Abstract
Retinoic acid (RA) and bile acids share common roles in regulating lipid homeostasis and insulin sensitivity. In addition, the receptor for RA (retinoid x receptor) is a permissive partner of the receptor for bile acids, farnesoid x receptor (FXR/NR1H4). Thus, RA can activate the FXR-mediated pathway as well. The current study was designed to understand the effect of all-trans RA on bile acid homeostasis. Mice were fed an all-trans RA-supplemented diet and the expression of 46 genes that participate in regulating bile acid homeostasis was studied. The data showed that all-trans RA has a profound effect in regulating genes involved in synthesis and transport of bile acids. All-trans RA treatment reduced the gene expression levels of Cyp7a1, Cyp8b1, and Akr1d1, which are involved in bile acid synthesis. All-trans RA also decreased the hepatic mRNA levels of Lrh-1 (Nr5a2) and Hnf4α (Nr2a1), which positively regulate the gene expression of Cyp7a1 and Cyp8b1. Moreover, all-trans RA induced the gene expression levels of negative regulators of bile acid synthesis including hepatic Fgfr4, Fxr, and Shp (Nr0b2) as well as ileal Fgf15. All-trans RA also decreased the expression of Abcb11 and Slc51b, which have a role in bile acid transport. Consistently, all-trans RA reduced hepatic bile acid levels and the ratio of CA/CDCA, as demonstrated by liquid chromatography-mass spectrometry. The data suggest that all-trans RA-induced SHP may contribute to the inhibition of CYP7A1 and CYP8B1, which in turn reduces bile acid synthesis and affects lipid absorption in the gastrointestinal tract.
Keywords: liver, nuclear receptor, FXR, SHP, CYP7A1, CYP8B1
1. Introduction
The role of retinoids in lipid metabolism is an emerging field in retinoid research due to their ability to regulate lipid homeostatic processes including adipogenesis, lipolysis, and fatty acid oxidation. Natural and synthetic retinoids are promising treatments for metabolic syndrome, obesity, and diabetes mellitus [1-5]. It has been shown that all-trans retinoic acid (all-trans RA), the active metabolite of vitamin A, can reduce body fat and improve insulin sensitivity in both lean and obese rodents [6]. Similarly, there is an inverse relationship between vitamin A intake and adiposity in healthy people [7]. Moreover, using genome-wide approaches, we showed that all-trans RA reduces serum lipid in vivo [8].
While there are beneficial effects of retinoids, published data also demonstrated their negative impact in human patients. For example, body weight gain and hyperlipidemia are common side effects when all-trans RA is used to treat acute promyelocytic leukemia [9, 10]. Likewise, hypertriglyceridemia is common in patients who receive retinoid treatment for dermatological disorders [11]. The controversial findings may be explained, in part, by the models used. The conflicting effects of RA treatments may also be due to the fact that retinoid x receptor (RXR), the RA receptor, is a permissive or active partner for the receptors of fatty acids (peroxisome proliferator activated receptors), oxysterols (liver x receptors), and bile acids (farnesoid x receptor) [12]. These receptors regulate lipid homeostasis and often have opposing effects. For example, PPARα (NR1C1), which is highly expressed in the liver, is responsible for lipid oxidation, while PPARγ (NR1C3) is involved in lipogenesis [13]. Thus, RA-mediated activation of one pathway can result in deactivation of another in a tissue-specific manner. Taken together, the role of retinoids in lipid homeostasis is complicated and warrants further investigation.
Bile acids are responsible for lipid absorption in the gastrointestinal tract. They are synthesized in the liver by cholesterol catabolism via the classical (CYP7A1 and CYP8B1) and the acidic pathways (CYP27A1 and CYP7B1) [14]. Upon ingestion of fat and protein, intestinal cholecystokinin stimulates the release of bile containing digestive enzymes and primary bile acids from the gallbladder [15]. In the liver, bile acids activate FXR, which induces the expression of SHP to inhibit the activity of LRH-1 and HNF4α, which are the positive regulators of Cyp7a1 [16, 17]. In the small intestine, bile acid-activated FXR can induce the expression of fibroblast growth factor 15/19 (FGF15/19, rodents/humans), which binds hepatic FGFR4 and activates ERK1/2 (MAPK1/3) and JNK1/2 (MAPK8/9) to inhibit hepatic bile acid synthesis [18-22]. Bile acids are actively reabsorbed from the ileum by IBAT (SLC10A2) and circulate back to the liver through the hepatic portal vein [23]. This highly efficient process ensures that the majority of bile acids are recycled [24]. SLC51A/B (OSTα/β) a heteromeric complex, functions as a major basolateral transporter of bile acids [25], and is essential for intestinal bile acid transportation as well [26]. FXR not only regulates bile acid homeostasis, it also has a role in controlling insulin resistance and glucose homeostasis [27]. Since both RA and bile acids regulate lipid homeostasis and insulin sensitivity, the current study examines the pharmacological effect of all-trans RA on bile acid homeostasis.
Using non-biased approaches, we have conducted microarray study, bile acid quantification, and proteomic study to analyze the action of all-trans RA in bile acid homeostasis. Our data show that all-trans RA has a significant effect in regulating bile acid homeostasis in vivo. All-trans RA inhibits bile acid synthesis by down regulating the expression of key bile acid synthesis enzymes, CYP7A1 and CYP8B1. All-trans RA also modulates the expression of genes that have a role in the transportation of bile acids. All-trans RA treatment reduced the CA/CDCA ratio and may have an impact on lipid absorption.
