Summary
In his homage to Lucretius (‘Georgica’), Vergil is credited with stating: ‘Felix qui potuit rerum cognoscere causas’ (‘Fortunate is he who knows the causes of things’). Based on numerous commentaries and publications it is obvious that clinicians, diagnosticians and biomedical research scientists continue to struggle with disease causation, particularly in the assessment of the pathogenic role of ‘stealth pathogens’ that produce persistent infections in the host. Bartonella species, because of their evolutionary ability to induce persistent intravascular infections, present substantial challenges for researchers attempting to clarify the ability of these stealth bacteria to cause disease. By studying the comparative biological and pathological behaviour of microbes across mammalian genera, researchers might be able more rapidly to advance medical science and, subsequently, patient care by undertaking focused research efforts involving a single mammalian species or by attempting to recapitulate a complex disease in an rodent model. Therefore, in an effort to further assist in the establishment of disease causation by stealth pathogens, we use recent research observations involving the genus Bartonella to propose an additional postulate of comparative infectious disease causation to Koch's postulates.
Keywords: disease, infection, pathology, Koch's postulates
Persistent Infection and Complex Disease Causation
Based on his work related to anthrax and the detection of the tubercle bacillus, Robert Koch proposed a set of postulates for establishing disease causation by an infectious agent on March 24, 1882, in Berlin, Germany (Loeffler, 1884; Tabrah, 2011). With strong support from the scientific community, these postulates ultimately became the foundation for establishing the pathogenic role of a microorganism in a disease process. The original postulates included (1) the organism must be regularly associated with the disease and its characteristic lesions, (2) the organism must be isolated from the diseased host and grown in culture and (3) the disease must be reproduced when a pure culture of the organism is introduced into a healthy susceptible host. Subsequently, a fourth postulate was added by Friedrich August Loeffler, a German physician: (4) the same organism must be reisolated from the experimentally infected host (Tabrah, 2011).
In 1988, in recognition of the advances in technology related to microbial identification and classification, Falkow proposed an alternative set of ‘molecular Koch's postulates', which could be applied to microbial studies designed to examine the role of specific genes and their products in the pathogenesis of infection and disease (Falkow, 1988). These postulates included (1) the phenotype or property under investigation should be associated with pathogenic members of a genus or pathogenic strains of a species, (2) specific inactivation of the gene(s) associated with the suspected virulence trait should lead to a measurable loss in pathogenicity or virulence, or the gene(s) associated with the suspected virulence trait should be isolated by molecular methods. Specific inactivation or deletion of the gene(s) should lead to loss of function, (3) reversion or allelic replacement of the mutated gene should lead to restoration of pathogenicity, or the replacement of the modified gene(s) for its allelic counterpart in the strain of origin should lead to loss of function and loss of pathogenicity or loss of virulence. Restoration of pathogenicity should accompany the reintroduction of the wild type gene(s). Subsequently, in 1996, Fredericks and Relman proposed molecular Koch's postulates based primarily on sequence-based identification of microbial pathogens (Fredericks and Relman, 1996).
In conjunction with an enhanced understanding of the complexity of microbial pathogenesis, particularly as occurs in association with fastidious or unculturable organisms, polymicrobial infections and chronic or persistent infections, the number of postulates continued to increase. Seven postulates were proposed including (1) a nucleic acid sequence belonging to the putative pathogen should be present in most cases of an infectious disease. Microbial nucleic acids should be found preferentially in those organs or gross anatomical sites known to be diseased and not in those organs that lack pathology, (2) fewer, or no, copy numbers of pathogen-associated nucleic acid sequences should occur in hosts or tissues without disease, (3) with resolution of disease, the copy number of pathogen-associated nucleic acid sequences should decrease or become undetectable. With clinical relapse, the opposite should occur, (4) when sequence detection predates disease or sequence copy number correlates with severity of disease or pathology, the sequence–disease association is more likely to be a causal relationship, (5) the nature of the microorganism inferred from the available sequence should be consistent with the known biological characteristics of that group of organisms, (6) tissue–sequence correlates should be sought at the cellular level and efforts should be made to demonstrate specific in-situ hybridization of the microbial sequence to areas of tissue pathology and to visible microorganisms or to areas where microorganisms are presumed to be located and (7) these sequence-based forms of evidence for microbial causation should be reproducible. Fredericks and Relman concluded that the power of Koch's postulates comes not from their rigid application, but from the spirit of scientific rigour that they foster and that proof of disease causation rests on the concordance of scientific evidence, with Koch's postulates serving as guidelines for collecting the evidence (Fredericks and Relman, 1996). When reflecting on the molecular postulates years later, Stanley Falkow emphasized that there is still no microbiological consensus as to what definitively constitutes a pathogen (Falkow, 2004). With the advent of data from the human microbiome project, it is becoming obvious that in addition to host and environmental factors, complex interactions among microbial populations may ultimately contribute to complexities of chronic disease expression.
In 2002, Jacomo et al. suggested that Koch's observation that the blood should be free of bacteria would not be applicable for establishing disease causation for the genus Bartonella (Jacomo et al., 2002). In 2004, Merrell and Falkow proposed that clinicians, microbiologists and research scientists divide pathogenic infectious agents into two major categories: ‘frontal pathogens’ and ‘stealth pathogens’ (Merrell and Falkow, 2004). Frontal pathogens typically induce an acute infection, while stealth pathogens are characterized by persistent infections for protracted periods of time. Factors that differentiate between stealth and frontal pathogens are summarized in Table 1 . Causation associated with frontal pathogens can in most instances be established using the original Koch's postulates. In contrast, establishing causation for stealth pathogens, particularly in the context of chronic disease causation, is more likely to be successful when the more recently proposed molecular Koch's postulates are applied to investigations of disease pathogenesis. In addition to considering the attributes of frontal versus stealth pathogens, this important and insightful discussion focused on two specific stealth pathogens, Helicobacter pylori and Bartonella henselae (Merrell and Falkow, 2004).
Table 1.
Features that facilitate differentiation of frontal versus stealth pathogens
| Frontal | Stealth | |
|---|---|---|
| Incubation | Short (hours to days) | Long (months to years) |
| Symptoms | Acute | Chronic |
| Immunity | Sterilizing | Non-sterilizing |
| Transmission | Direct | Indirect |
| Replication | Rapid | Slow |
| Carrier state | Uncommon | Common |
Adapted from Merrell and Falkow (2004).
