased plasma membrane expression of the transporter. Although all livers in our liver bank harboring individual SNP c.521TC were not different from wild-type, expression of OATP1B1 was modestly decreased in carriers of SNP c.521TC versus c.521TT when livers harboring c.388GG were excluded (Fig. 5C).
We observed that the synonymous SLCO1B1 SNP c.597C>T was associated with an increase of ∼1.7-fold in hepatic protein expression. However, it is important to note here that SNPs c.388A>G and c.597C>T showed a high degree of linkage disequilibrium; thus, this may not be an independent effect of the c.597C>T variant. Nevertheless, this observation highlights the fact that quantification of tissue transporter expression can result in the discovery of novel variants resulting in hypothesis-based clinical studies to determine the clinical significance of these variants.
Genetic polymorphism can affect the affinity of a substrate for a transporter (Km) or its maximal transport capacity (Vmax) or both. One factor that can affect Vmax is the magnitude of plasma membrane expression of the transporter. Although we measured total membrane expression of OATP1B1, we asked whether we could quantitatively predict the in vivo consequence of changes in the expression of the transporter using PBPK models. We assumed that OATP1B1 expression data for the various genotypes reflected a proportional change in the plasma membrane expression of the transporter. We predicted up to 40% decrease in the mean AUC of OATP1B1 substrates, rosuvastatin, and repaglinide for the various SLCO1B1 genotypes (Figs. 6 and 7; see Supplemental Table 2). Although the effect of most of these genotypes on the pharmacokinetics of these drugs remains to be tested in the clinic, where available, our predictions agreed with the observed data. For example, in agreement with the reported 32% decrease (P = 0.007) in mean AUC0-∞ (Kalliokoski et al., 2008a) of repaglinide in carriers of 388GG versus wild-type, we predicted that AUC changes from 17.2 (wild-type) to 11.8 ng/ml ⋅ h (388GG) (Fig. 7). The latter suggests that despite the fact that we measured the expression of the transporters in total membrane protein (and not specifically in the plasma membrane), we can predict the impact of OATP1B1 genotype on the in vivo disposition of OATP1B1 substrate drugs where the effect appears to occur primarily through change in protein expression. Our predictions also suggest that individuals with *14/*14 haplotypes will demonstrate the largest change in the pharmacokinetics of OATP1B1 substrate drugs.
In summary, LC-MS/MS is a sensitive, specific, simple, multiplex approach to measure simultaneously the interindividual variability in tissue expression of drug transporters. The data presented here, as well as those published previously (MRP2 and BCRP) (Deo et al., 2012; Prasad et al., 2013) in the same set of livers indicate that the interindividual variability in the expression of the major drug hepatic transporters is modest (4- to 8-fold). In addition, expression of these transporters is not associated with age (age 7–70 years) or sex. However, the expression of OATP1B1 was genotype-dependent. Our data indicate that measured expression of OATP1B1 in total membranes isolated from liver tissue (vs. plasma membrane) was predictive of the in vivo consequences of OATP1B1 genotype on drug pharmacokinetics. Collectively, the data presented here will potentially allow us to quantitatively predict transporter-based drug disposition and DDI through population PBPK modeling.
Supplementary Material
Acknowledgments
The authors thank Dr. Yvonne Lin, Department of Pharmaceutics, University of Washington, for genotyping data; Dr. Peggy Wong (Merck) for review of the statistical analysis; and Xiaoxin Cai and Dr. Xiaoyan Chu (Merck), Jen Harris and Rick Luzietti (AstraZeneca), and Johnathan Cheong (Genentech) for hepatocyte samples for several of the donors analyzed.
Abbreviations
- AUC
area under the curve
- BCA
bicinchoninic acid
- BCRP
breast cancer resistance protein
- CL
clearance
- DDI
drug-drug interactions
- LC-MS/MS
liquid chromatography tandem mass spectrometry
- MRM
multiple reaction monitoring
- MRP-2
multidrug resistance associated protein 2
- OATP
organic anion-transporting polypeptide
- P-gp
P-glycoprotein
- PBPK
physiologically based pharmacokinetics
- SIL
stable isotope label
- SNP
single nucleotide polymorphism
Authorship Contributions
Participated in research design: Prasad, Evers, Gupta, Salphati, Hop, Unadkat.