2. Materials and Methods
2.1 In vivo and in vitro Experiments
Wild type C57/BL mice were purchased from the Jackson Laboratory (Sacramento, CA, USA) and Slac Laboratory Animal (Shanghai, China). Mice were treated with standard rodent chow or supplemented with all-trans RA (Sigma, St. Louis, MO) (150 mg/kg diet) for seven days. The concentration was chosen due to its anti-carcinogenic effect in a rat model of liver carcinogenesis in the absence of severe toxicity [28]. At the end of the treatment, mice were anesthetized with isoflurane and euthanized. Livers and ileums were frozen in liquid nitrogen immediately after collection and stored in -80°C freezer for further assays. The animal treatment experiment was repeated twice using sample size of 5 per control and all-trans RA-treated group. Animal protocols and procedures were approved by the Institutional Animal Care and Use Committee (IACUC) at the University of Kansas Medical Center and the University of California, Davis as well as the Experimental Animal Ethics Committee at the Shanghai University of Traditional Chinese Medicine.
Primary human hepatocytes, derived from two donors, were provided by XenoTech (Lenexa, KS). Cells were treated with DMSO and all-trans RA (10 uM) for 12 hours in triplicates followed by RNA extraction to study gene expression.
2.2 Quantification of bile acids
An ultra-performance liquid chromatography instrument coupled with a quatropole mass spectrometry (UPLC-MS, Waters Co., MA, USA) was used to detect hepatic bile acids. Livers were homogenized in acetonitrile (100 mg tissue/500 μl acetonitrile) followed by centrifugation at 14,300 rpm for 10 min. The supernatant was dried under nitrogen steam, then re-dissolved in methanol solution (methanol : water : formic acid = 50 : 50 : 0.01) followed by centrifugation at 14,300 rpm for 10 min. The supernatants were injected into the UPLC-MS instrument. Both the UPLC and MS parameters were described in our previous publication [29]. Bile acids profiles in control and RA-treated mice were differentiated by principle component analysis (PCA). Significance of differences between individual bile acid levels in control and all-trans RA-treated mice were examined by Student's t-test.
2.3 Global expression profile of genes that contribute to bile acid homeostasis in control and all-trans RA-treated mice
The hepatic gene expressions in control and all-trans RA-treated mice (n = 3) were studied by microarray as described in our previous publication [30]. Microarray data are available in the public database (NIH GEO, GSE50028). Bile acid-related genes (n = 46) were selected from the KEGG (Kyoto Encyclopedia of Genes and Genomes) pathway database. Expression levels of these 46 genes were extracted from the microarray data. PCA was used to describe the expression profile of these genes in control and all-trans RA-treated groups. Student's t-test was used to differentiate expression profiles between groups based on PCA scores.
2.4 Proteomics
Proteins were extracted from mouse livers by T-PER (Thermo Scientific, Rockford, IL, USA). Protein concentrations were determined by protein assay kit (Thermo Scientific, Rockford, IL, USA). Proteins (200 μg) were precipitated and washed with Protein Precipitation Kit (Calbiochem, La Jolla, CA, USA). The protein pellets were reconstituted in urea solution (6 M in 25 mM ammonium bicarbonate) and then mixed with reducing reagent containing 30 mg/mL DTT in 25 mM ammonium bicarbonate. After 1 hour incubation at room temperature, 20 μl iodoacetamide (200 mM in 25 mM ammonium bicarbonate) was added for alkylation, which was quenched by dilution with 10 times the volume of ammonium bicarbonate (25 mM). The diluted samples were mixed with 10 μl trypsin (0.7 mg/ml in 25 mM ammonium bicarbonate), then incubated overnight at 37°C for digestion. The digested samples were cleaned with Aspire RP30 tips (Thermo Scientific, Rockford, IL, USA) followed by injection into the nano liquid chromatography (nLC) coupled with MS instrument (Q-Exactive, Thermo Fisher, San Jose, CA, USA). The nLC-MS parameters as well as the data processing and annotation were performed based on previously published methods [31]. PCA was used to describe the global expression profile of the mouse hepatic proteome in control and all-trans RA-treated groups. A volcano plot was generated to visualize both fold change and significance of the protein expression levels between control and all-trans RA -treated mice.
2.5 Quantification of mRNA
Total RNA was extracted using TRIzol reagent (Life Technologies, Carlsbad, CA, USA) followed by reverse transcription using the High Capacity cDNA Reverse Transcription Kits (Applied Biosystems, Foster City, CA, USA). The mRNA levels were quantified by real-time PCR on an ABI 7900HT Fast Real time PCR system (Applied Biosystems, CA, USA) using Power SYBR Green PCR Master Mix (Applied Biosystems, CA, USA). Hepatic and ileal mRNA levels were normalized to the mRNA level of glyceraldehyde-3-phosphate dehydrogenase (Gapdh). Gapdh is considered a house keeping gene and frequently used as a reference gene [32, 33]. In addition, it has been shown that Gapdh is one of the most stable reference genes [34]. Primers were designed using the Primer3 Input Program and the primer sequences are listed in supplemental Table S1 [35, 36].