The aim of the present review is to extend previous discussions of disease causation induced by stealth bacterial pathogens, using members of the genus Bartonella as contemporary microbial examples of bacteria that can potentially induce chronic intravascular infection and complex disease expression. These Gram-negative alpha proteobacteria cause long lasting intra-erythrocytic and endotheliotropic infections in reservoir hosts and chronic relapsing bacteraemias following opportunistic infections of non-reservoir hosts (Chomel et al., 2009a; Breitschwerdt et al., 2010a). Importantly, we wish to emphasize the comparative medical importance and pathogenic relevance of combining clinical, microbiological and pathological observations across animal genera and species in order to elucidate the capacity of a specific microorganism (or a combination of microorganisms in the context of co-infections) to cause similar disease manifestations or pathology in more than one mammalian species. Based on recent research observations derived from studies involving the genus Bartonella, we propose that the following postulate be added to Koch's postulates in order to assist in the establishment of disease causation by stealth pathogens: causation can be established if the same infectious agent (or combination of agents) is isolated or organism-specific DNA sequences are amplified from a naturally occurring pathological entity found in at least three different mammalian genera. Although the selection of a minimum of three different mammalian genera is arbitrary, the strength of this type of association would be supported by the fact that random detection of microbial DNA of a specific organism in a defined pathological lesion obtained from different animal genera, occurring spontaneously in nature at different time points, would have a low probability of being an unrelated occurrence. We suggest that the new postulate be referred to as the ‘postulate of comparative infectious disease causation’. Examples involving Bartonella will be given below to illustrate the potential application of this suggested addition to Koch's postulates. It is important to acknowledge that some stealth pathogens may not induce infection in three or more mammalian genera with the ultimate induction of a defined pathological lesion and, as such, other postulates or other approaches would be necessary to infer disease causation for those organisms.
Bartonella spp. Infection and Vasoproliferative Pathology
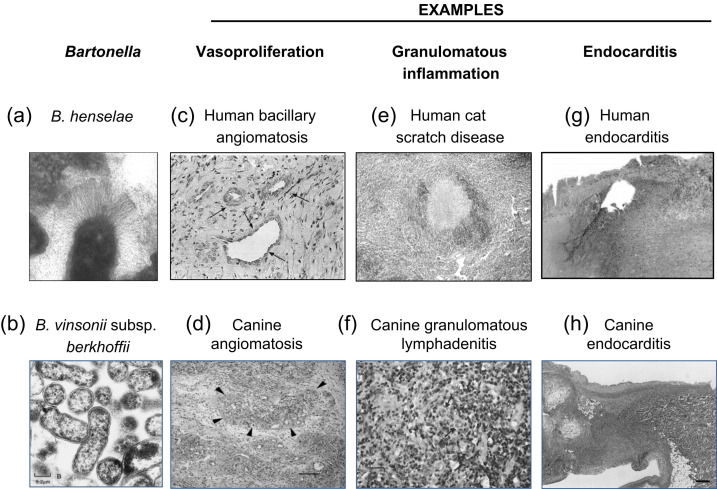
In North America prior to the 1990s, Bartonella spp. were not known to infect man or animals. If it were not for the acquired immunodeficiency syndrome (AIDS) epidemic and the recognition of two prototypical vasoproliferative lesions in this population of immunocompromised patients, it is likely that much of the contemporary literature about the genus Bartonella, as pathogens of increasing microbiological relevance in human and veterinary medicine, would not exist. Early in the 1990s, Bartonella quintana and B. henselae were implicated as the cause of bacillary angiomatosis (BA), a vasoproliferative lesion of the skin, which subsequently was described most often in immunocompromised patients infected with the human immunodeficiency virus (HIV) (Koehler and Tappero, 1993). Recently, BA was reported for the first time in an iatrogenically-immunosuppressed dog infected with Bartonella vinsonii subsp. berkhoffii (Yager et al., 2010). In Fig. 1 , vasoproliferation associated with B. henselae infection in a human patient is compared with a similar histopathological lesion in a dog, only in association with B. vinsonii subsp. berkhoffii infection. This observation was of comparative microbiological relevance in the context of disease pathogenesis, as subsequent studies documented the ability of B. vinsonii subsp. berkhoffii to induce the production of vascular endothelial growth factor (VEGF) (Beerlage et al., 2012), as previously described for B. quintana and B. henselae in human patients. Interestingly, immunosuppression apparently contributed to the subsequent development of BA in this dog, as has been documented for HIV-infected BA patients. On a comparative pathological basis, B. henselae is the only member of the genus that has been associated with peliosis hepatis (PH; a vasoproliferative lesion in the liver characterized by the presence of irregular blood-filled spaces within the parenchyma) in a human patient or a dog (Koehler et al., 1997; Kitchell et al., 2000). Therefore, DNA of the same Bartonella species has been amplified from dogs and people, both with clinically similar and histopathologically confirmed vasoproliferative lesions (PH and BA).
Fig. 1.
Examples of Bartonella spp.-associated vasoproliferation, granulomatous inflammation and endocarditis. The top images show examples from human patients associated with B. henselae infection, while the bottom images show similar histopathological lesions in dogs associated with B. vinsonii subsp. berkhoffii infection. Images are reproduced with permission from (a) Beerlage et al., 2011, (b) Breitschwerdt et al., 1995, (c) Kempf et al., 2001b, (d) Yager et al., 2010, (e) Kempf et al., 2001a, (f) Pappalardo et al., 2000, (g) Albrich et al., 2004 and (h) Breitschwerdt et al., 1999.
Additionally, in the context of Bartonella spp. and vascular endothelial cell proliferation, the following observations provide additional support for the adoption of a postulate of comparative infectious disease causation. A substantial body of literature now supports the ability of B. henselae, B. quintana, Bartonella bacilliformis and B. vinsonii subsp. berkhoffii to induce the production of VEGF and resultant vasoproliferation of endothelial cells (Kempf et al., 2001b, 2005; Resto-Ruiz et al., 2002; Dehio, 2005; Berrich et al., 2011; Beerlage et al., 2012). In the context of naturally occurring cancers, increased expression of VEGF has been documented in association with several vascular tumours including haemangiosarcoma in dogs (Yonemaru et al., 2006), epithelioid haemangioendothelioma (EHE) (Emamaullee et al., 2010) in human patients and haemangiopericytoma in dogs (Hatva et al., 1996). In 2009, B. vinsonii subsp. berkhoffii genotype II was isolated from a boy with EHE and from a dog with a haemangiopericytoma (Breitschwerdt et al., 2009). Subsequently, infection with B. henselae and Bartonella koehlerae was documented in patients with EHE from Australia and England (Mascarelli et al., 2011) and DNA of B. henselae, B. vinsonii subsp. berkhoffii or both organisms was amplified and sequenced from haemangiopericytomas obtained from dogs, a horse and a red wolf (Beerlage et al., 2012). Thus, intravascular infection with one or more Bartonella spp. has been documented in EHE patients from three continents and in haemangiopericytomas from three hosts, suggesting that persistent intravascular infection with selected Bartonella spp. might contribute to the development of these highly unusual and uncommon vascular tumours in immunocompetent people and in animals, respectively. On a comparative microbiological and pathological basis, B. henselae, B. koehlerae or B. vinsonii subsp. berkhoffii DNA has recently been amplified and sequenced (Beerlage et al., 2012) from formalin-fixed and paraffin wax-embedded tissues from cats (Fuji et al., 2005) and a steer (Breshears and Johnson, 2008) with systemic reactive angiomatosis. This rare disease is characterized pathologically by the proliferation of vessels throughout numerous tissues within the animal's body.
