Abstract
Cholangiocarcinoma (CCA) represents a diverse group of epithelial cancers associated with the biliary tract, and can best be stratified anatomically into intrahepatic (iCCA), perihilar (pCCA) and distal (dCCA) subsets. Molecular profiling has identified genetic aberrations associated with these anatomic subsets. For example, IDH catalytic site mutations and constitutively active FGFR2 fusion genes are predominantly identified in iCCA, whereas KRAS mutations and PRKACB fusions genes are identified in pCCA and dCCA. Clinical trials targeting these specific driver mutations are in progress. However, The Tumor Genome Atlas (TCGA) marker analysis of CCA also highlights the tremendous molecular heterogeneity of this cancer rendering comprehensive employment of targeted therapies challenging. CCA also display a rich tumor microenvironment which may be easier to target. For example, targeting cancer associated fibroblasts for apoptosis with BH3-mimetics and/or and reversing T-cell exhaustion with immune check point inhibitors may help aid in the treatment of this otherwise devastating malignancy. Combinatorial therapy attacking the tumor microenvironment plus targeted therapy may help advance treatment for CCA. This article is part of a Special Issue entitled: Cholangiocytes in Health and Disease edited by Jesus Banales, Marco Marzioni, Nicholas LaRusso and Peter Jansen.
Keywords: Cholangiocarcinoma, Biliary tract cancer, Molecular targets, Driver mutations, Microenvironment
1. Introduction
Cholangiocarcinoma (CCA) remains one of the most dismal tumors with very limited therapeutic options. CCA that are detected at very early stages can be amendable to resection with curative intent, especially peripherally located intrahepatic CCAs, or can be included in a protocol of neoadjuvant radio-chemotherapy with subsequent liver transplantation for perihilar CCA (pCCA) [1]. For tumors beyond these narrow limitations of curative surgical treatment, no other curative therapeutic options exist. CCA comprises a very heterogeneous group of tumors not only with respect to localization (intrahepatic, extrahepatic, perihilar) and pathological subtypes but also regarding genetic makeup [2,3]. The enormous genetic variability still poses a mayor challenge for effective pharmacological treatment. Current systemic therapy is limited to Gemcitabine plus Cisplatin which remains the standard of care but is palliative and of modest benefit [4]. Two non-mutually exclusive approaches are being pursued to address this therapeutic gap in hepatobiliary neoplasia. First, it is anticipated that detailed genetic analysis will identify driver mutations in subsets of patients which can be targeted. The second approach is based on targeting the rich tumor microenvironment of this cancer. Both approaches will be discussed in detail below.
2. Genetic mutations and therapeutic opportunities
The development of whole genome sequencing has taken the search for therapeutic targets in CCA to a new level. For the first time, targeted and individualized therapeutic approaches to this devastating tumor appear possible. At the same time, next-generation sequencing also reveals the complexity and heterogeneity of the different types of CCA and requires a differentiated discussion of driver mutations and drugable targets in different subtypes of CCA [5,6]. In the first part this review will focus on the most prominent molecular alterations and the observations for therapeutics currently in clinical and pre-clinical trials will be discussed. (See Fig. 1.)
Fig. 1.
Summary of some of the most promising tumor cell targeted therapeutic approaches in CCA. Besides the important FGFR2 mutations, mutations in cMET, Her2, IDH and PRKACA/B are promising new targets. Numbers in parenthesis indicate current clinical trials.
2.1. Cyclin-dependent kinase inhibitor 2A/B (CDKN2A/B)
Mutations of CDKN2, also called p16INK4a have been described in 15–20% of CCA, predominantly pCCA and dCCA. Inactivating mutations result in deregulation of cell cycle control by the INK4 family proteins p16 and p14ARF. Mutations or hypermethylation result in loss of S-phase inhibition by p16 or G1 to G2 phase control by p14ARF. Focal losses of CDKN2A as well as epigenetic silencing were frequently found in a set of 38 CCA analyzed by the Cancer Genome Atlas Network (TCGN). 47% of the CCA examined showed some loss or mutation of CDKN2 [7]. These data suggest cyclin dependent kinase (CDK) may be beneficial in a subset of CCA. This concept certainly has been overlooked in CCA biology and merits further examination.
2.2. KRAS
As in many malignomas, activating KRAS mutations are frequently detected in all subtypes of CCA and can be found in up to 40% of CCA, predominantly in perihilar and distal CCA [8,9]. Downstream signaling pathways of KRAS include the PI3K-AKT-mTOR as well as the Raf-MEK-ERK axis. Direct therapeutic inhibition of activated KRAS has proven elusive. Instead, inhibition of activated downstream signaling molecules such as MEK, AKT or mTOR is the current therapeutic strategy, as discussed below. Given the intense crosstalk between the signaling pathways downstream of KRAS and possible resistance mechanisms, combination of inhibitors targeting different redundant signaling pathways seems to be the most promising strategy. Co-targeting with a MEK inhibitor and the multi-kinase inhibitor ponatinib for example has shown promising effects in pancreatic cancer cells and in-vivo models [10].
Since there are no direct KRAS inhibitors available today, targeted therapy aims at modulation of downstream signaling along the KRAS pathway. The MEK 1/2 inhibitor selumetinib was evaluated in a phase II trial in advanced biliary tract cancer with perhaps modest effect [11]. Likewise, combination of standard of care Cis/Gem with selumetinib in a phase I trial for patients with advanced biliary tract cancer showed a signal for efficacy while adverse events were acceptable. Further trials targeting the KRAS signaling pathway with MEK inhibitors combined with other therapeutics are ongoing (NCT02042443; NCT01438554).
2.3. mTOR pathway
Several of the common oncogenic mutations in CCA, such as KRAS, MET or FGF converge on the pro-proliferative mTOR signaling pathway. Therefor targeting the mTOR pathway appears as an attractive targeted therapeutic strategy in CCA [12]. Again, redundancy in signaling pathways and signaling crosstalk, particularly with the MEK-ERK pathway makes combination therapies targeting several signaling molecules most promising [13].
Targeting the PI3/AKT/mTOR pathway in human malignancies is a one of the main novel therapeutic approaches. Accordingly, a large number of clinical trials are currently evaluating selective inhibitors [14]. Inhibition of more than one of the signaling molecules is probably necessary to circumvent feedback activation and signaling crosstalk, such as AKT activation by mTOR inhibition [13]. Combination of the mTOR inhibitor everolimus with the standard Cis/Gem did result in stable disease in 6/10 patients with advanced CCA. Current, mTOR inhibitors approved by regulatory agencies for use in man only inhibit the mTOR 1 complex; likely dual mTOR 1 and 2 inhibitors, which are in development, may be more effective for this disease.