2.6 Western Blot
Hepatic proteins were extracted using a T-PER kit (Thermo Scientific, Rockford, IL, USA) followed by quantification using a protein assay kit (Thermo Scientific, Rockford, IL, USA). Proteins (50 μg) were electrophoresed on a 12% SDS-PAGE and transferred to a polyvinylidene fluoride (PVDF) membrane (Bio-Rad, CA). Nonspecific bindings were blocked by 5% non-fat milk in TBST (10 mM Tris pH 7.5, 100 mM NaCl, 0.1% Tween 20). Antibodies specific for CYP7A1 (Millipore, Billerica, CA, USA), CYP8B1 (Santa Cruz Inc., Santa Cruz, CA, USA), SHP (Santa Cruz Inc., Santa Cruz, CA, USA), and GAPDH (Santa Cruz Inc., Santa Cruz, CA, USA) were used. Anti-mouse IgG (Thermo Scientific, Rockford, IL, USA) was used for detection of CYP7A1, CYP8B1, and SHP, while anti-rabbit IgG (Santa Cruz Inc. Santa Cruz, USA) was used for detection of GAPDH. Signals were imaged with Chemiluminescent Substrate Kit (Thermo Scientific, Rockford, IL, USA). NIH image program (ImageJ 1.47, http://rsb.info.nih.gov/ij/) was used to scan the band densities on western blot images. Scanned densities of target proteins were normalized to GAPDH bands, and then used for Student's t-test.
2.7 Data analysis
Student's t-test was performed following corresponding F test in Microsoft Excel 2010. PCA algorithm was performed in SPSS (version 20.0, IBM Co., CA, USA). A Volcano plot was generated by plot minus log2 p value (y-axis) against log2 fold change (x-axis) between two investigated groups. All graphs were generated with the SPSS software.
3. Results
3.1 All-trans RA regulates the expression of genes that control bile acid homeostasis
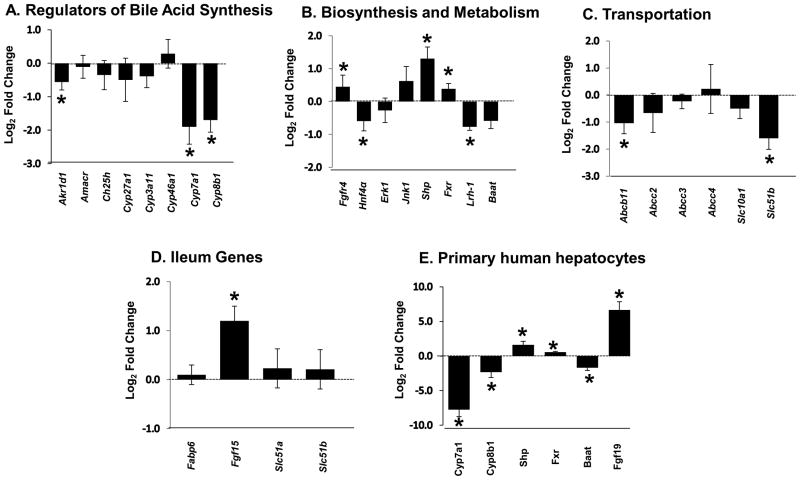
Forty-six genes involved in bile acid biosynthesis, conjugation, transportation, and regulation were identified based on the KEGG pathways. Hepatic mRNA levels of these genes in control and all-trans RA-treated groups were quantified using microarray (n =3). PCA was used to profile the change in their mRNA levels. The score plot shows that control and all-trans RA-treated mice belonged to two distinct groups (Fig. 1). Student's t-test with p value ≤ 0.05 indicated that all-trans RA treatment differentiated the two groups. Figure 2 illustrates the expression levels of genes measured by real-time PCR. All-trans RA treatment reduced the expression level of Cyp7a1, Cyp8b1, and Akr1d1, which are involved in bile acid biosynthesis or metabolism. All-trans RA also decreased the hepatic mRNA levels of Lrh-1 and Hnf4a, which can positively regulate the expression of Cyp7a1. Conversely, all-trans RA induced the expression levels of negative regulators of bile acid synthesis including Fgfr4, Shp, and Fxr All-trans RA also reduced the expression level of Abcb11 responsible for transporting bile acids from the liver to the small intestine. SLC51A/SLC51B heteromers transport bile acid as well, but only hepatic Slc51b mRNA level was reduced in all-trans RA-treated mice. In addition to regulating hepatic bile acid genes, all-trans RA increased the expression level of ileal Fgf15, another negative regulator of hepatic Cyp7a1 (Fig. 2E). Given these results, all-trans RA could regulate bile acid metabolism in mouse liver.
Figure 1. The effect of all-trans RA in regulating the expression of genes that control bile acid homeostasis.
Wild type mice were fed either an all-trans RA-supplemented (150 mg/kg body weight) or standard chow diet for 7 days. The expression levels of forty-six hepatic genes regulating bile acid homeostasis were studied by microarray (n = 3 per group). Score plot of principal component analysis (PCA) shows differential gene expression patterns for control and all-trans RA-treated mice in bile acid homeostasis.
Figure 2. The effect of all-trans RA in regulating the expression of genes involved in bile acid homeostasis.
(A-D) Real-time PCR was used to quantify the expression level of selected genes involved in bile acid homeostasis in control and all-trans RA-treated mice (n = 5). The experiment was repeated twice using different livers and the data were consistent in both experiments. (E) The effect of all-trans RA in regulating bile acid homeostasis genes was studied in primary human hepatocytes. Data were normalized to the control values and are expressed as mean +/- SD *, p ≤ 0.05.
The effect of all-trans RA in regulating bile acid homeostasis genes was also studied using primary human hepatocytes. All-trans RA treatment induced the expression of Fgf19, Shp and Fxr, but reduced the expression levels of Baat, Cyp7a1, and Cyp8b1. These findings were consistent with the data obtained from the in vivo mouse experiments.