Collectively, the above comparative microbiological and pathological findings served as the basis for a retrospective study designed to determine if Bartonella spp. might play a role in the pathogenesis of canine haemangiosarcoma (a malignant tumour of vascular endothelial cells that generally arises in either the spleen or the right atrium of the heart), one of the most common cancers affecting dogs (Varanat et al., 2011). Using surgically obtained formalin-fixed and paraffin wax-embedded tissue biopsy samples from 50 dogs with splenic haemangiosarcoma, a statistically higher prevalence of Bartonella spp. DNA was found (26%), compared with DNA from haemotropic Mycoplasma spp. (2%) or Babesia spp. (6%) (Varanat et al., 2011). In addition, Bartonella spp. DNA was statistically more prevalent in the spleens of dogs with haemangiosarcoma (26%), compared with the spleens from dogs with lymphoid nodular hyperplasia (10%). Bartonella spp. DNA was not amplified from the spleens of specific pathogen-free research dogs. Although Bartonella spp. DNA was amplified and sequenced from only 26% of the haemangiosarcoma tissues tested, numerous factors could be responsible for the relatively low overall percentage of splenic haemangiosarcomas from which organism-specific DNA sequences were obtained. For example, these tumours are often massive and for technical reasons only a small quantity of tissue was available for DNA extraction and polymerase chain reaction (PCR) amplification, prolonged formalin fixation may have compromised PCR amplification due to DNA cross-linking and DNA degradation, organisms may not have been distributed uniformly throughout the tumour, or infection with a Bartonella spp. may have induced a genetic mutation resulting in neoplastic transformation. Alternatively, documentation of Bartonella spp. DNA in dogs with splenic haemangiosarcoma may reflect preferential localization of these intravascular bacteria to a neoplastic spleen because of defective immune surveillance and, therefore, the bacteria did not contribute to tumourigenesis.Although causation cannot be established by a geographically limited, retrospective study, the comparative microbiological evidence outlined above implicates a potential pathogenic role for Bartonella spp. through the induction of hypoxia inducible factor resulting in overproduction of VEGF (Kempf et al., 2005) in immunocompetent animals and people, including EHE in human patients, haemangiopericytoma and haemangiosarcoma in dogs and systemic reactive angiomatosis in cats. If the association between infection with a Bartonella spp. and haemangiosarcoma is confirmed as causal, the development of a vaccine to prevent Bartonella spp. infections might decrease or eliminate one of the more common and serious malignancies affecting dogs, analogous to the papillomavirus vaccine that was recently introduced to decrease the prevalence of cervical cancer in woman (Jenkins et al., 2012). In summary and on a comparative microbiological and pathological basis, Bartonella spp. may contribute to the development of naturally occurring vasoproliferative tumours in cats, dogs, horses and people, thereby providing molecular support for the proposed Koch's postulate of comparative infectious disease causation.
Bartonella spp. Infection and Granulomatous Inflammation
Historically, granulomatous inflammation (a tissue inflammatory response dominated by macrophages and multinucleated macrophage giant cells) has long been associated with lymphadenopathy in patients with classical cat scratch disease (CSD) (Kempf et al., 2001a; Chomel et al., 2009a; Breitschwerdt et al., 2010a). Additionally, granulomatous hepatitis and/or splenitis (historically referred to as ‘atypical CSD’) have been reported in a subset of patients, particularly children, infected with B. henselae (Gerber et al., 2002; Giladi et al., 2005; Psarros et al., 2012; VanderHeyden et al., 2012). Granulomatous lymphadenitis caused by Bartonella alsatica infection has also been reported in patients with generalized lymphadenopathy (Angelakis et al., 2008). Rabbits are the reservoir hosts for this Bartonella species and infection can seemingly be acquired through contact while hunting or butchering wild rabbits. As reviewed by Breitschwerdt et al. (2010a), granulomatous lymphadenitis, hepatitis, panniculitis, rhinitis, meningitis and encephalitis have been described in dogs infected naturally with B. henselae or B. vinsonii subsp. berkhoffii (Gillespie et al., 2003; Mellor et al., 2006; Cross et al., 2008). Moreover, granulomatous osteomyelitis, an atypical manifestation of CSD in human patients infected with B. henselae (Giladi et al., 2005) occurred in a cat infected with B. vinsonii subsp. berkhoffii (Varanat et al., 2009). In Fig. 1, granulomatous lymphadenitis associated with B. henselae infection in a human patient is compared with a similar histopathological lesion in a dog, only in association with B. vinsonii subsp. berkhoffii infection. Thus, in the context of granulomatous inflammation, the same pathological response has occurred in cats, dogs and human patients when infected naturally with a Bartonella spp., thereby supporting the proposed Koch's postulate of comparative infectious disease causation.
Bartonella spp. Infection and Endocarditis
In 1993, for the first time in the medical literature, human endocarditis was associated with different Bartonella species (B. quintana, B. elizabethae and B. henselae) in three separate patients (Chomel et al., 2009b). Shortly thereafter, B. vinsonii subsp. berkhoffii became the first Bartonella spp. to be isolated from dogs with endocarditis (Kordick et al., 1996; Breitschwerdt et al., 1999). Subsequently, this subspecies was added to the list of Bartonella species that cause endocarditis in human patients (Roux et al., 2000). All known Bartonella spp. (currently at least 32 named or candidatus species) are highly fastidious bacteria, which historically has contributed to microbiological failure to isolate them by blood culture from animal or human patients with chronic bacteraemia, endocarditis or other forms of pathology. Following the initial descriptions of Bartonella spp. endocarditis, comparative infectious disease research over the ensuing two decades implicated numerous members of this genus as frequent causes of culture-negative endocarditis in both dogs and people (Avidor et al., 2004; Fenollar et al., 2005; Houpikian and Raoult, 2005; Fournier et al., 2010). As reviewed by Chomel et al. (2009b), five of the nine Bartonella species that have been associated with canine endocarditis have also been associated with human endocarditis. From a comparative microbiological perspective, many of the same Bartonella spp. cause endocarditis in both dogs and in people and from a comparative pathophysiological perspective, infection in both mammalian species preferentially involves the aortic valve, for reasons that remain unclear (MacDonald et al., 2004; Houpikian and Raoult, 2005; Henn et al., 2009; Chomel et al., 2009b; Fournier et al., 2010). Although cats are considered the primary reservoir host for B. henselae, this Bartonella species has also been implicated as a cause of aortic valve endocarditis in cats (Perez et al., 2010). Similarly, Bartonella bovis, for which cattle are the primary reservoir hosts, has been reported to cause endocarditis in older dairy cattle (Maillard et al., 2007). Pre-existing heart valve pathology, therapeutic suppression of the immune system or immune senescence with ageing appear to be common risk factors among animals and people for the development of Bartonella endocarditis (Fenollar et al., 2005; Houpikian and Raoult, 2005; Varanat et al., 2009; Henn et al., 2009; Fournier et al., 2010). In Fig. 1, endocarditis associated with B. henselae infection in a human patient is compared with the endocarditis in a dog, only in association with B. vinsonii subsp. berkhoffii infection. Thus, in the context of research observations related to endocarditis, cats, cows, dogs and human patients, when infected with a Bartonella spp., have developed a very similar life-threatening pathology involving infected heart valves. Therefore, in support of the proposed postulate of comparative infectious disease causation, infection with a Bartonella spp. has induced histologically similar pathology in four different mammalian genera.