2.4. Hedgehog signaling pathway
Activation of the Hedgehog (Hh) signaling pathway has been described in cholangiocarcinoma [15]. Activation of the canonical Hh signaling pathway confers apoptosis resistance in CCA via the cell cycle controlling polo-like kinase 2 (PLK2). Interestingly this pathway depends on intact primary cilia on the cell surfaces. Preclinical studies have shown an antiproliferative effect of the Hh inhibitor cyclopamine with reduction of PLK expression in experimental CCA [16]. In addition to the canonical Hh signaling pathway a non-canonical Hh signaling mechanism has been described particularly in CCA cells which often show a loss of primary cilia. Non-canonical Hh signaling promotes CCA tumor progression and inhibition of this signaling pathway with a specific antagonist to the Hh receptor protein Smoothened resulted in reduced tumor growth and metastasis in a murine model of CCA [17]. Hedgehog signaling inhibitors are approved for use in patients with germ line mutations given rise to basal cell carcinomas [18]. Given the lack of mutations affecting this pathway in CCA, the pharmaceutical industry has been reluctant to invest in testing Hedgehog signaling inhibitors for this disease.
2.5. FGFR gene fusions
Of the potentially targetable diver mutations specifically found in iCCA, mutations that alter fibroblast growth factor (FGF) signaling, primarily by FGF receptor 2 (FGFR2) gene fusions are among the most frequent, occurring in 10 up to 45% of all iCCA [19]. FGF downstream signaling pathways that become activated by FGF fusion proteins include the RAS-RAF-MEK-MAPK axis. MAPK signaling in particular has been implicated in increased cancer cell motility possibly promoting a ductular growth and a desmoplastic tumor microenvironment. Still the prognostic value of FGFR2 fusion mutations remains controversial as some studies report improved survival in patients with FGFR2 mutations while others describe no difference [20,21].
Based on positive preclinical data for FGFR inhibition from murine xenograft models of iCCA, several FGFR inhibitors have entered early clinical trials [22]. The unselective FGFR inhibitor BGJ398 did show anti-tumor activity and acceptable side effects in a phase I clinical trial of 132 patients with solid organ tumors and known FGFR mutations. An ongoing phase II clinical trial of second-line BGJ398 in CCA patients with FGFR mutations after unsuccessful platinum based first-line treatment reports an astonishing 82% disease control rate in these advanced stage CCA patients (NCT02150967) [23].
Erdafitinib (JNJ-42756493) is a second pan-FGFR small molecule kinase inhibitor currently under investigation in clinical trials [24]. Erdafitinib showed anti-tumor activity only in the 21 patients with FGFR mutations while 36 patients that did not have confirmed FGFR mutations had no significant response.
The ATP competitive small molecule kinase inhibitor ARQ 087 has demonstrated anti-proliferative activity in cell lines with various activating FGFR mutations. ARQ 087 has meanwhile entered a phase 1/2 clinical trial in patients with confirmed FGFR mutations. The study has enrolled iCCA patients with FGFR2 gene fusion mutations (NCT01752920). Several other FGFR kinase inhibitors, such as AZD4547, TAS120 and CH5183284/Debio 1347 are in early clinical trials after promising pre-clinical results (NCT02052778; NCT01948297).
Besides the selective FGFR inhibitors, unselective kinase inhibitors have been evaluated in patients with CCA and FGFR mutations. Ponatinib and pazopanib have demonstrated activity in individual patients with very advanced iCCA and FGFR fusion mutations [25]. Based on these promising data, ponatinib is being examined in a phase II trial of patients with advanced biliary tract cancer and known FGFR fusion mutations (NCT02265341).
Reversible inhibitors of FGFR such as BGJ398 appear to be subject to resistance development as has been demonstrated in recent studies of resistant patients [26]. Irreversible FGFR inhibition by novel covalently binding small molecules may circumvent this back draw of earlier compounds [27].
In addition to small molecule inhibitors, the monoclonal antibody FPA144 that is specific for the mutated FGFR2b isoform is currently being tested in patients with malignant tumors that overexpress or have amplified this particular receptor isoform (NCT02318329).
Given the very heterogeneous mutational landscape of CCA combination therapies that target more than one pertinent signaling pathway are probably the best strategy. With this in mind, the combination of the MEK inhibitor trametinib with the FGFR2 inhibitor pazobanib is currently being evaluated in a phase I clinical trial for solid tumors including CCA (NCT 01438554).
2.6. MET/HGF
About 7% of iCCA display activating mutations in the MET signaling axis. MET is the tyrosine kinase receptor for hepatocyte growth factor (HGF) and exerts effects on cell proliferation, motility and sensitivity to apoptotic cell death [28]. Overexpression of MET on the protein level was seen in up to 60% of iCCA [29], primarily in well differentiated iCCA. MET inhibitors may represent a novel approach to this subset of iCCA.
Inhibition of the MET signaling pathway by specific kinase inhibitors is a therapeutic concept in numerous malignant tumors. The oral MET inhibitor tivantinib has been evaluated in CCA patients in combination with gemcitabine with positive results, reaching response or stable disease in about 50 and 30% of patients respectively [30]. Besides tivantinib the MET inhibitor cabozantinib is under investigation in a phase II trial in advanced CCA that has failed first and second line chemotherapy (NCT01954745).
2.7. Mcl-1
Mcl-1 is an anti-apoptotic member of the Bcl-2 family of proteins that has been found overexpressed in around 20% of iCCA [8,31]. Mcl-1 confers resistance to apoptotic cell death by inhibition of the mitochondrial pathway of apoptosis. Mcl-1 upregulation by inflammatory IL6 signaling has been demonstrated in CCA [32]. IL6 induced upregulation of MCl-1 is conferred by downregulation of AKT as well as the JAK/STAT pathway [33]. Therapeutic interference with this signaling mechanism has been demonstrated to result in normalization of Mcl-1 expression and apoptotic sensitization of CCA cells. At the same time amplification of Mcl-1 itself can be observed in CCA, making direct targeting with novel Mcl-1 inhibitors a potential new treatment strategy. Kotschy and colleagues recently described S63845, a small molecule BH-3 mimetic that binds and inhibits Mcl1 with high affinity. In mechanistic studies S63845 potently killed Mcl1-dependent cancer cells by activation of the BAX/BAK-dependent mitochondrial pathway of apoptosis. S63845 showed good anti-tumor efficacy and acceptable safety as a single agent in several cancers [20].
