Highlights
-
•
Increased extrusion of the medial meniscus with loaded MRI compared to unloaded.
-
•
No change in lateral meniscus extrusion between loaded and unloaded MRI.
-
•
Increased extrusion of the medial meniscus with loaded MRI in those with tears.
Keywords: Stress MRI, Weighted MRI, Axial load, Meniscus extrusion, Osteoarthritis
Abstract
Objective
Assess the impact of knee joint loading on meniscal extrusion in normal individuals and those with varying degrees of osteoarthritis (OA).
Methods
143 healthy volunteers and patients with OA underwent 3 T MRI of the knee under unloaded and loaded conditions. OA was graded with the Kellgren-Lawrence (KL) system. Menisci were evaluated for presence of tear. Descriptive statistics were expressed as mean ± standard deviation. Loaded and unloaded groups were compared using Student’s t-test. Statistic significance was defined for all calculations as p < 0.05.
Results
The cohort included 87 women and 56 men with an average age of 53 years +/− 9.7 years. Kellgren-Lawrence grade distribution was as follows: 56 with grade 0, 46 with grade 1, 25 with grade 2, 13 with grade 3, and 3 with grade 4. 23% had medial meniscus tears and 16% had lateral meniscus tears. Differences in medial meniscal extrusion between loading and unloading were significant in the entire cohort (p < 0.0001). Statistically significant difference in medial meniscus extrusion with loading and unloading were found for KL score group of 0, 1 and 3 (p < 0.001, p < 0.001 and p = 0.005). Interestingly, no significant differences in extrusion with loading and unloading were found for the lateral meniscus (p = 0.07).
Conclusion
Our study demonstrated that medial meniscal extrusion significantly increased during loading, specifically in those low KL scores (0 and 1) and in KL score of 3. Loaded MRI may more accurately determine the extent of medial meniscal extrusion in particular in those with no to minimal OA.
1. Introduction
The meniscus is essential in the normal physiologic function of the knee. Important roles of the meniscus include shock absorption, load bearing, and joint stability. The ability of the meniscus to perform these functions is significantly limited by tears of the meniscus and meniscus extrusion. Failure of the meniscus to respond to fluctuating load bearing may lead to articular cartilage damage and progression of osteoarthritis [1]. Multiple studies have shown that meniscal extrusion is an independent predictor of tibiofemoral cartilage loss and degenerative subchondral marrow changes [2], [3], [4], [5], [6]. Along with high BMI and MR-depicted degenerative lesions, meniscus tears and extrusion are strong risk factors for more rapid cartilage loss [7]. Accurate determination of meniscal extrusion and the degree of meniscal extrusion is therefore important in the evaluation of osteoarthritis and progression of degenerative changes.
Abnormal medial meniscus extrusion is defined as protrusion of the body of the medial meniscus beyond the tibial plateau, by more than 3 mm [8]. Meniscus extrusion is commonly associated with severe meniscal tears or root tears that disrupt the hoop tension of the meniscus [1]. However, meniscus extrusion may also be present without an associated meniscal tear. Knee malalignment and tibiofemoral cartilage loss are both associated with meniscus extrusion, independent of meniscal tears [1]. Therefore, it is important to evaluate for meniscus extrusion, regardless of the presence or absence of a meniscal tear.
Meniscus extrusion is evaluated with magnetic resonance imaging (MRI), typically with the patient’s knee in supine, neutral position. However, cadaveric and patient studies show that the meniscus is mobile with varying knee position [8], [9]. Many dynamic imaging configurations have been evaluated, including flexing or rotating the knee or with the patient sitting or standing [8], [9], [10]. Simulation of weight bearing or loading can also be done with the patient in supine position. Stehling et al. [11] examined the effect of weight bearing on meniscus extrusion using a pulley device that transmitted 50% of the subjects’ body weight through a footplate position against the test lower extremity. This study showed that medial meniscus extrusion is greater with loaded versus unloaded MRI of the knee in a group of 30 subjects with osteoarthritis. The purpose of our study was to expand on that prior study by examining a larger cohort and also determine if changes in meniscal extrusion were more significant with more progressive osteoarthritis and with meniscal tears.