3.2 All-trans RA decreased hepatic bile acid levels
Twelve bile acids were analyzed by UPLC-MS in control and all-trans RA-treated mouse livers (n = 5). PCA score plot shows that control and all-trans RA-treated mice each belong to a distinct group (p ≤ 0.05) (Fig. 3A), indicating a role for all-trans RA in changing the bile acids profiles in the livers. Individual bile acid levels are shown in Figure 3B. All-trans RA significantly reduced most bile acid levels except for CDCA, TCDCA, and THDCA. Because all-trans RA reduced hepatic CA level by 2-fold, the ratio of CA to CDCA was reduced in all-trans RA-treated mouse livers.
Figure 3. The effect of all-trans RA on bile acids in mouse livers.
Twelve hepatic bile acids were quantified by UPLC-MS in control and all-trans RA-treated mouse livers (n = 5). (A) Score plot of PCA showing all-trans RA-mediated changes on bile acid profiles. (B) Individual bile acid levels were reduced by all-trans RA treatment. The CA/CDCA ratio also decreased significantly after all-trans RA treatment. *: p ≤ 0.05 vs. control.
3.3 All-trans RA affects the level of proteins that are involved in bile acid homeostasis
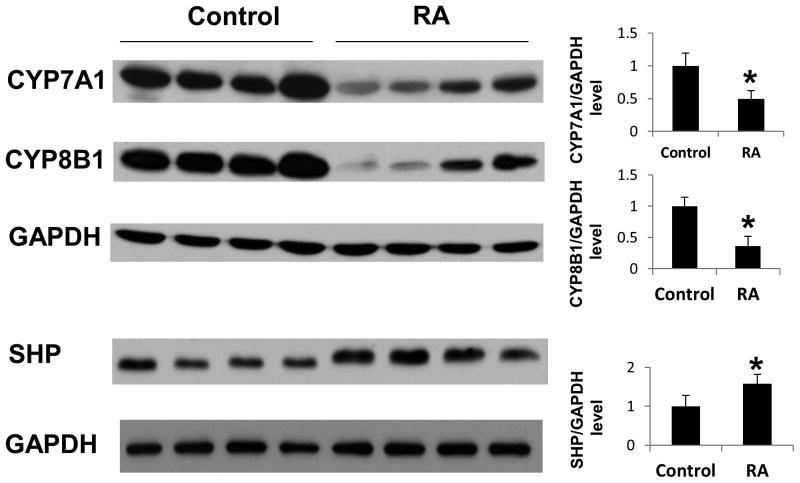
The effect of all-trans RA on the proteome was studied by nLC-MS (n=3 per group). The analysis was done in triplicates per mouse liver. Thus, nine data points per group were included for PCA analysis. The score plot shows that control and all-trans RA-treated mice each belongs to a separate group (p ≤ 0.05) (Fig. 4A). Thus, all-trans RA changed the expression profile of the mouse hepatic proteome. Further analysis was conducted to differentiate the protein levels by Student's t-test. The volcano plot shows that most detected proteins are located on the negative side of the x-axis, indicating that all-trans RA reduced the global protein expression (Fig. 4B). Thirteen bile acid-related proteins were detectable by nLC-MS. With the exception of ACOX2, AMACR, and SLCO1B2, all other detected proteins related to bile acids showed significant down regulation. Consistent with our hepatic mRNA expression data, the protein levels of CYP8B1 and AKR1D1 were reduced in all-trans RA -treated mice. In addition, the protein level of ABCB11, a bile acid transporter [23], and SLC27A5, a very long-chain acyl-CoA synthetase [37], was also reduced by all-trans RA treatment (Fig. 4). The protein levels of CYP7A1, CYP8B1, and SHP were also analyzed by Western blot. All-trans RA reduced the protein levels of CYP7A1 and CYP8B1, but increased SHP protein level (Fig. 5), which was consistent with gene expression data shown in figure 2.
Figure 4. All-trans RA affected the expression levels of global proteins as well as proteins associated with bile acids homeostasis in mouse livers.
The effect of all-trans RA on the proteome was studied by nLC-MS (n = 3 mice per group). (A) PCA score plot differentiates the global expression levels of all detected hepatic proteins in control and all-trans RA-treated mice. (B) Volcano plot shows significant protein changes regulated by all-trans RA treatment. The horizontal dash line divides significant (above the line) from non-significant (below the line) protein level changes. The vertical dash line separates up regulated proteins (right) from down regulated proteins (left).
Figure 5. The effect of all-trans RA on hepatic protein levels.
Hepatic protein levels of CYP7A1, CYP8B1, and SHP were examined in control and all-trans RA-treated mice (n = 4) by Western blot using specific antibodies. The experiment was repeated twice using different livers and the data were consistent in both experiments. Hepatic GAPDH level was used as loading control. CYP7A1 and CYP8B1 levels were reduced, but SHP level was increased by all-trans RA treatment.