Conducted experiments: Prasad, Shukla.
Performed data analysis: Prasad, Unadkat.
Contributed new reagents or analytic tools: Evers, Gupta, Salphati, Hop, Shukla, Ambudkar.
Wrote or contributed to the writing of the manuscript: Prasad, Evers, Gupta, Salphati, Hop, Shukla, Ambudkar, Unadkat.
Footnotes
This study was supported by the University of Washington Research Affiliate Program on Transporters sponsored by AstraZeneca, Genentech, and Merck & Co., Inc. (http://sop.washington.edu/uwrapt). R.E. thanks the Merck Research Laboratories New Technologies Review and Licensing Committee for funding. A.G. thanks the AstraZeneca External Science Committee and licensing group for their support. S.S. and S.V.A were supported by the Intramural Research Program of the National Institutes of Health National Cancer Institute Center for Cancer Research (grant number ZIA BC010030-13).
 This article has supplemental material available at dmd.aspetjournals.org.
This article has supplemental material available at dmd.aspetjournals.org.
References
- Alexandridis G, Pappas GA, Elisaf MS. (2000) Rhabdomyolysis due to combination therapy with cerivastatin and gemfibrozil. Am J Med 109:261–262 [DOI] [PubMed] [Google Scholar]
- Backman JT, Kyrklund C, Neuvonen M, Neuvonen PJ. (2002) Gemfibrozil greatly increases plasma concentrations of cerivastatin. Clin Pharmacol Ther 72:685–691 [DOI] [PubMed] [Google Scholar]
- Bailey KM, Romaine SP, Jackson BM, Farrin AJ, Efthymiou M, Barth JH, Copeland J, McCormack T, Whitehead A, Flather MD, et al. SPACE ROCKET Trial Group (2010) Hepatic metabolism and transporter gene variants enhance response to rosuvastatin in patients with acute myocardial infarction: the GEOSTAT-1 Study. Circ Cardiovasc Genet 3:276–285 [DOI] [PubMed] [Google Scholar]
- Balogh LM, Kimoto E, Chupka J, Zhang H, Lai Y. (2012) Membrane protein quantification by peptide-based mass spectrometry approaches: studies on the organic anion-transporting polypeptide family. J Proteomics Bioinform 84:1–8 [Google Scholar]
- Bi YA, Kimoto E, Sevidal S, Jones HM, Barton HA, Kempshall S, Whalen KM, Zhang H, Ji C, Fenner KS, et al. (2012) In vitro evaluation of hepatic transporter-mediated clinical drug-drug interactions: hepatocyte model optimization and retrospective investigation. Drug Metab Dispos 40:1085–1092 [DOI] [PubMed] [Google Scholar]
- Bosch Rovira T, Llompart Pou JA, Forteza-Rey J. (2001) [Rhabdomyolysis associated with combined treatment of cerivastatin and gemfibrozil]. Rev Clin Esp 201:731–732 [DOI] [PubMed] [Google Scholar]
- Chu X, Bleasby K, Evers R. (2013) Species differences in drug transporters and implications for translating preclinical findings to humans. Expert Opin Drug Metab Toxicol 9:237–252 [DOI] [PubMed] [Google Scholar]
- Deo AK, Prasad B, Balogh L, Lai Y, Unadkat JD. (2012) Interindividual variability in hepatic expression of the multidrug resistance-associated protein 2 (MRP2/ABCC2): quantification by liquid chromatography/tandem mass spectrometry. Drug Metab Dispos 40:852–855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly LA, Doney AS, Tavendale R, Lang CC, Pearson ER, Colhoun HM, McCarthy MI, Hattersley AT, Morris AD, Palmer CN. (2011) Common nonsynonymous substitutions in SLCO1B1 predispose to statin intolerance in routinely treated individuals