2. Materials and methods
2.1. Subjects
The study design was approved by the institutional Human Research Protection Program, and all procedures were performed in accordance with the Health Insurance Portability and Accountability Act (HIPAA).
143 subjects were recruited through research flyers. Subjects were initially screened by phone, and if eligible (as outlined below), underwent anterior-posterior knee radiography in an extended, weight-bearing position. These radiographs were scored for the presence of osteoarthritis by musculoskeletal radiologists according to the Kellgren-Lawrence (KL) scoring system. According to this system, KL score 0 is no osteoarthritis, 1 is doubtful osteoarthritis (minute osteophyte), 2 is minimal osteoarthritis (osteophytes but no joint space narrowing), 3 is moderate (osteophytes and joint space narrowing), and 4 is severe osteoarthritis (severe joint space narrowing and subchondral sclerosis) [12], [13]. Inclusion criteria for control subjects were age ≥35, no history of frequent knee pain, aching, or stiffness over the past year and no use of medication for knee pain in the past year. In addition, radiographs could not show evidence of osteoarthritis. Inclusion criteria for osteoarthritis subjects were age ≥35, self-reported pain, aching or stiffness most days of a month in the past year, and radiographic signs of osteoarthritis with a KL score of 2, 3, or 4. Exclusion criteria for both groups included history of fracture or surgery to the study knee and contraindication to MRI. The details of the experiment with all risks, benefits, and alternatives were explained to the subjects, and informed consent was obtained, with use of a form approved by the Committee on Human Research.
2.2. MR imaging
All imaging studies were performed in the Department of Radiology and Biomedical Imaging at the University of California, San Francisco. MRI of the subjects studied knees was performed using a 3T GE Excite HDx MR scanner (General Electric, Milwaukee, WI) with a dedicated 8-channel knee coil (Invivo, Orlando, FL, USA). The MRI protocol included the following sequences: (1) a high-resolution 3D fast spin-echo CUBE sequence for clinical grading and soft tissue segmentation (repetition time (TR)/echo time (TE) = 1500/26.69 ms, field of view = 16 cm, matrix = 384 × 384, slice thickness = 0.5 mm, echo train length = 32, bandwidth = 37.5 kHz, number of excitations (NEX) = 0.5, acquisition time = 10.5 min) (2) the T 1ρ relaxation time sequence (TR/TE = 9/2.6 ms, time of recovery = 1500 ms, field of view = 14 cm, matrix = 256 × 128, slice thickness = 4 mm, bandwidth = 62.5 kHz, time of spin-lock (TSL) = 0/2/4/8/12/20/40/80 ms, frequency of spin-lock = 500 Hz, acquisition time = 11 min) and (3) the T 2 relaxation time sequence (same as the T 1ρ quantification except for magnetization preparation TE = 1.8/3.67.3/14.5/29.1/43. 6/58.2, acquisition time = 11 min). Coronal images were reformatted from the 3D fast spin-echo CUBE sequences. The first phase of MRI consisted of unloaded imaging. This was achieved by having subjects rest in a chair with the knee in an unloaded position for 45 min prior to the beginning of the MRI. Subjects were then positioned on the MR scanner table in the supine position with their knees in neutral position, fully extended (Fig. 1a). After the unloaded imaging sequences were completed, knee loading was achieved with a custom-made loading device simulating standing by applying an axial load to the leg of 50% body weight [11] (Fig. 1b). Following 10 min of loading, the same MR sequences were repeated.
Fig. 1.