4. Discussion
The current paper studied the effect of all-trans RA on the expression of genes and encoded proteins that control bile acid homeostasis as well as hepatic bile acid profiles in mice. The data demonstrated a significant role of all-trans RA in regulating bile acid synthesis in the mouse liver. All-trans RA inhibited the gene expression of Cyp7a1, Cyp8b1, and Akr1d1, all of which control bile acid synthesis. In addition, all-trans RA also reduced the expression levels of Hnf4α and Lrh-1, which are key positive regulators for Cyp7a1 and Cyp8b1 expression. Conversely, all-trans RA increased the gene expression levels of Fgfr4, Shp, and Fxr, which negatively regulate Cyp7a1 and Cyp8b1 expression [16, 21, 22]. Synthetic compounds that are specific for RXR, such as LG268, have been used to study the effect of RXR in lipid homeostasis [38, 39]. Hepatic genome-wide binding of RXR and RAR have also been performed. The data demonstrated the extensive role of retinoids and RXR in regulating in lipid homeostasis [8, 39, 40]. LG268 also reduces bile acid pool size [38]. The current study used all-trans RA, which is the most abundant biological active form of RA in our body and is frequently used clinically to treat skin conditions and cancer. All-trans RA preferentially activates RAR [41]. However, high concentrations of all-trans RA can convert into 9-cis RA and activate RXR [42]. An FXR/RXR-independent mechanism for all-trans RA to repress Cyp7a1 has been reported previously in cell culture [43]. Our published data also showed that RARα binds to Cyp8b1, Abcc3, and Shp [30]. Thus, the observed regulatory effect could be mediated via RAR. It is important to note that in the current study, the mice were fed an all-trans RA-supplemented diet for 7 days, thus the observed regulatory effects could be mediated via RXR and its dimeric partners or even their downstream effects.
RA-induced down regulation of Cyp7a1 has been shown in vitro using human HepG2 and primary human hepatocytes [43]. This finding has been confirmed in this in vivo study. The current study also provides novel information that all-trans RA can inhibit multiple genes involved in bile acid synthesis in vivo. In addition to bile acid biosynthesis, all-trans RA also regulated genes that transport bile acids. All-trans RA decreased the gene expression levels of Abcb11 and Slc51b, which have a role in exporting bile acids from the liver [44]. It is likely that the transporters acted as bile acid sensors, which would have decreased along with the reduction of the bile acid pool. Taken together, all-trans RA reduced the hepatic bile acid levels by repressing bile acid biosynthesis.
The signaling pathway in the gut-liver axis regulates bile acid homeostasis. In the liver, the FXR-induced SHP interacts with LRH-1/HNF4α and inhibits Cyp7a1 as well as Cyp8b1 to limit the synthesis of bile acids [16, 45-47]. In the ileum, FXR-induced FGF15, via enterohepatic circulation, interacts with hepatic FGFR4 and activates ERK1/2 and JNK1/2. Activated ERK1/2 and JNK1/2 in turn represses Cyp7a1 and Cyp8b1 [18-22]. All-trans RA significantly increased ileal Fgf15 expression. Although Fgf19 was reported to be induced by all-trans RA in HepG2 cells and human hepatocytes [43], this is the first report showing the impact of all-trans RA on intestinal Fgf15 gene expression levels in vivo. Consistent with our findings, oral administration of vitamin A also induced intestinal Fgf15 and inhibited Cyp7a1 [48].
Our novel finding showed that in addition to CYP7A1, all-trans RA also reduced the gene and protein expression of CYP8B1, which is crucial for CA synthesis [49]. Without CYP8B1, CYP7A1 can only produce CDCA. Thus, alteration of CYP8B1 expression changes the CA/CDCA ratio [50]. It is also known that insulin can inhibit CYP8B1 [51]. In non-obese diabetic mice, CA/CDCA ratio is increased [52]. This increase in the CA/CDCA ratio enhances cholesterol absorption, leading to significant hypercholesterolemia, which in turn leads to the development of atheromatous lesions [53]. Specifically, CA promotes cholesterol absorption, while CDCA does not [54]. Therefore, a reduced CA/CDCA ratio may potentially lead to lower cholesterol absorption. Our novel data showed that all-trans RA reduces CA/CDCA ratio, which may in part explain the effect of all-trans RA in regulating cholesterol and triglyceride levels in vivo [30].
Taken together, all-trans RA has a profound effect in regulating genes and proteins involved in bile acid homeostasis in vivo. All-trans RA -regulated SHP pathway may play a role in inhibition of bile acid synthesis. As bile acids are important lipid regulators participating in lipid absorption and lipid metabolism, all-trans RA-mediated bile acids regulation could be used to explain the effect of RA in lipid homeostasis.
Acknowledgments
This work was supported by National Institutes of Health [DK092100 to Y-J.W., CA53596 to Y-J.W.]. Authors thank Dr. Yingying Huang of Thermo Fisher Scientific for helping proteomics assay, Dr. Sidhartha Hazari of UC Davis Medical Center for participating in proteomics sample preparation, and Lisa Teixeira for editing the manuscript.
Footnotes
Chemical compounds: All-trans retinoic acid (Pubchem CID: 444795)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Fan Yang, Email: fanyangforever@gmail.com.
Yuqi He, Email: hyqjeff@gmail.com.
Hui-Xin Liu, Email: huixinliu2012@gmail.com.
Jessica Tsuei, Email: Jltsuei10@gmail.com.
Xiaoyue Jiang, Email: xiaoyue.jiang@thermofisher.com.
Li Yang, Email: yangli7951@hotmail.com.
Zheng-Tao Wang, Email: wangzht@hotmail.com.
Yu-Jui Yvonne Wan, Email: yjywan@ucdavis.edu.