with type 2 diabetes: a go-DARTS study. Clin Pharmacol Ther 89:210–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacomini KM, Huang SM, Tweedie DJ, Benet LZ, Brouwer KL, Chu X, Dahlin A, Evers R, Fischer V, Hillgren KM, et al. International Transporter Consortium (2010) Membrane transporters in drug development. Nat Rev Drug Discov 9:215–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartkoorn RC, Kwan WS, Shallcross V, Chaikan A, Liptrott N, Egan D, Sora ES, James CE, Gibbons S, Bray PG, et al. (2010) HIV protease inhibitors are substrates for OATP1A2, OATP1B1 and OATP1B3 and lopinavir plasma concentrations are influenced by SLCO1B1 polymorphisms. Pharmacogenet Genomics 20:112–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwood MD, Neuhoff S, Carlson GL, Warhurst G, Rostami-Hodjegan A. (2013) Absolute abundance and function of intestinal drug transporters: a prerequisite for fully mechanistic in vitro-in vivo extrapolation of oral drug absorption. Biopharm Drug Dispos 34:2–28 [DOI] [PubMed] [Google Scholar]
- Ji C, Tschantz WR, Pfeifer ND, Ullah M, Sadagopan N. (2012) Development of a multiplex UPLC-MRM MS method for quantification of human membrane transport proteins OATP1B1, OATP1B3 and OATP2B1 in in vitro systems and tissues. Anal Chim Acta 717:67–76 [DOI] [PubMed] [Google Scholar]
- Kalliokoski A, Backman JT, Neuvonen PJ, Niemi M. (2008a) Effects of the SLCO1B1*1B haplotype on the pharmacokinetics and pharmacodynamics of repaglinide and nateglinide. Pharmacogenet Genomics 18:937–942 [DOI] [PubMed] [Google Scholar]
- Kalliokoski A, Neuvonen M, Neuvonen PJ, Niemi M. (2008b) The effect of SLCO1B1 polymorphism on repaglinide pharmacokinetics persists over a wide dose range. Br J Clin Pharmacol 66:818–825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kameyama Y, Yamashita K, Kobayashi K, Hosokawa M, Chiba K. (2005) Functional characterization of SLCO1B1 (OATP-C) variants, SLCO1B1*5, SLCO1B1*15 and SLCO1B1*15+C1007G, by using transient expression systems of HeLa and HEK293 cells. Pharmacogenet Genomics 15:513–522 [DOI] [PubMed] [Google Scholar]
- Kamiie J, Ohtsuki S, Iwase R, Ohmine K, Katsukura Y, Yanai K, Sekine Y, Uchida Y, Ito S, Terasaki T. (2008) Quantitative atlas of membrane transporter proteins: development and application of a highly sensitive simultaneous LC/MS/MS method combined with novel in-silico peptide selection criteria. Pharm Res 25:1469–1483 [DOI] [PubMed] [Google Scholar]
- Karlgren M, Vildhede A, Norinder U, Wisniewski JR, Kimoto E, Lai Y, Haglund U, Artursson P. (2012) Classification of inhibitors of hepatic organic anion transporting polypeptides (OATPs): influence of protein expression on drug-drug interactions. J Med Chem 55:4740–4763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimoto E, Yoshida K, Balogh LM, Bi YA, Maeda K, El-Kattan A, Sugiyama Y, Lai Y. (2012) Characterization of organic anion transporting polypeptide (OATP) expression and its functional contribution to the uptake of substrates in human hepatocytes. Mol Pharm 9:3535–3542 [DOI] [PubMed] [Google Scholar]
- Link E, Parish S, Armitage J, Bowman L, Heath S, Matsuda F, Gut I, Lathrop M, Collins R, SEARCH Collaborative Group (2008) SLCO1B1 variants and statin-induced myopathy—a genomewide study. N Engl J Med 359:789–799 [DOI] [PubMed] [Google Scholar]