2.8. Isocytrate dehydrogenase 1/2 (IDH 1/2)
Mutations in the α-ketoglutarate synthesizing enzymes IDH 1 and 2 are found in up to 30% of iCCA [19,31] and much less frequent in pCCA. Several known IDH mutations result in dysfunctional enzymes and lead to increased intracellular levels of 2-hydroxyglutarate which induces epigenetic changes and thus shows a diverse array of oncogenic effects [34]. Given the oncogenic mechanism, inhibition of mutated IDH isoforms seems a feasible approach. The question remains whether inhibition of IDH is still effective in a situation where malignant transformation has already taken place.
The occurrence of IDH mutations in various malignant tumors has fostered the development of specific inhibitors and has resulted in several clinical trials evaluating IDH inhibitor compounds. AG-120 is an oral selective inhibitor of mutant IDH1 was well tolerated and has demonstrated therapeutic activity with reduction of 2-HG levels in solid tumors including CCA. A follow-up trial in CCA patients with known IDH1 mutations is about to enroll patients in the near future (NCT02989857). Patients with solid tumors that carry IDH2 mutations can be enrolled in the clinical trials evaluating the inhibitor of mutant IDH2, the orally bioavailable compound AG-221 (NCT02273739).
2.9. Protein tyrosine phosphatases (PTP)
PTPs dephosphorylate tyrosine residues in a multitude of proteins [35]. Alterations in the PTP function can be oncogenic. A study of 124 iCCA with paired non-tumor tissue showed activating mutations of PTPN3 in more than 40% of iCCA with resulting tumor promoting activity and higher iCCA recurrence rates. PTP gain of function mutations appear functionally highly relevant, potentially drugable and are therefore promising novel therapeutic targets [36].
2.10. Chromatin remodeling
In a recent study of 32 iCCA, almost 50% were found to have one or more mutation in genes important for chromatine remodeling [6]. Genes that were frequently inactivated in iCCA were BAP1, a deubiquitinase that participates in chromatin remodeling, furthermore PBRM1 and ARID1A (AT-rich interactive domain-containing protein 1A), both subunits of the chromatin remodeling complexes SWI/SNF. All of the aforementioned mutations seem to result in worse overall survival [6]. A recent large multicenter study of comprehensive genomic profiling (CGP) in CCA identified ARID1A as one of the most frequent mutations in iCCA [37]. Mutations were found in close to 20% of 412 iCCA specimens.
Currently the main therapeutic approach to chromatin remodeling relies on small molecule inhibition of histone deacetylase (HDAC) and DNA methyltransferase (DNMT). The HDAC inhibitors include vorinostat and romidepsin, small molecule DNMTs are azacitidine and decitabine [38]. So far there are no clinical trials of drugs targeting chromatin remodeling in CCA.
Enhancer of zeste homolog 2 (EZH2), a histone methyltransferase has been identified as epigenetic modulator frequently upregulated in various cancers [39,40]. Proposed mechanisms of malignancy are activation of p-ERK-β-catenin signaling [41] and downregulation of TIMP with subsequent increased invasiveness [42]. Inhibitors of EZH2 are currently under investigation [43].
2.11. EGF/HER2
Particularly in pCCA oncogenic activation of the epidermal growth factor signaling pathway has been described. The four receptors of the epidermal growth factor receptor family (ERBB) are EGFR (ERBB1), Her-2/neu (ERBB2) as well as ERBB3 and ERBB4 [44]. In several studies, activating mutations of Her-2/neu (ERBB2) have been described in about 20% of pCCA and dCCA in contrast to only 1–2% of iCCA [8,20,37]. Combined irreversible inhibition of activated EGFR and Her-2/neu that also circumvents resistance conveyed by kinase domain mutated ERBB is a promising target and most likely more effective than reversible inhibition by erlotinib that showed only limited effect in clinical studies [45,46].
As described above for dCCA, Her-2/neu mutations are frequent also in dCCA. 10–15% of ampullary carcinomas show genetic alterations of the Her-2/neu (ERBB2) signaling pathway [47]. As described above the multitude of signaling crosstalk downstream of the ERBB receptors makes combined inhibition of more than one target molecule the most promising approach. Clinical trials with the reversible Her-2/neu (ERBB2) inhibitor erlotinib have had only limited success in CCA [45,46]. This may be due to the prevalence of kinase domain mutations in CCA that confer resistance to reversible kinase inhibitors. The recently described activating ERBB2 kinase mutation V777L was resistant to reversible inhibition by lapatinib but showed sensitivity to the irreversible inhibitor nertatinib [48]. This probably indicates that irreversible ERBB2 inhibition (neratinib, afatinib, dacomatinib) is necessary in the heterogeneous CCA setting.
2.12. Protein kinase cyclic AMP (PKA) pathway
Protein kinase cyclic AMP activated catalytic subunit alpha (PRKACA) and beta (PRKACB). Fusion genes that result in enhanced expression of PRKACA and B have only recently been described in pCCA and dCCA [49]. PRKACA and B function as subunits of PKA and increased activation results in enhanced MAPK signaling. Further activating mutations in PKA regulatory subunits have been described in single cases of pCCA/dCCA and exhibit oncogenic effects through downstream activation of MAPK, PI3K, JAK/STAT and Wnt/b-catening signaling [50]. The identification of the PRKACA and PRKACA fusion genes in a subset of pCCA is of high level interest as a therapeutic target. Another PRKACA fusion gene has been implicated in the pathogenesis of fibrolamellar hepatocellular carcinoma [51], and drugs are being developed for this target, which hopefully will also inhibit the PRKACB fusions.
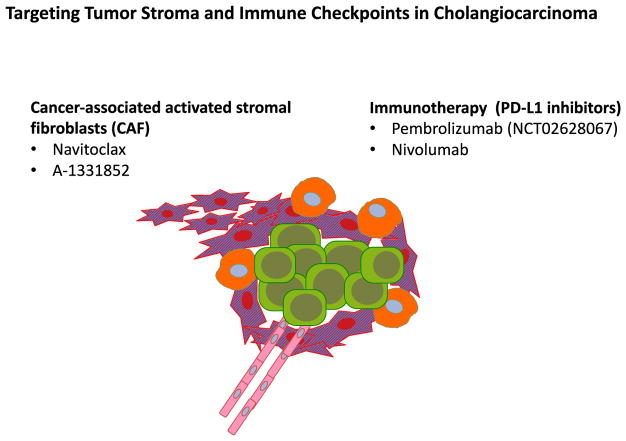
3. Targeting CCA tumor stroma
The tremendous genetic heterogeneity of CCA cells renders targeting genetic aberrations difficult [52]. Targeting the much less genetically diverse stromal compartment is an attractive alternative strategy. Moreover, CCA is a particularly desmoplastic, stroma-rich tumor entity [53]. Activated stromal fibroblasts, also called cancer associated fibroblasts (CAF) often outnumber the actual tumor cells by several fold. CAF appear to support tumor growth and metastasis [54]. Clinical studies have reported that the number of CAF in CCA specimens is inversely correlated with patient survival [55]. This supports the concept that CAF play an important role for the biology and aggressiveness of CCA. We have demonstrated earlier that CAF, much like activated fibroblasts in acute and chronic liver injury, are sensitized for apoptotic cell death a state also termed ‘apoptotic priming’ [56]. Small molecule pro-apoptotic compounds, so called BH-3 mimetics exploit this apoptotic priming and induce apoptosis in sensitized cells. Accordingly, BH3 mimetics reduced tumor growth and metastasis and improved survival in a murine model of CCA [56,57]. These encouraging results should warrant further clinical studies targeting stroma in patients with cholangiocarcinoma.