References
- 1.Pinaire JA, Reifel-Miller A. Therapeutic potential of retinoid x receptor modulators for the treatment of the metabolic syndrome. PPAR research. 2007;2007:94156. doi: 10.1155/2007/94156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shulman AI, Mangelsdorf DJ. Retinoid x receptor heterodimers in the metabolic syndrome. The New England journal of medicine. 2005;353:604–15. doi: 10.1056/NEJMra043590. [DOI] [PubMed] [Google Scholar]
- 3.Mukherjee R, Davies PJ, Crombie DL, Bischoff ED, Cesario RM, Jow L, et al. Sensitization of diabetic and obese mice to insulin by retinoid X receptor agonists. Nature. 1997;386:407–10. doi: 10.1038/386407a0. [DOI] [PubMed] [Google Scholar]
- 4.Wolf G. Retinoic acid activation of peroxisome proliferation-activated receptor delta represses obesity and insulin resistance. Nutrition reviews. 2010;68:67–70. doi: 10.1111/j.1753-4887.2009.00261.x. [DOI] [PubMed] [Google Scholar]
- 5.Han SY, So GA, Jee YH, Han KH, Kang YS, Kim HK, et al. Effect of retinoic acid in experimental diabetic nephropathy. Immunology and cell biology. 2004;82:568–76. doi: 10.1111/j.1440-1711.2004.01287.x. [DOI] [PubMed] [Google Scholar]
- 6.Berry DC, Noy N. All-trans-retinoic acid represses obesity and insulin resistance by activating both peroxisome proliferation-activated receptor beta/delta and retinoic acid receptor. Molecular and cellular biology. 2009;29:3286–96. doi: 10.1128/MCB.01742-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zulet MA, Puchau B, Hermsdorff HH, Navarro C, Martinez JA. Vitamin A intake is inversely related with adiposity in healthy young adults. Journal of nutritional science and vitaminology. 2008;54:347–52. doi: 10.3177/jnsv.54.347. [DOI] [PubMed] [Google Scholar]
- 8.He Y, Gong L, Fang Y, Zhan Q, Liu HX, Lu Y, et al. The role of retinoic acid in hepatic lipid homeostasis defined by genomic binding and transcriptome profiling. BMC genomics. 2013;14:575. doi: 10.1186/1471-2164-14-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fenaux P, De Botton S. Retinoic acid syndrome. Recognition, prevention and management. Drug safety : an international journal of medical toxicology and drug experience. 1998;18:273–9. doi: 10.2165/00002018-199818040-00003. [DOI] [PubMed] [Google Scholar]
- 10.Tallman MS, Andersen JW, Schiffer CA, Appelbaum FR, Feusner JH, Ogden A, et al. All-trans-retinoic acid in acute promyelocytic leukemia. The New England journal of medicine. 1997;337:1021–8. doi: 10.1056/NEJM199710093371501. [DOI] [PubMed] [Google Scholar]
- 11.Bershad S, Rubinstein A, Paterniti JR, Le NA, Poliak SC, Heller B, et al. Changes in plasma lipids and lipoproteins during isotretinoin therapy for acne. The New England journal of medicine. 1985;313:981–5. doi: 10.1056/NEJM198510173131604. [DOI] [PubMed] [Google Scholar]
- 12.Bonet ML, Ribot J, Palou A. Lipid metabolism in mammalian tissues and its control by retinoic acid. Biochimica et biophysica acta. 2012;1821:177–89. doi: 10.1016/j.bbalip.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 13.Chawla A, Repa JJ, Evans RM, Mangelsdorf DJ. Nuclear receptors and lipid physiology: opening the X-files. Science (New York, NY) 2001;294:1866–70. doi: 10.1126/science.294.5548.1866. [DOI] [PubMed] [Google Scholar]
- 14.Chiang JY. Bile acids: regulation of synthesis. Journal of lipid research. 2009;50:1955–66. doi: 10.1194/jlr.R900010-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dockray GJ. Cholecystokinin. Current opinion in endocrinology, diabetes, and obesity. 2012;19:8–12. doi: 10.1097/MED.0b013e32834eb77d. [DOI] [PubMed] [Google Scholar]
- 16.Goodwin B, Jones SA, Price RR, Watson MA, McKee DD, Moore LB, et al. A regulatory cascade of the nuclear receptors FXR, SHP-1, and LRH-1 represses bile acid biosynthesis. Molecular cell. 2000;6:517–26. doi: 10.1016/s1097-2765(00)00051-4. [DOI] [PubMed] [Google Scholar]
- 17.Wei J, Qiu de K, Ma X. Bile acids and insulin resistance: implications for treating nonalcoholic fatty liver disease. Journal of digestive diseases. 2009;10:85–90. doi: 10.1111/j.1751-2980.2009.00369.x. [DOI] [PubMed] [Google Scholar]
- 18.Stroeve JH, Brufau G, Stellaard F, Gonzalez FJ, Staels B, Kuipers F. Intestinal FXR-mediated FGF15 production contributes to diurnal control of hepatic bile acid synthesis in mice. Laboratory investigation; a journal of technical methods and pathology. 2010;90:1457–67. doi: 10.1038/labinvest.2010.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inagaki T, Choi M, Moschetta A, Peng L, Cummins CL, McDonald JG, et al. Fibroblast growth factor 15 functions as an enterohepatic signal to regulate bile acid homeostasis. Cell Metab. 2005;2:217–25. doi: 10.1016/j.cmet.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 20.Shin DJ, Osborne TF. FGF15/FGFR4 integrates growth factor signaling with hepatic bile acid metabolism and insulin action. The Journal of biological chemistry. 2009;284:11110–20. doi: 10.1074/jbc.M808747200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu C, Wang F, Jin C, Huang X, McKeehan WL. Independent repression of bile acid synthesis and activation of c-Jun N-terminal kinase (JNK) by activated hepatocyte fibroblast growth factor receptor 4 (FGFR4) and bile acids. The Journal of biological chemistry. 2005;280:17707–14. doi: 10.1074/jbc.M411771200. [DOI] [PubMed] [Google Scholar]