- Lon HK, Liu D, Jusko WJ. (2012) Pharmacokinetic/pharmacodynamic modeling in inflammation. Crit Rev Biomed Eng 40:295–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsà Carretero M, Alos Manrique C, Valles Callol JA. (2002) Rhabdomyolysis associated with cerivastatin plus gemfibrozil combined regimen. Br J Gen Pract 52:235–236 [PMC free article] [PubMed] [Google Scholar]
- Meier Y, Pauli-Magnus C, Zanger UM, Klein K, Schaeffeler E, Nussler AK, Nussler N, Eichelbaum M, Meier PJ, Stieger B. (2006) Interindividual variability of canalicular ATP-binding-cassette (ABC)-transporter expression in human liver. Hepatology 44:62–74 [DOI] [PubMed] [Google Scholar]
- Mwinyi J, Johne A, Bauer S, Roots I, Gerloff T. (2004) Evidence for inverse effects of OATP-C (SLC21A6) 5 and 1b haplotypes on pravastatin kinetics. Clin Pharmacol Ther 75:415–421 [DOI] [PubMed] [Google Scholar]
- Niemi M, Schaeffeler E, Lang T, Fromm MF, Neuvonen M, Kyrklund C, Backman JT, Kerb R, Schwab M, Neuvonen PJ, et al. (2004) High plasma pravastatin concentrations are associated with single nucleotide polymorphisms and haplotypes of organic anion transporting polypeptide-C (OATP-C, SLCO1B1). Pharmacogenetics 14:429–440 [DOI] [PubMed] [Google Scholar]
- Nies AT, Niemi M, Burk O, Winter S, Zanger UM, Stieger B, Schwab M, Schaeffeler E. (2013) Genetics is a major determinant of expression of the human hepatic uptake transporter OATP1B1, but not of OATP1B3 and OATP2B1. Genome Med 5:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtsuki S, Schaefer O, Kawakami H, Inoue T, Liehner S, Saito A, Ishiguro N, Kishimoto W, Ludwig-Schwellinger E, Ebner T, et al. (2012) Simultaneous absolute protein quantification of transporters, cytochromes P450, and UDP-glucuronosyltransferases as a novel approach for the characterization of individual human liver: comparison with mRNA levels and activities. Drug Metab Dispos 40:83–92 [DOI] [PubMed] [Google Scholar]
- Paine MF, Khalighi M, Fisher JM, Shen DD, Kunze KL, Marsh CL, Perkins JD, Thummel KE. (1997) Characterization of interintestinal and intraintestinal variations in human CYP3A-dependent metabolism. J Pharmacol Exp Ther 283:1552–1562 [PubMed] [Google Scholar]
- Prasad B, Lai Y, Lin Y, Unadkat JD. (2013) Interindividual variability in the hepatic expression of the human breast cancer resistance protein (BCRP/ABCG2): effect of age, sex, and genotype. J Pharm Sci 102:787–793 [DOI] [PubMed] [Google Scholar]
- Rodrigues AC, Perin PM, Purim SG, Silbiger VN, Genvigir FD, Willrich MA, Arazi SS, Luchessi AD, Hirata MH, Bernik MM, et al. (2011) Pharmacogenetics of OATP transporters reveals that SLCO1B1 c.388A>G variant is determinant of increased atorvastatin response. Int J Mol Sci 12:5815–5827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauna ZE, Nandigama K, Ambudkar SV. (2006) Exploiting reaction intermediates of the ATPase reaction to elucidate the mechanism of transport by P-glycoprotein (ABCB1). J Biol Chem 281:26501–26511 [DOI] [PubMed] [Google Scholar]
- Schaefer O, Ohtsuki S, Kawakami H, Inoue T, Liehner S, Saito A, Sakamoto A, Ishiguro N, Matsumaru T, Terasaki T, et al. (2012) Absolute quantification and differential expression of drug transporters, cytochrome P450 enzymes, and UDP-glucuronosyltransferases in cultured primary human hepatocytes. Drug Metab Dispos 40:93–103 [DOI] [PubMed] [Google Scholar]