4. Immunotherapy in CCA
Immune checkpoints maintain self-tolerance and prevent damage to normal tissue during an immune response. Cancers frequently exploit these immune checkpoints as resistance mechanism to evade immune surveillance. Reconstituting normal anti-tumor immunity by blockade of immune checkpoints is a novel and promising new therapeutic approach in cancer. The cytotoxic T lymphocyte associated protein 4 (CTLA-4) plays a critical role in the regulation of T-cell tolerance and has become a main focus of immunotherapy. Anti-CTLA-4 monoclonal antibodies have meanwhile entered clinical cancer therapy and have proven highly effective in several cancer entities. Likewise, the programmed death 1 (PD-1) and programmed death ligand 1 (PD-L1) inhibitors are meanwhile in clinical use for cancer immunotherapy. Upregulation of immune checkpoint molecules was seen in 45% of 260 biliary tract cancer that were subject to molecular characterization [49]. Upregulation of PD-1/PD-L1 was demonstrated in a different set of intrahepatic CCA [58]. Dysregulation of immune checkpoint molecules was associated with less differentiated histology, more advanced tumor stage and worse outcome while HLA 1 overexpression seems to have inverse effect [59]. There is very few data on clinical use of immune therapeutics in CCA. The anti-PD-1 antibody pembrolizumab is currently under investigation in Phase 1/2 studies. Preliminary data show promising efficacy in CCA with about 40% response rate. A Phase II trial is ongoing (NCT02628067). The PD-L1 inhibitor nivolumab has just been approved for hepatocellular carcinoma but data for cholangiocarcinoma are still missing.
5. Conclusion and perspective
After decades of little progress in systemic treatment for CCA, advances in genetic profiling including second generation sequencing have opened the door for identification of specific and even individual therapeutic targets in this dismal cancer. This has in a second step led to identification of drugable targets and candidate molecules. Some are widely known from many different types of cancer, others are more specific for cholangiocarcinoma. Among the most advanced and promising strategies for CCA are the attempts to influence FGFR mutations, the therapies targeting EGFR, in particular Her-2 mutations and the trials on IDH directed treatments.
Many more molecular targets require further investigation, high-throughput screening for therapeutic molecules and preclinical and clinical testing. To identify candidates and avoid false negative study results, a more diligent and differentiated stratification of patients according to CCA subtypes, mutational landscape and disease stage is necessary. A novel clinical staging system may facilitate stratification but further augmentation with genetic information and biomarkers will be crucial to successful trials with novel compounds [60]. The extensive inter- but also intratumoral heterogeneity of CCA will most likely require a multimodal, multiagent therapy. At the same time, potentially tumor supporting stromal cells, such as activated stromal fibroblasts and inflammatory cells may represent valuable targets besides the actual cancer cells. In preclinical trials, cancer associated fibroblasts in CCA are sensitized for apoptosis and can be therapeutically targeted with pro-apoptotic BH3 mimetics [56]. The increasing interest and attention that CCA receives from investigators as well as pharmaceutical industry and the formation of new and driven interest groups augurs well for the urgently needed advancement of therapy [61]. (See Fig. 2.)
Fig. 2.
The tumor ‘ecosystem’ contains abundant activated cancer associated stromal fibroblasts beside the actual tumor cells. These activated fibroblast support tumor development and are sensitive to apoptosis induction by BH3 mimetics such as Navitoclax. Depletion of CAF reduces tumor growth in a murine model of CCA. PD-L1 inhibition reconstitutes T-cell response and anti-tumor immunity. Such inhibitors are established in other tumor entities and are currently under investigation for CCA.
Supplementary Material
Abbreviations
- CCA
Cholangiocarcinoma
- iCCA
Intrahepatic CCA
- pCCA
Perihilar CCA
- dCCA
Distal CCA
- CDK
Cyclin dependent kinase
- CDKN2A/B
Cyclin-dependent kinase inhibitor 2A/B
- PLK2
Polo-like kinase 2
- FGF
Fibroblast growth factor
- HGF
Hepatocyte growth factor
- IDH 1/2
Isocytrate dehydrogenase 1/2
- PTP
Protein tyrosine phosphatases
- ARIDA1
AT-rich interactive domain-containing protein 1A
Footnotes
This article is part of a Special Issue entitled: Cholangiocytes in Health and Disease edited by Jesus Banales, Marco Marzioni, Nicholas LaRusso and Peter Jansen.
The http://dx.doi.org/10.1016/j.bbadis.2017.08.027 associated with this article can be found, in the online version.