Bartonella spp. and Chronic Intravascular Infection
Historically and excluding Carrion's disease caused by B. bacilliformis for which chronic bacteraemia has been documented in people for over 100 years, infections associated with Bartonella spp. have for the most part been relegated to three distinct medical entities: CSD, BA and endocarditis (Dehio, 2005; Varanat et al., 2009; Jenkins et al., 2012). With the exception of endocarditis, BA and PH in immunocompromised patients, Bartonella spp. bacteraemia was historically considered self-limiting and of brief duration in immunocompetent patients. Because CSD was considered self-limiting in all patients, antibiotic treatment historically has not been recommended. In contrast, chronic bacteraemia is often documented among the numerous clinically normal animal reservoir hosts that are naturally infected by a spectrum of arthropod vectors (Billeter et al., 2008). Persistent infections have been described previously in domestic and wild animal species including, but not limited to, cats, cattle, dogs and naturally- and experimentally-infected rodents (Kordick and Breitschwerdt, 1997, 1998; Cherry et al., 2009; Bai et al., 2011). With the development of novel insect cell culture-based isolation approaches (Duncan et al., 2007; Riess et al., 2008), it is increasingly clear that bacteraemia, potentially spanning decades in duration, can persist in immunocompetent people (Breitschwerdt et al., 2007, 2008, 2010b,c, 2011; Maggi et al., 2011). Among other published examples, documentation of infection with B. henselae and B. vinsonii subsp. berkhoffii in a mother, her 10-year-old son and a twin daughter who died shortly after childbirth supports both persistent infection in the mother and son and the likelihood of perinatal infection of the children (Breitschwerdt et al., 2010b). Transplacental transmission of Bartonella spp. occurs commonly in naturally- and experimentally infected rodents (Bai et al., 2011) and may be a source of transmission for other animals. Therefore, on a comparative medical basis, chronic bacteraemia appears to be another pathophysiological finding that is associated with disease causation in animals and people infected with Bartonella spp. Additionally, in the context of disease causation, the symptoms and pathology reported by chronically bacteraemic immunocompetent patients are in many instances similar to the clinical signs and pathological lesions found in dogs naturally infected with the same Bartonella species (Table 2 ). Although causation has not been validated scientifically for each of these entities (by the principles of evidence-based medicine), evolving comparative medical research observations increasingly support a primary or cofactor role for Bartonella spp. in the pathogenesis of a spectrum of chronic diseases in man and animals (Henn et al., 2005; Goodman and Breitschwerdt, 2005; Breitschwerdt et al., 2007, 2008, 2010a,b,c, 2011; Diniz et al., 2009; Maggi et al., 2011, 2012). Table 3 provides evidence of persistent intravascular infection with B. henselae in a human patient with seizures and a prior history of CSD. Table 4 provides evidence of persistent intravascular infection in a young dog infected with B. vinsonii subsp. berkhoffii. As described above, persistent bacteraemia with a spectrum of Bartonella spp. was a well-documented phenomenon in multiple, naturally infected animal species before research efforts to document persistent bacteraemia in human patients became a consideration.
Table 2.
Comparative pathological and haematological abnormalities associated with canine and human bartonellosis
| Abnormality | Dog | Man |
|---|---|---|
| PH | + | + |
| BA | + | + |
| Endocarditis | + | + |
| Myocarditis | + | + |
| Granulomatous | ||
| Lymphadenitis | + | + |
| Hepatitis | + | + |
| Panniculitis | + | + |
| Anterior uveitis | + | + |
| Encephalitis | + | + |
| Thrombocytopenia | + | + |
| Haemolytic anaemia | + | + |
Causation has not been clearly established for all of these entities in either species. Details are provided in Chomel et al., 2009a, b; Breitschwerdt et al., 2010a.
Table 3.
Serological, PCR and culture results for a 23-year-old woman with progressive neurological dysfunction, seizures and persistent B. henselae infection
| Date of sample and sample type | IFA titre |
PCR result after |
||||
|---|---|---|---|---|---|---|
| B. henselae | B. quintana | B. vinsonii subsp. berkhoffii | Direct extraction | BAPGM enrichment culture | Blood agar plate isolate | |
| 26/05/2005, blood | 256 | 128 | 256 | B. henselae (H1)∗ | – | – |
| 27/06/2005, blood | 256 | 64 | 128 | B. henselae (H1)∗ | B. henselae (H1)∗ | B. henselae (H1)∗ |
| 20/09/2005, blood | 256 | 128 | 128 | – | – | – |
| 10/02/2006, CSF | NT | NT | NT | – | B. henselae (H1)∗ | – |
| 31/08/2006, blood | 64 | 64 | 64 | – | – | – |
Data from Breitschwerdt et al., 2008. CSF, cerebrospinal fluid; IFA, indirect fluorescent antibody; BAPGM, Bartonella alpha proteobacteria growth medium.
16S-23S ITS DNA sequencing results.
Table 4.