MRI-compatible axial loading device. (a) For unloaded imaging, the subject is in neutral position with the leg extended. (b) For loaded imaging, hanging weights equaling half of the patient’s body weight are applied to the frame that. The force of the weight is transmitted through a series of pulleys to the patient’s foot.
2.3. Image analysis
All MR images of the knees were evaluated on picture archiving and communication system PACS workstations (Agfa, Ridgefield Park, NJ). Sagittal T2 FSE CUBE sequences from both loaded and unloaded conditions were reformatted in the coronal plane using the PACS workstations. The body of the meniscus was determined to be at the midportion of the tibial plateau. The distance from the outermost aspect of the tibial plateau articular cartilage to the outermost edge of the body of the meniscus was measured and reported in mm (Fig. 2). These measurements were performed on unloaded and loaded imaging. A musculoskeletal radiologist with 3 years of experience in musculoskeletal imaging scored the images for meniscal extrusion. The images were also independently scored for meniscal tears. Each meniscus, medial and lateral, was graded for presence or absence of meniscal tear. The meniscal tears were further categorized as non-displaced or displaced (Fig. 3, Fig. 4, Fig. 5, Fig. 6 ).
Fig. 2.
Method of meniscus extrusion measurement. The distance from the outermost aspect of the tibial plauteau articular cartilage (solid line) to the outermost edge of the body of the meniscus (dashed line) was measured and reported in mm.
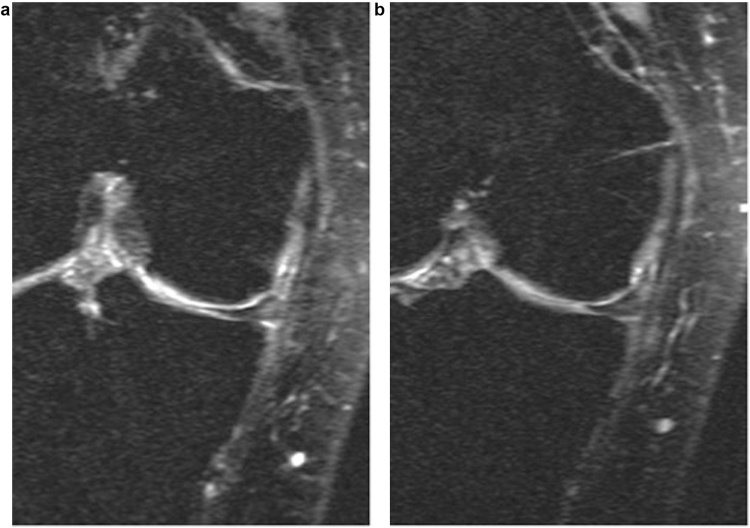
Fig. 3.
52-year-old female with KL score of 1. These images show increased measurement of medial meniscus extrusion from (a) unloaded to (b) loaded conditions. With loading, there is increase in medial meniscus extrusion.
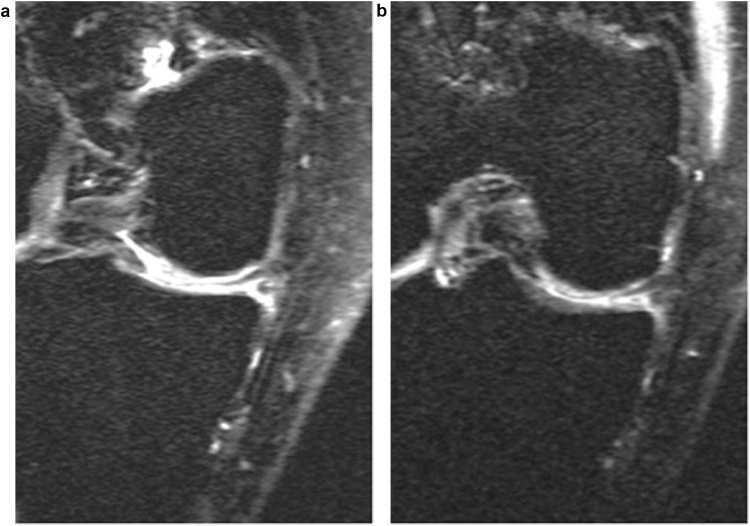
Fig. 4.