References
- 1.Rizvi S, Gores GJ. Pathogenesis, diagnosis, and management of cholangiocarcinoma. Gastroenterology. 2013;145:1215–1229. doi: 10.1053/j.gastro.2013.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Komuta M, Govaere O, Vandecaveye V, Akiba J, Van Steenbergen W, Verslype C, Laleman W, Pirenne J, Aerts R, Yano H, Nevens F, Topal B, Roskams T. Histological diversity in cholangiocellular carcinoma reflects the different cholangiocyte phenotypes. Hepatology. 2012;55:1876–1888. doi: 10.1002/hep.25595. [DOI] [PubMed] [Google Scholar]
- 3.Rizvi S, Borad MJ, Patel T, Gores GJ. Cholangiocarcinoma: molecular pathways and therapeutic opportunities. Semin Liver Dis. 2014;34:456–464. doi: 10.1055/s-0034-1394144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, Madhusudan S, Iveson T, Hughes S, Pereira SP, Roughton M, Bridgewater J Investigators ABCT. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362:1273–1281. doi: 10.1056/NEJMoa0908721. [DOI] [PubMed] [Google Scholar]
- 5.Ong CK, Subimerb C, Pairojkul C, Wongkham S, Cutcutache I, Yu W, McPherson JR, Allen GE, Ng CC, Wong BH, Myint SS, Rajasegaran V, Heng HL, Gan A, Zang ZJ, Wu Y, Wu J, Lee MH, Huang D, Ong P, Chanon W, Cao Y, Qian CN, Lim KH, Ooi A, Dykema K, Furge K, Kukongviriyapan V, Sripa B, Wongkham C, Yongvanit P, Futreal PA, Bhudhisawasdi V, Rozen S, Tan P, Teh BT. Exome sequencing of liver fluke-associated cholangiocarcinoma. Nat Genet. 2012;44:690–693. doi: 10.1038/ng.2273. [DOI] [PubMed] [Google Scholar]
- 6.Jiao Y, Pawlik TM, Anders RA, Selaru FM, Streppel MM, Lucas DJ, Niknafs N, Guthrie VB, Maitra A, Argani P, Offerhaus GJ, Roa JC, Roberts LR, Gores GJ, Popescu I, Alexandrescu ST, Dima S, Fassan M, Simbolo M, Mafficini A, Capelli P, Lawlor RT, Ruzzenente A, Guglielmi A, Tortora G, de Braud F, Scarpa A, Jarnagin W, Klimstra D, Karchin R, Velculescu VE, Hruban RH, Vogelstein B, Kinzler KW, Papadopoulos N, Wood LD. Exome sequencing identifies frequent inactivating mutations in BAP1, ARID1A and PBRM1 in intrahepatic cholangiocarcinomas. Nat Genet. 2013;45:1470–1473. doi: 10.1038/ng.2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farshidfar F, Zheng S, Gingras MC, Newton Y, Shih J, Robertson AG, Hinoue T, Hoadley KA, Gibb EA, Roszik J, Covington KR, Wu CC, Shinbrot E, Stransky N, Hegde A, Yang JD, Reznik E, Sadeghi S, Pedamallu CS, Ojesina AI, Hess JM, Auman JT, Rhie SK, Bowlby R, Borad MJ, Zhu AX, Stuart JM, Sander C, Akbani R, Cherniack AD, Deshpande V, Mounajjed T, Foo WC, Torbenson MS, Kleiner DE, Laird PW, Wheeler DA, McRee AJ, Bathe OF, Andersen JB, Bardeesy N, Roberts LR, Kwong LN Cancer Genome Atlas N. Integrative genomic analysis of cholangiocarcinoma identifies distinct IDH-mutant molecular profiles. Cell Rep. 2017;18:2780–2794. doi: 10.1016/j.celrep.2017.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Churi CR, Shroff R, Wang Y, Rashid A, Kang HC, Weatherly J, Zuo M, Zinner R, Hong D, Meric-Bernstam F, Janku F, Crane CH, Mishra L, Vauthey JN, Wolff RA, Mills G, Javle M. Mutation profiling in cholangiocarcinoma: prognostic and therapeutic implications. PLoS One. 2014;9:e115383. doi: 10.1371/journal.pone.0115383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu AX, Borger DR, Kim Y, Cosgrove D, Ejaz A, Alexandrescu S, Groeschl RT, Deshpande V, Lindberg JM, Ferrone C, Sempoux C, Yau T, Poon R, Popescu I, Bauer TW, Gamblin TC, Gigot JF, Anders RA, Pawlik TM. Genomic profiling of intrahepatic cholangiocarcinoma: refining prognosis and identifying therapeutic targets. Ann Surg Oncol. 2014;21:3827–3834. doi: 10.1245/s10434-014-3828-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sahu N, Chan E, Chu F, Pham T, Koeppen H, Forrest W, Merchant M, Settleman J. Cotargeting of MEK and PDGFR/STAT3 Pathways to Treat Pancreatic Ductal Adenocarcinoma. Mol Cancer Ther. 2017;16(9):1729–1738. doi: 10.1158/1535-7163.MCT-17-0009. [DOI] [PubMed] [Google Scholar]
- 11.Bekaii-Saab T, Phelps MA, Li X, Saji M, Goff L, Kauh JS, O’Neil BH, Balsom S, Balint C, Liersemann R, Vasko VV, Bloomston M, Marsh W, Doyle LA, Ellison G, Grever M, Ringel MD, Villalona-Calero MA. Multi-institutional phase II study of selumetinib in patients with metastatic biliary cancers. J Clin Oncol. 2011;29:2357–2363. doi: 10.1200/JCO.2010.33.9473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yothaisong S, Dokduang H, Techasen A, Namwat N, Yongvanit P, Bhudhisawasdi V, Puapairoj A, Riggins GJ, Loilome W. Increased activation of PI3K/AKT signaling pathway is associated with cholangiocarcinoma metastasis and PI3K/mTOR inhibition presents a possible therapeutic strategy. Tumour Biol. 2013;34:3637–3648. doi: 10.1007/s13277-013-0945-2. [DOI] [PubMed] [Google Scholar]
- 13.Ewald F, Grabinski N, Grottke A, Windhorst S, Norz D, Carstensen L, Staufer K, Hofmann BT, Diehl F, David K, Schumacher U, Nashan B, Jucker M. Combined targeting of AKT and mTOR using MK-2206 and RAD001 is synergistic in the treatment of cholangiocarcinoma. Int J Cancer. 2013;133:2065–2076. doi: 10.1002/ijc.28214. [DOI] [PubMed] [Google Scholar]
- 14.Sheppard K, Kinross KM, Solomon B, Pearson RB, Phillips WA. Targeting PI3 kinase/AKT/mTOR signaling in cancer. Crit Rev Oncog. 2012;17:69–95. doi: 10.1615/critrevoncog.v17.i1.60. [DOI] [PubMed] [Google Scholar]