Sequential lysis centrifugation blood culture and IFA results for a 7-month-old neutered female mixed breed dog with persistent B. vinsonii subsp. berkhoffii bacteraemia
| Date of sample | Culture results | Colony counts/ml | IFA titre |
||
|---|---|---|---|---|---|
| B. henselae | B. clarridgeiae | B. vinsonii subsp. berkhoffii | |||
| 19/11/1995 | + (Bvb) | >1000 | 128 | <16 | 512 |
| 25/02/1996 | + (Bvb) | 369 | 64 | <16 | 256 |
| 24/03/1996 | + (Bvb) | 164 | 32 | <16 | 256 |
| 21/04/1996 | + (Bvb) | 154 | 16 | <16 | 128 |
| 22/06/1996 | + (Bvb) | 357 | 16 | <16 | 128 |
| 24/08/1996 | + (Bvb) | 12 | <16 | <16 | 64 |
| 21/10/1996 | – | 0 | <16 | <16 | 64 |
| 18/12/1996 | + (Bvb) | 6 | 16 | <16 | 64 |
| 30/01/1997∗ | + (Bvb) | 1 | 16 | <16 | 64 |
| 21/03/1997 | – | 0 | 16 | <16 | 32 |
Data from Kordick and Breitschwerdt (1998). Bvb, B. vinsonii subsp. berkhoffii; IFA, indirect fluorescent antibody.
After collection of blood for culture, the dog received doxycycline hyclate for 28 days.
Concluding Remarks
It is very clear that the original and the more recently proposed molecular Koch's postulates have been historically useful, particularly when attempting to confirm that a disease is caused by a single infectious agent that induces an acute versus a chronic infection. Causation is established more readily when an organism has a brief incubation period, when there is a readily defined source of exposure and when the pathogen induces an acute illness (microbiological features of frontal pathogens). Unfortunately, as was acknowledged by Koch and others, application of the original four postulates has serious limitations when attempting to attribute disease causation to stealth pathogens that can induce chronic, slowly progressive disease manifestations in an animal or human patient. In addition, Koch's postulates do not allow researchers to readily address naturally occurring environmental, nutritional, genetic and other medically relevant factors that influence disease causation and do not consider the pathogenic complexities induced by sequential or simultaneous infection with more than one pathogenic microorganism. As approximately 70% of emerging infectious diseases are zoonotic in nature (Taylor et al., 2001), understanding the comparative biological and pathological behaviour of a specific infectious agent across different animal hosts, particularly human patients, pet cats and dogs that share the same environment, might provide useful indicators of chronic disease causation (Day et al., 2012). This is an important concept with respect to the mounting importance of the global ‘One Health’ paradigm that proposes much closer integration of human and veterinary medicine (Jones et al., 2008; People, Pathogens and Our Planet Volume 1, 2010). It is essential that cross-species infectious agents are investigated in a collaborative fashion by integrated teams of medical, veterinary medical and other public health officials and that appropriate resources are allocated to permit this approach to be successful. Although the present review is focused on organisms of the genus Bartonella, there are numerous other frontal pathogens (e.g. influenza virus, methicillin-resistant Staphylococcus aureus, SARS coronavirus and monkey pox) and stealth pathogens (e.g. Anaplasma phagocytophilum, Borrelia burgdorferi, Coxiella burnetii, Ehrlichia spp. and Toxoplasma gondii), shared between man and small companion animals, for which a co-ordinated One Health approach to investigation and application of our proposed Koch's postulate of comparative disease causation would be of benefit to animal and human health.
In conclusion, we propose the addition of a fifth Koch's postulate to address comparative disease causation where the same infectious agent is isolated or DNA sequences are found in at least three mammalian genera. In the examples provided in this manuscript, this postulate has been achieved for Bartonella spp. and vasoproliferative lesions in cats, dogs, a horse, people and a steer, granulomatous inflammatory lesions in cats, dogs and human patients, endocarditis in cats, cows, dogs and human patients and chronic bacteraemia in cats, dogs, people and numerous rodent species. The authors hope that the postulate of ‘comparative infectious disease causation’ can be used by other infectious disease researchers to assist with efforts to define the role of specific or co-infecting infectious agents in patients with chronic, complex disease expression.
Conflict of Interest Statement
In conjunction with Dr. S. Sontakke and North Carolina State University, Dr. Breitschwerdt holds US Patent No. 7,115,385; Media and Methods for cultivation of microorganisms, which was issued October 3, 2006. He is the chief scientific officer for Galaxy Diagnostics, a newly formed company that provides diagnostic testing for the detection of Bartonella spp. infection in animals and in human patient samples. Dr. R. Maggi has led efforts to optimize the BAPGM platform and is the Scientific Technical Adviser and Laboratory Director for Galaxy Diagnostics. All other authors report no conflicts of interest.
References
- Albrich W.C., Kraft C., Fisk T., Albrecht H. A mechanic with a bad valve: blood-culture-negative endocarditis. Lancet Infectious Diseases. 2004;4:777–784. doi: 10.1016/S1473-3099(04)01226-5. [DOI] [PubMed] [Google Scholar]
- Angelakis E., Lepidi H., Canel A., Rispal P., Perraudeau F. Human case of Bartonella alsatica lymphadenitis. Emerging Infectious Diseases. 2008;14:1951–1953. doi: 10.3201/eid1412.080757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avidor B., Graidy M., Efrat G., Leibowitz C., Shapira G. Bartonella koehlerae, a new cat-associated agent of culture-negative human endocarditis. Journal of Clinical Microbiology. 2004;42:3462–3468. doi: 10.1128/JCM.42.8.3462-3468.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai Y., Calisher C.H., Kosoy M.Y., Root J.J., Doty J.B. Persistent infection or successive reinfection of deer mice with Bartonella vinsonii subsp. arupensis. Applied and Environmental Microbiology. 2011;77:1728–1731. doi: 10.1128/AEM.02203-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beerlage C., O’Rourke F., Kempf V.A.J. Bartonella henselae verbindet Infektionsforschung mit Blutgefäßwachstum. Forschung Frankfurt. 2011;2:26–29. [Google Scholar]