- 22.Song KH, Li T, Owsley E, Strom S, Chiang JY. Bile acids activate fibroblast growth factor 19 signaling in human hepatocytes to inhibit cholesterol 7alpha-hydroxylase gene expression. Hepatology (Baltimore, Md) 2009;49:297–305. doi: 10.1002/hep.22627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meier PJ, Stieger B. Bile salt transporters. Annual review of physiology. 2002;64:635–61. doi: 10.1146/annurev.physiol.64.082201.100300. [DOI] [PubMed] [Google Scholar]
- 24.Galatola G, Jazrawi RP, Bridges C, Joseph AE, Northfield TC. Direct measurement of first-pass ileal clearance of a bile acid in humans. Gastroenterology. 1991;100:1100–5. doi: 10.1016/0016-5085(91)90288-v. [DOI] [PubMed] [Google Scholar]
- 25.Ballatori N, Fang F, Christian WV, Li N, Hammond CL. Ostalpha-Ostbeta is required for bile acid and conjugated steroid disposition in the intestine, kidney, and liver. American journal of physiology Gastrointestinal and liver physiology. 2008;295:G179–G86. doi: 10.1152/ajpgi.90319.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rao A, Haywood J, Craddock AL, Belinsky MG, Kruh GD, Dawson PA. The organic solute transporter alpha-beta, Ostalpha-Ostbeta, is essential for intestinal bile acid transport and homeostasis. Proceedings of the National Academy of Sciences of the United States of America. 2008;105:3891–6. doi: 10.1073/pnas.0712328105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trauner M, Claudel T, Fickert P, Moustafa T, Wagner M. Bile acids as regulators of hepatic lipid and glucose metabolism. Digestive diseases (Basel, Switzerland) 2010;28:220–4. doi: 10.1159/000282091. [DOI] [PubMed] [Google Scholar]
- 28.Tamura K, Nakae D, Horiguchi K, Akai H, Kobayashi Y, Andoh N, et al. Inhibition by N-(4-hydroxyphenyl)retinamide and all-trans-retinoic acid of exogenous and endogenous development of putative preneoplastic, glutathione S-transferase placental form-positive lesions in the livers of rats. Carcinogenesis. 1997;18:2133–41. doi: 10.1093/carcin/18.11.2133. [DOI] [PubMed] [Google Scholar]
- 29.Yang F, Xu Y, Xiong A, He Y, Yang L, Wan YJY, et al. Evaluation of the protective effect of Rhei Radix et Rhizoma against α-naphthylisothiocyanate induced liver injury based on metabolic profile of bile acids. Journal of ethnopharmacology. 2012;144:599–604. doi: 10.1016/j.jep.2012.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He Y, Gong L, Fang Y, Zhan Q, Liu HX, Lu Y, et al. The role of retinoic acid in hepatic lipid homeostasis defined by genomic binding and transcriptome profiling. BMC genomics. 2013;14:575. doi: 10.1186/1471-2164-14-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Michalski A, Damoc E, Hauschild JP, Lange O, Wieghaus A, Makarov A, et al. Mass spectrometry-based proteomics using Q Exactive, a high-performance benchtop quadrupole Orbitrap mass spectrometer. Molecular & cellular proteomics : MCP. 2011;10:M111 011015. doi: 10.1074/mcp.M111.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yoshimoto S, Loo TM, Atarashi K, Kanda H, Sato S, Oyadomari S, et al. Obesity-induced gut microbial metabolite promotes liver cancer through senescence secretome. Nature. 2013;499:97–101. doi: 10.1038/nature12347. [DOI] [PubMed] [Google Scholar]
- 33.Neumann K, Kruse N, Szilagyi B, Erben U, Rudolph C, Flach A, et al. Connecting liver and gut: murine liver sinusoidal endothelium induces gut tropism of CD4+ T cells via retinoic acid. Hepatology (Baltimore, Md) 2012;55:1976–84. doi: 10.1002/hep.24816. [DOI] [PubMed] [Google Scholar]
- 34.Xu L, Ma X, Cui B, Li X, Ning G, Wang S. Selection of reference genes for qRT-PCR in high fat diet-induced hepatic steatosis mice model. Molecular biotechnology. 2011;48:255–62. doi: 10.1007/s12033-010-9366-2. [DOI] [PubMed] [Google Scholar]
- 35.Untergasser A, Cutcutache I, Koressaar T, Ye J, Faircloth BC, Remm M, et al. Primer3-new capabilities and interfaces. Nucleic acids research. 2012;40:e115. doi: 10.1093/nar/gks596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koressaar T, Remm M. Enhancements and modifications of primer design program Primer3. Bioinformatics (Oxford, England) 2007;23:1289–91. doi: 10.1093/bioinformatics/btm091. [DOI] [PubMed] [Google Scholar]