59-year-old female with KL score of 1. There is no significant change in the lateral meniscus under (a) unloaded and (b) loaded conditions. No significant difference in meniscus position is noted.
Fig. 5.
69-year-old female with KL score 2. There is increased medial meniscus extrusion under (a) unloaded and (b) loaded conditions. The medial meniscus in this subject was torn. The torn meniscus is more extruded with loading.
Fig. 6.
Comparison of unloading and loading on the medial meniscus for subjects with increasing KL score. This series of images shows the medial meniscus under unloaded (left column) and loaded (right column) conditions. The subject in the top row has KL Score of 0, followed by 1, 2, 3 and KL score of 4 in the bottom row. All subjects show some increase in medial meniscus extrusion. Although the difference in unloading versus loading seems more apparent with higher KL score versus lower KL score in this group of subjects, no statistically significant difference was noted in the study population.
2.4. Statistical analysis
Descriptive statistics are expressed as mean ± SD. Continuous variables were examined for normality with the Kolmogorov-Smirnov univariate normality test. Frequencies of discrete variables were generated. Knee outcomes were compared between the loaded and unloaded groups using Student’s t-test. Criterion values were adjusted for unequal variances where appropriate. Estimation of between-group differences in those outcomes involving covariate adjustment used analysis of covariance (ANCOVA). All statistical tests were performed at the two-sided p value 0.05 level of significance. Statistical analysis was performed using SAS, version 9.4 (SAS Institute, Inc., Cary, NC, USA) and MedCalc (MedCalc Software bvba, Belgium).
3. Results
3.1. Subject characteristics
The cohort included 87 women and 56 men (61% and 39% of the total 143, respectively). The distribution of patient age ranged from 35 to 72 years old, mean of 53 years. The distribution of KL score was as follows: 56 patients with KL score of 0, 46 patients with KL score of 1, 25 patients with KL score of 2, 13 patients with KL score of 3, and 3 patients with KL score of 4 (Table 1). The cohort also included 39 patients with medial meniscus tears (24%; 109 (76%) without) and 23 patients with lateral meniscus tears (16%; 120 (84%) without).
Table 1.
KL score distribution.
| KL Score | Number | Age Range | Female | Male |
|---|---|---|---|---|
| 0 | 56 (39%) | 35–72 yo | 33 (59%) | 23 (41%) |
| 1 | 46 (32%) | 38–72 yo | 28 (61%) | 18 (39%) |
| 2 | 25 (17%) | 42–72 yo | 15 (60%) | 10 (40%) |
| 3 | 13 (9%) | 41–72 yo | 9 (69%) | 4 (31%) |
| 4 | 3 (2%) | 55–64 yo | 2 (67%) | 1 (33%) |
3.2. Changes under loading versus unloading for the entire cohort
The mean measurement of medial meniscus extrusion was significantly different between unloading (mean measurement of 1.0 mm) and loading (mean measurement of 1.8 mm, p < 0.0001). The differences in medial meniscus extrusion with loading and unloading are described in Table 2. The differences between lateral meniscus extrusion in unloaded and loaded conditions were not statistically significant. The mean measurement of lateral meniscus extrusion was 0.3 mm with unloaded conditions and 0.5 mm with loaded conditions (p = 0.072). The differences in lateral meniscus extrusion with loading and unloading are described in Table 3.
Table 2.