- Beerlage C., Varanat M., Linder K., Maggi R.G., Colley J. Bartonella vinsonii subsp. berkhofffii and Bartonella henselae as potential causes of proliferative vascular disease in animals. Medical Microbiology and Immunology. 2012;201:319–326. doi: 10.1007/s00430-012-0234-5. [DOI] [PubMed] [Google Scholar]
- Berrich M., Kieda C., Grillon C., Monteil M., Lamerant N. Differential effects of Bartonella henselae on human and feline macro- and micro-vascular endothelial cells. PLoS One. 2011;6:e20204. doi: 10.1371/journal.pone.0020204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billeter S.A., Levy M.G., Chomel B.B., Breitschwerdt E.B. Vector transmission of Bartonella species with emphasis on the potential for tick transmission. Medical and Veterinary Entomology. 2008;22:1–15. doi: 10.1111/j.1365-2915.2008.00713.x. [DOI] [PubMed] [Google Scholar]
- Breitschwerdt E.B., Atkins C.E., Brown T.T., Kordick D.L., Snyder P.S. Bartonella vinsonii subsp. berkhoffii and related members of the alpha subdivision of the Proteobacteria in dogs with cardiac arrhythmias, endocarditis, or myocarditis. Journal of Clinical Microbiology. 1999;37:3618–3626. doi: 10.1128/jcm.37.11.3618-3626.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitschwerdt E.B., Kordick D.L., Malarkey D.E., Keene B., Hadfield T.L. Endocarditis in a dog due to infection with a novel Bartonella subspecies. Journal of Clinical Microbiology. 1995;33:154–160. doi: 10.1128/jcm.33.1.154-160.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitschwerdt E.B., Maggi R.G., Chomel B.B., Lappin M.R. Bartonellosis: an emerging infectious disease of zoonotic importance to animals and human beings. Journal of Veterinary Emergency and Critical Care. 2010;20:8–30. doi: 10.1111/j.1476-4431.2009.00496.x. [DOI] [PubMed] [Google Scholar]
- Breitschwerdt E.B., Maggi R.G., Duncan A.W., Nicholson W.L., Hegarty B.C. Bartonella species in blood of immunocompetent persons with animal and arthropod contact. Emerging Infectious Diseases. 2007;13:938–941. doi: 10.3201/eid1306.061337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitschwerdt E.B., Maggi R.G., Farmer P., Mascarelli P.E. Molecular evidence of perinatal transmission of Bartonella vinsonii subsp. berkhoffii and Bartonella henselae to a child. Journal of Clinical Microbiology. 2010;48:2289–2293. doi: 10.1128/JCM.00326-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitschwerdt E.B., Maggi R.G., Lantos P.M., Woods C.W., Hegarty B.C. Bartonella vinsonii subsp. berkhoffii and Bartonella henselae bacteremia in a father and daughter with neurological disease. Parasites and Vectors. 2010;3:29–37. doi: 10.1186/1756-3305-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitschwerdt E.B., Maggi R.G., Nicholson W.L., Cherry N.A., Woods C.W. Bartonella sp. bacteremia in patients with neurological and neurocognitive dysfunction. Journal of Clinical Microbiology. 2008;46:2856–2861. doi: 10.1128/JCM.00832-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitschwerdt E.B., Maggi R.G., Varanat M., Linder K.E., Weinberg G. Isolation of Bartonella vinsonii subsp. berkhoffii genotype II from a boy with epithelioid hemangioendothelioma and a dog with hemangiopericytoma. Journal of Clinical Microbiology. 2009;47:1957–1960. doi: 10.1128/JCM.00069-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitschwerdt E.B., Mascarelli P.E., Schweickert L.A., Maggi R.G., Hegarty B.C. Hallucinations, sensory neuropathy, and peripheral visual deficits in a young woman infected with Bartonella koehlerae. Journal of Clinical Microbiology. 2011;49:3415–3417. doi: 10.1128/JCM.00833-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breshears M.A., Johnson B.J. Systemic reactive angioendotheliomatosis-like syndrome in a steer presumed to be persistently infected with bovine viral diarrhea virus. Veterinary Pathology. 2008;45:645–649. doi: 10.1354/vp.45-5-645. [DOI] [PubMed] [Google Scholar]
- Cherry N.A., Maggi R.G., Cannedy A.L., Breitschwerdt E.B. PCR detection of Bartonella bovis and Bartonella henselae in the blood of beef cattle. Veterinary Microbiology. 2009;135:308–312. doi: 10.1016/j.vetmic.2008.09.063. [DOI] [PubMed] [Google Scholar]
- Chomel B.B., Boulouis H.J., Breitschwerdt E.B., Kasten R.W., Vayssier-Taussat M. Ecological fitness and strategies of adaptation of Bartonella species to their hosts and vectors. Veterinary Research. 2009;40:29. doi: 10.1051/vetres/2009011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chomel B.B., Kasten R.W., Williams C., Wey A.C., Henn J.B. Bartonella endocarditis: a pathology shared by animal reservoirs and patients. Annals of the New York Academy of Sciences. 2009;1166:120–126. doi: 10.1111/j.1749-6632.2009.04523.x. [DOI] [PubMed] [Google Scholar]
- Cross J.R., Rossmeisl J.H., Maggi R.G., Breitschwerdt E.B., Duncan R.B. Bartonella-associated meningoradiculoneuritis and dermatitis or panniculitis in 3 dogs. Journal of Veterinary Internal Medicine. 2008;22:674–678. doi: 10.1111/j.1939-1676.2008.0087.x. [DOI] [PubMed] [Google Scholar]
- Day M.J., Breitschwerdt E.B., Cleaveland S., Karkare U., Khanna C. Surveillance of zoonotic infectious disease transmitted by small companion animals. Emerging Infectious Diseases. 2012 2012 Dec [date cited] [Google Scholar]
- Dehio C. Bartonella – host cell interactions and vascular tumor formation. Nature Reviews Microbiology. 2005;3:621–631. doi: 10.1038/nrmicro1209. [DOI] [PubMed] [Google Scholar]
- Diniz P.P., Wood M., Maggi R.G., Sontakke S., Stepnik M. Co-isolation of Bartonella henselae and Bartonella vinsonii subsp. berkhoffii from blood, joint and subcutaneous seroma fluids from two naturally infected dogs. Veterinary Microbiology. 2009;138:368–372. doi: 10.1016/j.vetmic.2009.01.038. [DOI] [PubMed] [Google Scholar]
- Duncan A.W., Maggi R.G., Breitschwerdt E.B. A combined approach for the enhanced detection and isolation of Bartonella species in dog blood samples: pre-enrichment liquid culture followed by PCR and subculture onto agar plates. Journal of Microbiological Methods. 2007;69:273–281. doi: 10.1016/j.mimet.2007.01.010. [DOI] [PubMed] [Google Scholar]
- Emamaullee J.A., Edgar R., Toso C., Thiesen A., Bain V. Vascular endothelial growth factor expression in hepatic epithelioid hemangioendothelioma: implications for treatment and surgical management. Liver Transplantation. 2010;16:191–197. doi: 10.1002/lt.21964. [DOI] [PubMed] [Google Scholar]