- 15.Jinawath A, Akiyama Y, Sripa B, Yuasa Y. Dual blockade of the Hedgehog and ERK1/2 pathways coordinately decreases proliferation and survival of cholangiocarcinoma cells. J Cancer Res Clin Oncol. 2007;133:271–278. doi: 10.1007/s00432-006-0166-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fingas CD, Bronk SF, Werneburg NW, Mott JL, Guicciardi ME, Cazanave SC, Mertens JC, Sirica AE, Gores GJ. Myofibroblast-derived PDGF-BB promotes Hedgehog survival signaling in cholangiocarcinoma cells. Hepatology. 2011;54:2076–2088. doi: 10.1002/hep.24588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Razumilava N, Gradilone SA, Smoot RL, Mertens JC, Bronk SF, Sirica AE, Gores GJ. Non-canonical Hedgehog signaling contributes to chemotaxis in cholangiocarcinoma. J Hepatol. 2014;60:599–605. doi: 10.1016/j.jhep.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Von Hoff DD, LoRusso PM, Rudin CM, Reddy JC, Yauch RL, Tibes R, Weiss GJ, Borad MJ, Hann CL, Brahmer JR, Mackey HM, Lum BL, Darbonne WC, Marsters JC, Jr, de Sauvage FJ, Low JA. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361:1164–1172. doi: 10.1056/NEJMoa0905360. [DOI] [PubMed] [Google Scholar]
- 19.Sia D, Losic B, Moeini A, Cabellos L, Hao K, Revill K, Bonal D, Miltiadous O, Zhang Z, Hoshida Y, Cornella H, Castillo-Martin M, Pinyol R, Kasai Y, Roayaie S, Thung SN, Fuster J, Schwartz ME, Waxman S, Cordon-Cardo C, Schadt E, Mazzaferro V, Llovet JM. Massive parallel sequencing uncovers actionable FGFR2-PPHLN1 fusion and ARAF mutations in intrahepatic cholangiocarcinoma. Nat Commun. 2015;6:6087. doi: 10.1038/ncomms7087. [DOI] [PubMed] [Google Scholar]
- 20.Kotschy A, Szlavik Z, Murray J, Davidson J, Maragno AL, Le Toumelin-Braizat G, Chanrion M, Kelly GL, Gong JN, Moujalled DM, Bruno A, Csekei M, Paczal A, Szabo ZB, Sipos S, Radics G, Proszenyak A, Balint B, Ondi L, Blasko G, Robertson A, Surgenor A, Dokurno P, Chen I, Matassova N, Smith J, Pedder C, Graham C, Studeny A, Lysiak-Auvity G, Girard AM, Grave F, Segal D, Riffkin CD, Pomilio G, Galbraith LC, Aubrey BJ, Brennan MS, Herold MJ, Chang C, Guasconi G, Cauquil N, Melchiore F, Guigal-Stephan N, Lockhart B, Colland F, Hickman JA, Roberts AW, Huang DC, Wei AH, Strasser A, Lessene G, Geneste O. The MCL1 inhibitor S63845 is tolerable and effective in diverse cancer models. Nature. 2016;538:477–482. doi: 10.1038/nature19830. [DOI] [PubMed] [Google Scholar]
- 21.Arai Y, Totoki Y, Hosoda F, Shirota T, Hama N, Nakamura H, Ojima H, Furuta K, Shimada K, Okusaka T, Kosuge T, Shibata T. Fibroblast growth factor receptor 2 tyrosine kinase fusions define a unique molecular subtype of cholangiocarcinoma. Hepatology. 2014;59:1427–1434. doi: 10.1002/hep.26890. [DOI] [PubMed] [Google Scholar]
- 22.Rizvi S, Yamada D, Hirsova P, Bronk SF, Werneburg NW, Krishnan A, Salim W, Zhang L, Trushina E, Truty MJ, Gores GJ. A hippo and fibroblast growth factor receptor autocrine pathway in cholangiocarcinoma. J Biol Chem. 2016;291:8031–8047. doi: 10.1074/jbc.M115.698472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Borad MJ, Gores GJ, Roberts LR. Fibroblast growth factor receptor 2 fusions as a target for treating cholangiocarcinoma. Curr Opin Gastroenterol. 2015;31:264–268. doi: 10.1097/MOG.0000000000000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tabernero J, Bahleda R, Dienstmann R, Infante JR, Mita A, Italiano A, Calvo E, Moreno V, Adamo B, Gazzah A, Zhong B, Platero SJ, Smit JW, Stuyckens K, Chatterjee-Kishore M, Rodon J, Peddareddigari V, Luo FR, Soria JC. Phase I dose-escalation study of JNJ-42756493, an oral pan-fibroblast growth factor receptor inhibitor, in patients with advanced solid tumors. J Clin Oncol. 2015;33:3401–3408. doi: 10.1200/JCO.2014.60.7341. [DOI] [PubMed] [Google Scholar]
- 25.Borad MJ, Champion MD, Egan JB, Liang WS, Fonseca R, Bryce AH, McCullough AE, Barrett MT, Hunt K, Patel MD, Young SW, Collins JM, Silva AC, Condjella RM, Block M, McWilliams RR, Lazaridis KN, Klee EW, Bible KC, Harris P, Oliver GR, Bhavsar JD, Nair AA, Middha S, Asmann Y, Kocher JP, Schahl K, Kipp BR, Barr Fritcher EG, Baker A, Aldrich J, Kurdoglu A, Izatt T, Christoforides A, Cherni I, Nasser S, Reiman R, Phillips L, McDonald J, Adkins J, Mastrian SD, Placek P, Watanabe AT, Lobello J, Han H, Von Hoff D, Craig DW, Stewart AK, Carpten JD. Integrated genomic characterization reveals novel, therapeutically relevant drug targets in FGFR and EGFR pathways in sporadic intrahepatic cholangiocarcinoma. PLoS Genet. 2014;10:e1004135. doi: 10.1371/journal.pgen.1004135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goyal L, Saha SK, Liu LY, Siravegna G, Leshchiner I, Ahronian LG, Lennerz JK, Vu P, Deshpande V, Kambadakone A, Mussolin B, Reyes S, Henderson L, Sun JE, Van Seventer EE, Gurski JM, Jr, Baltschukat S, Schacher-Engstler B, Barys L, Stamm C, Furet P, Ryan DP, Stone JR, Iafrate AJ, Getz G, Porta DG, Tiedt R, Bardelli A, Juric D, Corcoran RB, Bardeesy N, Zhu AX. Polyclonal secondary FGFR2 mutations drive acquired resistance to FGFR inhibition in patients with FGFR2 fusion-positive cholangiocarcinoma. Cancer Discov. 2017;7:252–263. doi: 10.1158/2159-8290.CD-16-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tan L, Wang J, Tanizaki J, Huang Z, Aref AR, Rusan M, Zhu SJ, Zhang Y, Ercan D, Liao RG, Capelletti M, Zhou W, Hur W, Kim N, Sim T, Gaudet S, Barbie DA, Yeh JR, Yun CH, Hammerman PS, Mohammadi M, Janne PA, Gray NS. Development of covalent inhibitors that can overcome resistance to first-generation FGFR kinase inhibitors. Proc Natl Acad Sci U S A. 2014;111:E4869–4877. doi: 10.1073/pnas.1403438111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Appleman LJ. MET signaling pathway: a rational target for cancer therapy. J Clin Oncol. 2011;29:4837–4838. doi: 10.1200/JCO.2011.37.7929. [DOI] [PubMed] [Google Scholar]