Change in medial meniscus extrusion with loading versus unloading.
| Medial Meniscus extrusion (in mm) | Unloading |
Loading |
Statistical analysis (p) | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| KL Score 0 | 1.0 | 0.7 | 1.6 | 0.9 | <0.0001 |
| KL Score 1 | 1.1 | 0.7 | 2.0 | 1.0 | <0.0001 |
| KL Score 2 | 1.4 | 1.1 | 2.1 | 1.3 | 0.052 |
| KL Score 3 | 0.9 | 0.6 | 1.8 | 0.8 | 0.005 |
| KL Score 4 | 0.7 | 0.4 | 1.2 | 0.3 | 0.097 |
| Entire cohort | 1.0 | 0.8 | 1.8 | 1.0 | <0.0001 |
Table 3.
Change in lateral meniscus extrusion with loading versus unloading.
| Lateral Meniscus extrusion (in mm) | Unloading |
Loading |
Statistical analysis (p) | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| KL Score 0 | 0.3 | 0.5 | 0.4 | 0.6 | 0.315 |
| KL Score 1 | 0.4 | 0.6 | 0.6 | 0.1 | 0.233 |
| KL Score 2 | 0.4 | 0.1 | 0.5 | 0.1 | 0.407 |
| KL Score 3 | 0.1 | 0.1 | 0.2 | 0.1 | 0.626 |
| KL Score 4 | 0.1 | 0.1 | 0.1 | 0.1 | 1.000 |
| Entire cohort | 0.3 | 0.5 | 0.5 | 0.6 | 0.07 |
3.3. Changes under loading for different KL scores
The change in meniscus extrusion with loading versus unloading was also examined for each KL score group (Table 2). The differences in medial meniscus extrusion between loading and unloading remained statistically significant across KL scores 0, 1 and 3. For those with KL score of 0, measurement of medial meniscus extrusion measured 1.0 mm with unloading and 1.6 mm with loading (p < 0.0001). For those with KL score of 1, measurement of medial meniscus extrusion measured 1.1 mm with unloading and 2.0 mm with loading (p < 0.0001). For those with KL score of 2, measurement of medial meniscus extrusion measured 1.4 mm with unloading and 2.1 mm with loading (p = 0.052). For those with KL score of 3, measurement of medial meniscus extrusion measured 0.9 mm with unloading and 1.8 mm with loading (p = 0.005). For those with KL score 4, measurement of medial meniscus extrusion measured 0.7 with unloading and 1.2 with loading (p = 0.09). No statistically significant difference was found for subjects with KL score of 2 or 4. Accounting for differing KL score, the difference between medial meniscus extrusion with loading and was not statistically significant (p = 0.38).
No statistically significant difference was found for lateral meniscus extrusion for any KL score group. These differences are outlined in Table 3. Differences between lateral meniscus extrusion in unloaded and loaded conditions were also not statistically significant when accounting for differing KL score (p = 0.31).
3.4. Meniscal tears
The menisci were also evaluated for presence or absence of meniscal tear. Of the 143 patients, 120 did not have a lateral meniscus tear and 23 did (84% and 16%, respectively). A non-displaced tear was found in 14 of the 23 with lateral meniscus tears (10% of the total cohort) and a displaced tear or maceration was found in 9 (6% of the total cohort). There were 109 without a medial meniscus tear and 34 with a medial meniscus tear (76% and 24%, respectively). There were 19 (13% of the total cohort) who had a non-displaced medial meniscus tear and 15 with displaced tear or maceration (10% of the total cohort). There was significantly more extrusion of the medial meniscus with loading than with unloading in those who had any medial meniscus tear (p = 0.002). There was also increased medial meniscus extrusion in those with increased severity of meniscal tear (no tear compared to nondisplaced tear compared to displaced tear) (p = 0.005; Table 4). There was no significant difference in lateral meniscus extrusion with unloading or loading in those with a lateral meniscus tear (p = 0.714).
Table 4.