- Falkow S. Molecular Koch's postulates applied to microbial pathogenicity. Reviews of Infectious Diseases. 1988;10(Suppl. 2):S274–S276. doi: 10.1093/cid/10.supplement_2.s274. [DOI] [PubMed] [Google Scholar]
- Falkow S. Molecular Koch's postulates applied to bacterial pathogenicity – a personal recollection 15 years later. Nature Reviews Microbiology. 2004;2:67–72. doi: 10.1038/nrmicro799. [DOI] [PubMed] [Google Scholar]
- Fenollar F., Sire S., Raoult D. Bartonella vinsonii subsp. arupensis as an agent of blood culture-negative endocarditis in a human. Journal of Clinical Microbiology. 2005;43:945–947. doi: 10.1128/JCM.43.2.945-947.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier P.E., Thuny F., Richet H., Lepidi H., Casalta J.P. Comprehensive diagnostic strategy for blood culture-negative endocarditis: a prospective study of 819 new cases. Clinical Infectious Diseases. 2010;51:131–140. doi: 10.1086/653675. [DOI] [PubMed] [Google Scholar]
- Fredericks D.N., Relman D.A. Sequence-based identification of microbial pathogens: a reconsideration of Koch's postulates. Clinical Microbiology Reviews. 1996;9:18–33. doi: 10.1128/cmr.9.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuji R.N., Patton K.M., Steinbach T.J., Schulman F.Y., Bradley G.A. Feline systemic reactive angioendotheliomatosis: eight cases and literature review. Veterinary Pathology. 2005;42:608–617. doi: 10.1354/vp.42-5-608. [DOI] [PubMed] [Google Scholar]
- Gerber J.E., Johnson J.E., Scott M.A., Madhusudhan K.T. Fatal meningitis and encephalitis due to Bartonella henselae bacteria. Journal of Forensic Sciences. 2002;47:640–664. [PubMed] [Google Scholar]
- Giladi M., Maman E., Paran D., Bickels J., Comaneshter D. Cat-scratch disease-associated arthropathy. Arthritis and Rheumatism. 2005;52:3611–3617. doi: 10.1002/art.21411. [DOI] [PubMed] [Google Scholar]
- Gillespie T.N., Washabau R.J., Goldschmidt M.H., Cullen J.M., Rogala A.R. Detection of Bartonella henselae and Bartonella clarridgeiae DNA in hepatic specimens from two dogs with hepatic disease. Journal of the American Veterinary Medical Association. 2003;222:47–51. doi: 10.2460/javma.2003.222.47. [DOI] [PubMed] [Google Scholar]
- Goodman R.A., Breitschwerdt E.B. Clinicopathologic findings in dogs seroreactive to Bartonella henselae antigens. American Journal of Veterinary Research. 2005;66:2060–2064. doi: 10.2460/ajvr.2005.66.2060. [DOI] [PubMed] [Google Scholar]
- Hatva E., Böhling T., Jääskeläinen J., Persico M.G., Haltia M. Vascular growth factors and receptors in capillary hemangioblastomas and hemangiopericytomas. American Journal of Pathology. 1996;148:763–775. [PMC free article] [PubMed] [Google Scholar]
- Henn J.B., Gabriel M.W., Kasten R.W., Brown R.N., Koehler J.E. Infective endocarditis in a dog and the phylogenetic relationship of the associated ‘Bartonella rochalimae’ strain with isolates from dogs, gray foxes, and a human. Journal of Clinical Microbiology. 2009;47:787–790. doi: 10.1128/JCM.01351-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henn J.B., Liu C.H., Kasten R.W., VanHorn B.A., Beckett L.A. Seroprevalence of antibodies against Bartonella species and evaluation of risk factors and clinical signs associated with seropositivity in dogs. American Journal of Veterinary Research. 2005;66:688–694. doi: 10.2460/ajvr.2005.66.688. [DOI] [PubMed] [Google Scholar]
- Houpikian P., Raoult D. Blood culture-negative endocarditis in a reference center: etiologic diagnosis of 348 cases. Medicine (Baltimore) 2005;84:162–173. doi: 10.1097/01.md.0000165658.82869.17. [DOI] [PubMed] [Google Scholar]
- Jacomo V., Kelly P.J., Raoult D. Natural history of Bartonella infections (an exception to Koch's postulate) Clinical and Diagnostic Laboratory Immunology. 2002;9:8–18. doi: 10.1128/CDLI.9.1.8-18.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins M., Chiriva-Internati M., Mirandola L., Tonroy C., Tedjarati S.S. Perspective for prophylaxis and treatment of cervical cancer: an immunological approach. International Reviews of Immunology. 2012;31:3–21. doi: 10.3109/08830185.2011.637254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones K.E., Patel N.G., Levy M.A., Storeygard A., Balk D. Global trends in emerging infectious diseases. Nature. 2008;451:990–994. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempf V.A., Lebiedziejewski M., Alitalo K., Wälzlein J.H., Ehehalt U. Activation of hypoxia-inducible factor-1 in bacillary angiomatosis: evidence for a role of hypoxia-inducible factor-1 in bacterial infections. Circulation. 2005;111:1054–1062. doi: 10.1161/01.CIR.0000155608.07691.B7. [DOI] [PubMed] [Google Scholar]
- Kempf V.A., Petzold H., Autenrieth I.B. Cat scratch disease due to Bartonella henselae infection mimicking parotid malignancy. European Journal of Clinical Microbiology and Infectious Diseases. 2001;20:732–733. doi: 10.1007/s100960100605. [DOI] [PubMed] [Google Scholar]
- Kempf V.A., Volkmann B., Schaller M., Sander C.A., Alitalo K. Evidence of a leading role for VEGF in Bartonella henselae-induced endothelial cell proliferations. Cellular Microbiology. 2001;3:623–632. doi: 10.1046/j.1462-5822.2001.00144.x. [DOI] [PubMed] [Google Scholar]
- Kitchell B.E., Fan T.M., Kordick D., Breitschwerdt E.B., Wollenberg G. Peliosis hepatis in a dog infected with Bartonella henselae. Journal of the American Veterinary Medical Association. 2000;216:519–523. doi: 10.2460/javma.2000.216.519. [DOI] [PubMed] [Google Scholar]
- Koehler J.E., Sanchez M.A., Garrido C.S., Whitfeld M.J., Chen F.M. Molecular epidemiology of Bartonella infections in patients with bacillary angiomatosis-peliosis. New England Journal of Medicine. 1997;337:1876–1883. doi: 10.1056/NEJM199712253372603. [DOI] [PubMed] [Google Scholar]
- Koehler J.E., Tappero J.W. Bacillary angiomatosis and bacillary peliosis in patients infected with human immunodeficiency virus. Clinical Infectious Diseases. 1993;17:612–624. doi: 10.1093/clinids/17.4.612. [DOI] [PubMed] [Google Scholar]
- Kordick D.L., Breitschwerdt E.B. Relapsing bacteremia following blood transmission of Bartonella henselae in cats. American Journal of Veterinary Research. 1997;58:492–497. [PubMed] [Google Scholar]