- Schipani A, Egan D, Dickinson L, Davies G, Boffito M, Youle M, Khoo SH, Back DJ, Owen A. (2012) Estimation of the effect of SLCO1B1 polymorphisms on lopinavir plasma concentration in HIV-infected adults. Antivir Ther 17:861–868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneck DW, Birmingham BK, Zalikowski JA, Mitchell PD, Wang Y, Martin PD, Lasseter KC, Brown CD, Windass AS, Raza A. (2004) The effect of gemfibrozil on the pharmacokinetics of rosuvastatin. Clin Pharmacol Ther 75:455–463 [DOI] [PubMed] [Google Scholar]
- Shitara Y, Hirano M, Sato H, Sugiyama Y. (2004) Gemfibrozil and its glucuronide inhibit the organic anion transporting polypeptide 2 (OATP2/OATP1B1:SLC21A6)-mediated hepatic uptake and CYP2C8-mediated metabolism of cerivastatin: analysis of the mechanism of the clinically relevant drug-drug interaction between cerivastatin and gemfibrozil. J Pharmacol Exp Ther 311:228–236 [DOI] [PubMed] [Google Scholar]
- Shitara Y, Horie T, Sugiyama Y. (2006) Transporters as a determinant of drug clearance and tissue distribution. Eur J Pharm Sci 27:425–446 [DOI] [PubMed] [Google Scholar]
- Sortica VA, Fiegenbaum M, Lima LO, Van der Sand CR, Van der Sand LC, Ferreira ME, Pires RC, Hutz MH. (2012) SLCO1B1 gene variability influences lipid-lowering efficacy on simvastatin therapy in Southern Brazilians. Clin Chem Lab Med 50:441–448 [DOI] [PubMed] [Google Scholar]
- Tirona RG, Leake BF, Merino G, Kim RB. (2001) Polymorphisms in OATP-C: identification of multiple allelic variants associated with altered transport activity among European- and African-Americans. J Biol Chem 276:35669–35675 [DOI] [PubMed] [Google Scholar]
- Tomlinson B, Hu M, Lee VW, Lui SS, Chu TT, Poon EW, Ko GT, Baum L, Tam LS, Li EK. (2010) ABCG2 polymorphism is associated with the low-density lipoprotein cholesterol response to rosuvastatin. Clin Pharmacol Ther 87:558–562 [DOI] [PubMed] [Google Scholar]
- Tucker TG, Milne AM, Fournel-Gigleux S, Fenner KS, Coughtrie MW. (2012) Absolute immunoquantification of the expression of ABC transporters P-glycoprotein, breast cancer resistance protein and multidrug resistance-associated protein 2 in human liver and duodenum. Biochem Pharmacol 83:279–285 [DOI] [PubMed] [Google Scholar]
- Varma MV, Lai Y, Feng B, Litchfield J, Goosen TC, Bergman A. (2012) Physiologically based modeling of pravastatin transporter-mediated hepatobiliary disposition and drug-drug interactions. Pharm Res 29:2860–2873 [DOI] [PubMed] [Google Scholar]
- Varma MV, Lai Y, Kimoto E, Goosen TC, El-Kattan AF, Kumar V. (2013) Mechanistic modeling to predict the transporter- and enzyme-mediated drug-drug interactions of repaglinide. Pharm Res 30:1188–1199 [DOI] [PubMed] [Google Scholar]
- Voora D, Shah SH, Spasojevic I, Ali S, Reed CR, Salisbury BA, Ginsburg GS. (2009) The SLCO1B1*5 genetic variant is associated with statin-induced side effects. J Am Coll Cardiol 54:1609–1616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Li N, Brown PW, Ozer JS, Lai Y. (2011) Liquid chromatography/tandem mass spectrometry based targeted proteomics quantification of P-glycoprotein in various biological samples. Rapid Commun Mass Spectrom 25:1715–1724 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.