Change in medial meniscus extrusion with loading versus unloading according to presence or absence of meniscal tear.
| Medial Meniscus extrusion (in mm) | Unloading |
Loading |
Statistical analysis (p) | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| No meniscus tear | 1.0 | 0.7 | 1.7 | 1.0 | <0.0001 |
| Non-displaced meniscus tear | 1.4 | 0.8 | 2.0 | 0.8 | <0.0001 |
| Displaced meniscus tear | 1.5 | 1.1 | 2.5 | 1.3 | <0.0001 |
4. Discussion
Our study is the largest to date to evaluate the impact of weighted imaging of the knee at 3T field strength MRI and serves to corroborate findings suggested by earlier, smaller studies that subjects demonstrate increased medial meniscal extrusion on weighted imaging compared to non-weighted imaging. Furthermore, our study also found that the increased medial meniscal extrusion is seen with in patients with meniscal tears and those with low KL score. Although prior studies have shown that increased meniscal extrusion with loading is seen in patients with abnormal KL score (KL score 2 and 3) compared to those with KL score 0, our study found meniscal extrusion to be significantly different only in patients with KL score of 0, 1, and 3. No statistically significant difference was found in patients with KL score of 2, though there was a statistical trend to increased extrusion. Finally, no statistically significant difference was found for lateral meniscus extrusion on weighted compared to non-weighted imaging for any KL score group in our cohort.
Early identification of peripheral meniscal extrusion is paramount, as multiple studies have suggested a relationship between peripheral meniscal extrusion and chondral degradation [2], [4]. This is even more crucial in light of the Multicenter Osteoarthritis (MOST) study’s finding that meniscal extrusion is an independently strong predictor of fast rather than slow cartilage loss [7]. Radiologists routinely recognize peripheral meniscal extrusions associated with meniscal tears including radial and root tears, but meniscal tears are not the only factors associated with meniscal extrusions and peripheral meniscal extrusions may be present in the absence of meniscal tears [1]. Identification of such peripheral meniscal extrusions without associated meniscal tear can be challenging on routine MRI and results in under-diagnosis. A promising application of weighted imaging of the knee is early evaluation and diagnosis of peripheral meniscal extrusion, especially in those without associated meniscal tear or in those with no or minimal osteoarthritis.
Stehling previously reviewed 30 subjects and found that loading of the knee is associated with medial meniscal extrusion in mild and moderate osteoarthritis (KL score 2 and 3) [11]. Our study also found increased meniscal extrusion with loading versus unloading, but found this difference was significant only in those with low KL score (0 and 1) and moderate osteoarthritis (KL score 3). Although no statistically significant difference between meniscal extrusion in loading and unloading was found for KL score 2, there was a statistical trend towards increased extrusion with loading in this KL score group. The finding of statistically significant difference in KL score group 0 and 1 is promising. This finding suggests that weighted MRI of the knee may be a sensitive measure of meniscal extrusion in those with no osteoarthritis or minimal findings of osteoarthritis. In addition to the above findings, there was also significant difference in meniscal extrusion between loading and unloading in those with meniscal tears. This finding is concordant with findings from Stehling et al. [11]. However, loading did not significantly change lateral meniscus extrusion in those with lateral meniscus tears.
There are several limitations to our study. First, the musculoskeletal radiologist who interpreted degree of meniscal extrusion was not blinded to the unloaded and loaded sequences, which may affect measurements. Secondly, the population size of the higher KL score group was much smaller than the lower KL score group. More than half of the cohort was KL score of 0 or 1. Those with a KL score of 3 or 4 accounted for only 11% of the cohort. This variance in population size amongst KL score groups could affect the findings, including the finding of lack of significant difference between loading and unloading in the higher KL score groups. Future directions of study include examining larger groups of patients with KL score 3 or 4 to determine the effect of loading on meniscus extrusion with high KL score. Finally, the ability to perform weighted imaging of the knee in the clinical setting assumes a certain comfort level by the patient and expertise by the technologist performing the exam.