- 29.Terada T, Nakanuma Y, Sirica AE. Immunohistochemical demonstration of MET overexpression in human intrahepatic cholangiocarcinoma and in hepatolithiasis. Hum Pathol. 1998;29:175–180. doi: 10.1016/s0046-8177(98)90229-5. [DOI] [PubMed] [Google Scholar]
- 30.Pant S, Saleh M, Bendell J, Infante JR, Jones S, Kurkjian CD, Moore KM, Kazakin J, Abbadessa G, Wang Y, Chen Y, Schwartz B, Camacho LH. A phase I dose escalation study of oral c-MET inhibitor tivantinib (ARQ 197) in combination with gemcitabine in patients with solid tumors. Ann Oncol. 2014;25:1416–1421. doi: 10.1093/annonc/mdu157. [DOI] [PubMed] [Google Scholar]
- 31.Ross JS, Wang K, Gay L, Al-Rohil R, Rand JV, Jones DM, Lee HJ, Sheehan CE, Otto GA, Palmer G, Yelensky R, Lipson D, Morosini D, Hawryluk M, Catenacci DV, Miller VA, Churi C, Ali S, Stephens PJ. New routes to targeted therapy of intrahepatic cholangiocarcinomas revealed by next-generation sequencing. Oncologist. 2014;19:235–242. doi: 10.1634/theoncologist.2013-0352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kobayashi S, Werneburg NW, Bronk SF, Kaufmann SH, Gores GJ. Interleukin-6 contributes to Mcl-1 up-regulation and TRAIL resistance via an Akt-signaling pathway in cholangiocarcinoma cells. Gastroenterology. 2005;128:2054–2065. doi: 10.1053/j.gastro.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 33.Isomoto H, Kobayashi S, Werneburg NW, Bronk SF, Guicciardi ME, Frank DA, Gores GJ. Interleukin 6 upregulates myeloid cell leukemia-1 expression through a STAT3 pathway in cholangiocarcinoma cells. Hepatology. 2005;42:1329–1338. doi: 10.1002/hep.20966. [DOI] [PubMed] [Google Scholar]
- 34.Grassian AR, Pagliarini R, Chiang DY. Mutations of isocitrate dehydrogenase 1 and 2 in intrahepatic cholangiocarcinoma. Curr Opin Gastroenterol. 2014;30:295–302. doi: 10.1097/MOG.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 35.Julien SG, Dube N, Hardy S, Tremblay ML. Inside the human cancer tyrosine phosphatome. Nat Rev Cancer. 2011;11:35–49. doi: 10.1038/nrc2980. [DOI] [PubMed] [Google Scholar]
- 36.Gao Q, Zhao YJ, Wang XY, Guo WJ, Gao S, Wei L, Shi JY, Shi GM, Wang ZC, Zhang YN, Shi YH, Ding J, Ding ZB, Ke AW, Dai Z, Wu FZ, Wang H, Qiu ZP, Chen ZA, Zhang ZF, Qiu SJ, Zhou J, He XH, Fan J. Activating mutations in PTPN3 promote cholangiocarcinoma cell proliferation and migration and are associated with tumor recurrence in patients. Gastroenterology. 2014;146:1397–1407. doi: 10.1053/j.gastro.2014.01.062. [DOI] [PubMed] [Google Scholar]
- 37.Javle M, Bekaii-Saab T, Jain A, Wang Y, Kelley RK, Wang K, Kang HC, Catenacci D, Ali S, Krishnan S, Ahn D, Bocobo AG, Zuo M, Kaseb A, Miller V, Stephens PJ, Meric-Bernstam F, Shroff R, Ross J. Biliary cancer: utility of next-generation sequencing for clinical management. Cancer. 2016;122:3838–3847. doi: 10.1002/cncr.30254. [DOI] [PubMed] [Google Scholar]
- 38.Dawson MA, Kouzarides T. Cancer epigenetics: from mechanism to therapy. Cell. 2012;150:12–27. doi: 10.1016/j.cell.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 39.Cao Q, Mani RS, Ateeq B, Dhanasekaran SM, Asangani IA, Prensner JR, Kim JH, Brenner JC, Jing X, Cao X, Wang R, Li Y, Dahiya A, Wang L, Pandhi M, Lonigro RJ, Wu YM, Tomlins SA, Palanisamy N, Qin Z, Yu J, Maher CA, Varambally S, Chinnaiyan AM. Coordinated regulation of polycomb group complexes through microRNAs in cancer. Cancer cell. 2011;20:187–199. doi: 10.1016/j.ccr.2011.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yan KS, Lin CY, Liao TW, Peng CM, Lee SC, Liu YJ, Chan WP, Chou RH. EZH2 in cancer progression and potential application in cancer therapy: a friend or foe? Int J Mol Sci. 2017;18 doi: 10.3390/ijms18061172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chang CJ, Yang JY, Xia W, Chen CT, Xie X, Chao CH, Woodward WA, Hsu JM, Hortobagyi GN, Hung MC. EZH2 promotes expansion of breast tumor initiating cells through activation of RAF1-beta-catenin signaling. Cancer cell. 2011;19:86–100. doi: 10.1016/j.ccr.2010.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yi X, Guo J, Guo J, Sun S, Yang P, Wang J, Li Y, Xie L, Cai J, Wang Z. EZH2-mediated epigenetic silencing of TIMP2 promotes ovarian cancer migration and invasion. Sci Rep. 2017;7:3568. doi: 10.1038/s41598-017-03362-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Knutson SK, Wigle TJ, Warholic NM, Sneeringer CJ, Allain CJ, Klaus CR, Sacks JD, Raimondi A, Majer CR, Song J, Scott MP, Jin L, Smith JJ, Olhava EJ, Chesworth R, Moyer MP, Richon VM, Copeland RA, Keilhack H, Pollock RM, Kuntz KW. A selective inhibitor of EZH2 blocks H3K27 methylation and kills mutant lymphoma cells. Nat Chem Biol. 2012;8:890–896. doi: 10.1038/nchembio.1084. [DOI] [PubMed] [Google Scholar]
- 44.Sirica AE. Role of ErbB family receptor tyrosine kinases in intrahepatic cholangiocarcinoma. World J Gastroenterol. 2008;14:7033–7058. doi: 10.3748/wjg.14.7033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lubner SJ, Mahoney MR, Kolesar JL, Loconte NK, Kim GP, Pitot HC, Philip PA, Picus J, Yong WP, Horvath L, Van Hazel G, Erlichman CE, Holen KD. Report of a multicenter phase II trial testing a combination of biweekly bevacizumab and daily erlotinib in patients with unresectable biliary cancer: a phase II Consortium study. J Clin Oncol. 2010;28:3491–3497. doi: 10.1200/JCO.2010.28.4075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Philip PA, Mahoney MR, Allmer C, Thomas J, Pitot HC, Kim G, Donehower RC, Fitch T, Picus J, Erlichman C. Phase II study of erlotinib in patients with advanced biliary cancer. J Clin Oncol. 2006;24:3069–3074. doi: 10.1200/JCO.2005.05.3579. [DOI] [PubMed] [Google Scholar]