- Kordick D.L., Breitschwerdt E.B. Persistent infection of pets within a household with three Bartonella species. Emerging Infectious Diseases. 1998;4:325–328. doi: 10.3201/eid0402.980225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kordick D.L., Swaminathan B., Greene C.E., Wilson K.H., Whitney A.M. Bartonella vinsonii subsp. berkhoffii subsp. nov., isolated from dogs; Bartonella vinsonii subsp. vinsonii; and amended description of Bartonella vinsonii. International Journal of Systemic Bacteriology. 1996;46:704–709. doi: 10.1099/00207713-46-3-704. [DOI] [PubMed] [Google Scholar]
- Loeffler F. Mitt. Aus dem Kaiserl. Gesundheitsamte. 1884;2:421–499. [Google Scholar]
- MacDonald K.A., Chomel B.B., Kittleson M.D., Kasten R.W., Thomas W.P. A prospective study of canine infective endocarditis in northern California (1999-2001): emergence of Bartonella as a prevalent etiologic agent. Journal of Veterinary Internal Medicine. 2004;18:56–64. doi: 10.1892/0891-6640(2004)18<56:apsoci>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Maggi R.G., Mascarelli P.E., Pultorak E.L., Hegarty B.C., Bradley J.M. Bartonella spp. bacteremia in high-risk immunocompetent patients. Diagnostic Microbiology and Infectious Disease. 2011;71:430–437. doi: 10.1016/j.diagmicrobio.2011.09.001. [DOI] [PubMed] [Google Scholar]
- Maggi R.G., Mozayeni R.B., Hegarty B.C., Bradley J.M., Breitschwerdt E.B. Bartonella spp. bacteremia in rheumatic patients from Lyme disease-endemic region. Emerging Infectious Diseases. 2012;18:783–791. doi: 10.3201/eid1805.111366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maillard R., Petit E., Chomel B., Lacroux C., Schelcher F. Endocarditis in cattle caused by Bartonella bovis. Emerging Infectious Diseases. 2007;13:1383–1385. doi: 10.3201/eid1309.070236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mascarelli P.E., Iredell J.R., Maggi R.G., Weinberg G., Breitschwerdt E.B. Bartonella species bacteremia in two patients with epithelioid hemangioendothelioma. Journal of Clinical Microbiology. 2011;49:4006–4012. doi: 10.1128/JCM.05527-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellor P.J., Fetz K., Maggi R.G., Haugland S., Dunning M. Alpha1-proteinase inhibitor deficiency and Bartonella infection in association with panniculitis, polyarthritis, and meningitis in a dog. Journal of Veterinary Internal Medicine. 2006;20:1023–1028. doi: 10.1892/0891-6640(2006)20[1023:aidabi]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Merrell D.S., Falkow S. Frontal and stealth attack strategies in microbial pathogenesis. Nature. 2004;430:250–256. doi: 10.1038/nature02760. [DOI] [PubMed] [Google Scholar]
- Pappalardo B.L., Brown T., Gookin J.L., Morrill C.L., Breitschwerdt E.B. Granulomatous disease associated with Bartonella infection in 2 dogs. Journal of Veterinary Internal Medicine. 2000;14:37–42. doi: 10.1892/0891-6640(2000)014<0037:gdawii>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- People, Pathogens and Our Planet. Vol. 1 . International Bank for Reconstruction and Development/World Bank; 1818 H Street NW, Washington DC: 2010. Towards a One Health Approach to Controlling Zoonotic Disease. World Bank Report 50833-GLB. p. 20433. [Google Scholar]
- Perez C., Hummel J.B., Keene B.W., Maggi R.G., Diniz P.P. Successful treatment of Bartonella henselae endocarditis in a cat. Journal of Feline Medicine and Surgery. 2010;12:483–486. doi: 10.1016/j.jfms.2009.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psarros G., Riddell J., 4th, Gandhi T., Kauffman C.A., Cinti S.K. Bartonella henselae infections in solid organ transplant recipients: report of 5 cases and review of the literature. Medicine (Baltimore) 2012;91:111–121. doi: 10.1097/MD.0b013e31824dc07a. [DOI] [PubMed] [Google Scholar]
- Resto-Ruiz S.I., Schmiederer M., Sweger D., Newton C., Klein T.W. Induction of a potential paracrine angiogenic loop between human THP-1 macrophages and human microvascular endothelial cells during Bartonella henselae infection. Infection and Immunity. 2002;70:4564–4570. doi: 10.1128/IAI.70.8.4564-4570.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riess T., Dietrich F., Schmidt K.V., Kaiser P.O., Schwarz H. Analysis of a novel insect cell culture medium-based growth medium for Bartonella species. Applied and Environmental Microbiology. 2008;74:5224–5227. doi: 10.1128/AEM.00621-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux V., Eykyn S.J., Wyllie S., Raoult D. Bartonella vinsonii subsp. berkhoffii as an agent of afebrile blood culture-negative endocarditis in a human. Journal of Clinical Microbiology. 2000;38:1698–1700. doi: 10.1128/jcm.38.4.1698-1700.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabrah F.L. Koch's postulates, carnivorous cows, and tuberculosis today. Hawaii Medical Journal. 2011;70:144–148. [PMC free article] [PubMed] [Google Scholar]
- Taylor L.H., Latham S.M., Woolhouse M.E. Risk factors for human disease emergence. Philosophical Transactions of the Royal Society of London. 2001;356:983–989. doi: 10.1098/rstb.2001.0888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderHeyden T.R., Yong S.L., Breitschwerdt E.B., Maggi R.G., Mihalik A.R. Granulomatous hepatitis due to Bartonella henselae infection in an immunocompetent patient. BMC Infectious Diseases. 2012;12:17. doi: 10.1186/1471-2334-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varanat M., Maggi R.G., Linder K.E., Breitschwerdt E.B. Molecular prevalence of Bartonella, Babesia and hemotropic Mycoplasma sp. in dogs with splenic disease. Journal of Veterinary Internal Medicine. 2011;25:1284–1291. doi: 10.1111/j.1939-1676.2011.00811.x. [DOI] [PubMed] [Google Scholar]
- Varanat M., Travis A., Lee W., Maggi R.G., Bissett S.A. Recurrent osteomyelitis in a cat due to infection with Bartonella vinsonii subsp. berkhoffii genotype II. Journal of Veterinary Internal Medicine. 2009;23:1273–1277. doi: 10.1111/j.1939-1676.2009.0372.x. [DOI] [PubMed] [Google Scholar]
- Yager J.A., Best S.J., Maggi R.G., Varanat M., Znajda N. Bacillary angiomatosis in an immunosuppressed dog. Veterinary Dermatology. 2010;21:420–428. doi: 10.1111/j.1365-3164.2010.00879.x. [DOI] [PubMed] [Google Scholar]
- Yonemaru K., Sakai H., Murakami M., Yanai T., Masegi T. Expression of vascular endothelial growth factor, basic fibroblast growth factor, and their receptors (flt-1, flk-1, and flg-1) in canine vascular tumors. Veterinary Pathology. 2006;43:971–980. doi: 10.1354/vp.43-6-971. [DOI] [PubMed] [Google Scholar]