In conclusion, increased medial meniscal extrusions are seen in all subjects on loaded MRI compared to non-loaded MRI. The degree of medial meniscal extrusion is significantly different between loaded and unloaded MRI in those with no osteoarthritis or minimal osteoarthritis (KL score of 0 and 1). Although prior studies have shown a trend towards increasing differences in extrusion with increasing KL score, our study did not support this finding.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Acknowledgements
The project described was supported by Grant Numbers R01 AR062370, R01 AR46906, and P50 AR060752, from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. These grants provided funding for the completion of the MRI exams used for this study.
References
- 1.Crema M.D., Roemer F.W., Felson D.T. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the Multicenter Osteoarthritis study. Radiology. 2012;264(2):494–503. doi: 10.1148/radiol.12110986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berthiaume M.J., Raynauld J.P., Martel-Pelletier J. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann. Rheum. Dis. 2005;64(4):556–563. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Englund M., Guermazi A., Roemer F.W. Meniscal pathology on MRI increases the risk for both incident and enlarging subchondral bone marrow lesions of the knee: the MOST Study. Ann. Rheum. Dis. 2010;69(10):1796–1802. doi: 10.1136/ard.2009.121681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hunter D.J., Zhang Y.Q., Niu J.B. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54(3):795–801. doi: 10.1002/art.21724. [DOI] [PubMed] [Google Scholar]
- 5.MacLeod T.D., Subburaj K., Wu S., Kumar D., Wyatt C., Souza R.B. Magnetic resonance analysis of loaded meniscus deformation: a novel technique comparing participants with and without radiographic knee osteoarthritis. Skeletal Radiol. 2015;44(1):125–135. doi: 10.1007/s00256-014-2022-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Y., Wluka A.E., Pelletier J.P. Meniscal extrusion predicts increases in subchondral bone marrow lesions and bone cysts and expansion of subchondral bone in osteoarthritic knees. Rheumatology. 2010;49(5):997–1004. doi: 10.1093/rheumatology/keq034. [DOI] [PubMed] [Google Scholar]
- 7.Roemer F.W., Zhang Y., Niu J. Tibiofemoral joint osteoarthritis: risk factors for MR-depicted fast cartilage loss over a 30-month period in the multicenter osteoarthritis study. Radiology. 2009;252(3):772–780. doi: 10.1148/radiol.2523082197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boxheimer L., Lutz A.M., Treiber K. MR imaging of the knee. Invest. Radiol. 2004;39(5):254–263. doi: 10.1097/01.rli.0000116895.04239.84. [DOI] [PubMed] [Google Scholar]
- 9.Vedi V., Williams A., Tennant S.J., Spouse E., Hunt D.M., Gedroyc W.M. Meniscal movement: an in-vivo study using dynamic MRI. J. Bone Joint Surg. Br. 1999;81(1):37–41. doi: 10.1302/0301-620x.81b1.8928. [DOI] [PubMed] [Google Scholar]
- 10.Boxheimer L., Lutz A.M., Zanetti M. Characteristics of displaceable and nondisplaceable meniscal tears at kinematic MR imaging of the knee. Radiology. 2006;238(1):221–231. doi: 10.1148/radiol.2381041234. [DOI] [PubMed] [Google Scholar]
- 11.Stehling C., Souza R.B., Hellio Le Graverand M.P. Loading of the knee during 3.0 T MRI is associated with significantly increased medial meniscus extrusion in mild and moderate osteoarthritis. Eur. J. Radiol. 2012;81(8):1839–1845. doi: 10.1016/j.ejrad.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Petersson I.F., Boegard T., Saxne T., Silman A.J., Svensson B. Radiographic osteoarthritis of the knee classified by the Ahlback and Kellgren & Lawrence systems for the tibiofemoral joint in people aged 35–54 years with chronic knee pain. Ann. Rheum. Dis. 1997;56(8):493–496. doi: 10.1136/ard.56.8.493. [DOI] [PMC free article] [PubMed] [Google Scholar]