- 47.Yachida S, Wood LD, Suzuki M, Takai E, Totoki Y, Kato M, Luchini C, Arai Y, Nakamura H, Hama N, Elzawahry A, Hosoda F, Shirota T, Morimoto N, Hori K, Funazaki J, Tanaka H, Morizane C, Okusaka T, Nara S, Shimada K, Hiraoka N, Taniguchi H, Higuchi R, Oshima M, Okano K, Hirono S, Mizuma M, Arihiro K, Yamamoto M, Unno M, Yamaue H, Weiss MJ, Wolfgang CL, Furukawa T, Nakagama H, Vogelstein B, Kiyono T, Hruban RH, Shibata T. Genomic sequencing identifies ELF3 as a driver of ampullary carcinoma. Cancer cell. 2016;29:229–240. doi: 10.1016/j.ccell.2015.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bose R, Kavuri SM, Searleman AC, Shen W, Shen D, Koboldt DC, Monsey J, Goel N, Aronson AB, Li S, Ma CX, Ding L, Mardis ER, Ellis MJ. Activating HER2 mutations in HER2 gene amplification negative breast cancer. Cancer Discov. 2013;3:224–237. doi: 10.1158/2159-8290.CD-12-0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nakamura H, Arai Y, Totoki Y, Shirota T, Elzawahry A, Kato M, Hama N, Hosoda F, Urushidate T, Ohashi S, Hiraoka N, Ojima H, Shimada K, Okusaka T, Kosuge T, Miyagawa S, Shibata T. Genomic spectra of biliary tract cancer. Nat Genet. 2015;47:1003–1010. doi: 10.1038/ng.3375. [DOI] [PubMed] [Google Scholar]
- 50.Loilome W, Juntana S, Namwat N, Bhudhisawasdi V, Puapairoj A, Sripa B, Miwa M, Saya H, Riggins GJ, Yongvanit P. PRKAR1A is overexpressed and represents a possible therapeutic target in human cholangiocarcinoma. Int J Cancer. 2011;129:34–44. doi: 10.1002/ijc.25646. [DOI] [PubMed] [Google Scholar]
- 51.Simon EP, Freije CA, Farber BA, Lalazar G, Darcy DG, Honeyman JN, Chiaroni-Clarke R, Dill BD, Molina H, Bhanot UK, La Quaglia MP, Rosenberg BR, Simon SM. Transcriptomic characterization of fibrolamellar hepatocellular carcinoma. Proc Natl Acad Sci U S A. 2015;112:E5916–5925. doi: 10.1073/pnas.1424894112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Greaves M, Maley CC. Clonal evolution in cancer. Nature. 2012;481:306–313. doi: 10.1038/nature10762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mertens JC, Gores GJ. Targeting tumor stroma: exploiting apoptotic priming. Oncotarget. 2012;3:1501–1502. doi: 10.18632/oncotarget.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sirica AE, Campbell DJ, Dumur CI. Cancer-associated fibroblasts in intrahepatic cholangiocarcinoma. Curr Opin Gastroenterol. 2011;27:276–284. doi: 10.1097/MOG.0b013e32834405c3. [DOI] [PubMed] [Google Scholar]
- 55.Chuaysri C, Thuwajit P, Paupairoj A, Chau-In S, Suthiphongchai T, Thuwajit C. Alpha-smooth muscle actin-positive fibroblasts promote biliary cell proliferation and correlate with poor survival in cholangiocarcinoma. Oncol Rep. 2009;21:957–969. doi: 10.3892/or_00000309. [DOI] [PubMed] [Google Scholar]
- 56.Mertens JC, Fingas CD, Christensen JD, Smoot RL, Bronk SF, Werneburg NW, Gustafson MP, Dietz AB, Roberts LR, Sirica AE, Gores GJ. Therapeutic effects of deleting cancer-associated fibroblasts in cholangiocarcinoma. Cancer Res. 2013;73:897–907. doi: 10.1158/0008-5472.CAN-12-2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rizvi S, Mertens JC, Bronk SF, Hirsova P, Dai H, Roberts LR, Kaufmann SH, Gores GJ. Platelet-derived growth factor primes cancer-associated fibroblasts for apoptosis. J Biol Chem. 2014;289:22835–22849. doi: 10.1074/jbc.M114.563064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ye Y, Zhou L, Xie X, Jiang G, Xie H, Zheng S. Interaction of B7-H1 on intrahepatic cholangiocarcinoma cells with PD-1 on tumor-infiltrating T cells as a mechanism of immune evasion. J Surg Oncol. 2009;100:500–504. doi: 10.1002/jso.21376. [DOI] [PubMed] [Google Scholar]
- 59.Sabbatino F, Villani V, Yearley JH, Deshpande V, Cai L, Konstantinidis IT, Moon C, Nota S, Wang Y, Al-Sukaini A, Zhu AX, Goyal L, Ting DT, Bardeesy N, Hong TS, Fernandez-del Castillo C, Tanabe KK, Lillemoe KD, Ferrone S, Ferrone CR. PD-L1 and HLA class I antigen expression and clinical course of the disease in intrahepatic cholangiocarcinoma. Clin Cancer Res. 2016;22:470–478. doi: 10.1158/1078-0432.CCR-15-0715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chaiteerakij R, Harmsen WS, Marrero CR, Aboelsoud MM, Ndzengue A, Kaiya J, Therneau TM, Sanchez W, Gores GJ, Roberts LR. A new clinically based staging system for perihilar cholangiocarcinoma. Am J Gastroenterol. 2014;109:1881–1890. doi: 10.1038/ajg.2014.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Banales JM, Cardinale V, Carpino G, Marzioni M, Andersen JB, Invernizzi P, Lind GE, Folseraas T, Forbes SJ, Fouassier L, Geier A, Calvisi DF, Mertens JC, Trauner M, Benedetti A, Maroni L, Vaquero J, Macias RI, Raggi C, Perugorria MJ, Gaudio E, Boberg KM, Marin JJ, Alvaro D. Expert consensus document: cholangiocarcinoma: current knowledge and future perspectives consensus statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA) Nat Rev Gastroenterol Hepatol. 2016;13:261–280. doi: 10.1038/nrgastro.2016.51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.