- 37.Anderson CM, Stahl A. SLC27 fatty acid transport proteins. Molecular aspects of medicine. 2013;34:516–28. doi: 10.1016/j.mam.2012.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Repa JJ, Turley SD, Lobaccaro JA, Medina J, Li L, Lustig K, et al. Regulation of absorption and ABC1-mediated efflux of cholesterol by RXR heterodimers. Science (New York, NY) 2000;289:1524–9. doi: 10.1126/science.289.5484.1524. [DOI] [PubMed] [Google Scholar]
- 39.Kosters A, Sun D, Wu H, Tian F, Felix JC, Li W, et al. Sexually dimorphic genome-wide binding of retinoid X receptor alpha (RXRalpha) determines male-female differences in the expression of hepatic lipid processing genes in mice. PloS one. 2013;8:e71538. doi: 10.1371/journal.pone.0071538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhan Q, Fang Y, He Y, Liu HX, Fang J, Wan YJ. Function annotation of hepatic retinoid x receptor alpha based on genome-wide DNA binding and transcriptome profiling. PloS one. 2012;7:e50013. doi: 10.1371/journal.pone.0050013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allenby G, Bocquel MT, Saunders M, Kazmer S, Speck J, Rosenberger M, et al. Retinoic acid receptors and retinoid X receptors: interactions with endogenous retinoic acids. Proceedings of the National Academy of Sciences of the United States of America. 1993;90:30–4. doi: 10.1073/pnas.90.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heyman RA, Mangelsdorf DJ, Dyck JA, Stein RB, Eichele G, Evans RM, et al. 9-cis retinoic acid is a high affinity ligand for the retinoid X receptor. Cell. 1992;68:397–406. doi: 10.1016/0092-8674(92)90479-v. [DOI] [PubMed] [Google Scholar]
- 43.Cai SY, He H, Nguyen T, Mennone A, Boyer JL. Retinoic acid represses CYP7A1 expression in human hepatocytes and HepG2 cells by FXR/RXR-dependent and independent mechanisms. Journal of lipid research. 2010;51:2265–74. doi: 10.1194/jlr.M005546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dawson PA, Lan T, Rao A. Bile acid transporters. Journal of lipid research. 2009;50:2340–57. doi: 10.1194/jlr.R900012-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang M, Chiang JY. Transcriptional regulation of the human sterol 12alpha-hydroxylase gene (CYP8B1): roles of heaptocyte nuclear factor 4alpha in mediating bile acid repression. The Journal of biological chemistry. 2001;276:41690–9. doi: 10.1074/jbc.M105117200. [DOI] [PubMed] [Google Scholar]
- 46.Ortlund EA, Lee Y, Solomon IH, Hager JM, Safi R, Choi Y, et al. Modulation of human nuclear receptor LRH-1 activity by phospholipids and SHP. Nature structural & molecular biology. 2005;12:357–63. doi: 10.1038/nsmb910. [DOI] [PubMed] [Google Scholar]
- 47.del Castillo-Olivares A, Campos JA, Pandak WM, Gil G. The role of alpha1-fetoprotein transcription factor/LRH-1 in bile acid biosynthesis: a known nuclear receptor activator that can act as a suppressor of bile acid biosynthesis. The Journal of biological chemistry. 2004;279:16813–21. doi: 10.1074/jbc.M400646200. [DOI] [PubMed] [Google Scholar]
- 48.Schmidt DR, Holmstrom SR, Fon Tacer K, Bookout AL, Kliewer SA, Mangelsdorf DJ. Regulation of bile acid synthesis by fat-soluble vitamins A and D. The Journal of biological chemistry. 2010;285:14486–94. doi: 10.1074/jbc.M110.116004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vlahcevic ZR, Eggertsen G, Bjorkhem I, Hylemon PB, Redford K, Pandak WM. Regulation of sterol 12alpha-hydroxylase and cholic acid biosynthesis in the rat. Gastroenterology. 2000;118:599–607. doi: 10.1016/s0016-5085(00)70267-8. [DOI] [PubMed] [Google Scholar]
- 50.Pandak WM, Bohdan P, Franklund C, Mallonee DH, Eggertsen G, Bjorkhem I, et al. Expression of sterol 12alpha-hydroxylase alters bile acid pool composition in primary rat hepatocytes and in vivo. Gastroenterology. 2001;120:1801–9. doi: 10.1053/gast.2001.24833. [DOI] [PubMed] [Google Scholar]
- 51.Ishida H, Yamashita C, Kuruta Y, Yoshida Y, Noshiro M. Insulin is a dominant suppressor of sterol 12 alpha-hydroxylase P450 (CYP8B) expression in rat liver: possible role of insulin in circadian rhythm of CYP8B. Journal of biochemistry. 2000;127:57–64. doi: 10.1093/oxfordjournals.jbchem.a022584. [DOI] [PubMed] [Google Scholar]
- 52.Uchida K, Makino S, Akiyoshi T. Altered bile acid metabolism in nonobese, spontaneously diabetic (NOD) mice. Diabetes. 1985;34:79–83. doi: 10.2337/diab.34.1.79. [DOI] [PubMed] [Google Scholar]
- 53.Uchida K, Satoh T, Takase H, Nomura Y, Takasu N, Kurihara H, et al. Altered bile acid metabolism related to atherosclerosis in alloxan diabetic rats. Journal of atherosclerosis and thrombosis. 1996;3:52–8. doi: 10.5551/jat1994.3.52. [DOI] [PubMed] [Google Scholar]
- 54.Reynier MO, Montet JC, Gerolami A, Marteau C, Crotte C, Montet AM, et al. Comparative effects of cholic, chenodeoxycholic, and ursodeoxycholic acids on micellar solubilization and intestinal absorption of cholesterol. Journal of lipid research. 1981;22:467–73. [PubMed] [Google Scholar]