Objective
Mortality by coronavirus disease 2019 (COVID-19) is lower in women than in men.1 Mortality pertains mostly to aging, in which a protective effect of ovarian hormones is difficult to envision. However, speculation on the possible protective effect of estrogens is being formulated. Currently, the epidemiologic evidence does not clearly indicate whether mortality of individuals with COVID-19 is affected differently between sexes with age. In this study, we investigated whether mortality is affected differently between sexes with age.
Study Design
On April 19, 2020, the Italian National Institute of Health (ISS) published data on infection and death by COVID-19 that occurred in Italy in 2 months, from Feb. 22, 2020 (infection outbreak), to April 19, 2020.2 Data divided by sex and age categories of 10 years were based on swab test results, positive for severe acute respiratory syndrome coronavirus and analyzed by ISS-accredited laboratories, and death certificates. Infections and deaths of individuals aged 10 to 89 years were retrieved.2 Death rate (deaths/100 infected) was calculated separately for each sex and age category. Death rate (deaths/100 individuals) unrelated to COVID-19 was obtained, stratified by age and sex, from the Istituto Nazionale di Statistica (Italian National Statistics Institute) database in the year 2018.3 The data of the entire year were adapted to a period of 2 months. To obtain the estimated excess death rate caused by COVID-19, the death rate was subtracted from that observed in the cohort of individuals with COVID-19. Excess death rate was then stratified by sex and age in categories of 10 years. To evaluate whether the difference of excess death rate (deaths/infected) caused by COVID-19 between men and women remained constant across age, for any age category, the ratio of death rate of women and death rate of men was calculated and expressed in percentage.
Results
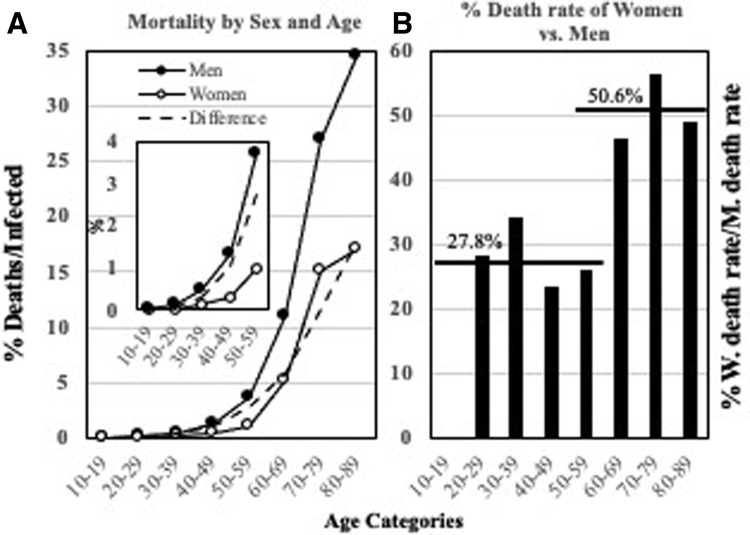
In the ISS report, there were 147,706 affected individuals of whom 17,520 died during the 2 months (death rate of 11.8%). In the same period, death rate of noninfected individuals was 1.00%. As a result, excess death rate caused by COVID-19 was estimated to be 10.8%. Excess death rate increased with age and was always lower in women than in men (Figure , A). An excess death rate by COVID-19 higher than 1% was observed after 50 to 59 years of age in women and after 30 to 39 years of age in men (Figure, A). The difference in excess death rate by COVID-19 between women and men changed with age. By considering men’s death rate equal to 100%, women’s death rate was only 27.8% (−72.2%) in ages 20 to 59 years and 50.6% (−49.4%) in ages 60 to 89 years (Figure, B).
Figure.
Excess death rate by COVID-19 of men and women of different ages
A, Excess death rate by COVID-19 of men and women stratified by age. The insert refers only to the age categories of 50 to 59 years. The interrupted line indicates the difference in death rate between men and women in each age category. B, Percentages of COVID-19–related death rate of women (W) vs men (M) (deaths in 100 infected women/deaths in 100 infected men×100) for each age category. Sample sizes of the age categories were as follows: 10 to 19 years, n=1798; 20 to 29 years, n=7688; 30 to 39 years, n=11,643; 40 to 49 years, n=20,519; 50 to 59 years, n=29,794; 60 to 69 years, n=23,987; 70 to 79 years, n=25,674; 80 to 89 years, n=26,661.
COVID-19, coronavirus disease 2019.
Cagnacci. Age-related difference in the rate of coronavirus disease 2019 mortality in women versus men. Am J Obstet Gynecol 2020.
Conclusion
Excess death rate by COVID-19 is lower in women than in men. Lifestyle, rate of smoking, or other risk factors may be different between men and women. However, these data were not available, and we could not control for these factors. Nevertheless, we controlled for natural mortality, which should integrate differences in risk factors between the 2 sexes. Genes are also different between men and women. All these factors may explain the different rate of COVID-19–related mortality between sexes but are unlikely to explain the reason the difference of death rate between sexes changed abruptly and constantly after 50 to 59 years of age. The endocrine milieu is different between men and women. In women, ovarian hormones influence inflammation, immunity, and the expression of angiotensin-converting enzyme 24 that seems to play a role in determining COVID-19 progression.1 These effects are lost after menopause, which occurs in Italian women at median age of 50 years (range, 30–61 years).5 However, we could not perform a more specific calculation such as grouping women with and without menopause, but existing results may prompt further analyses on this issue.
Footnotes
The authors report no conflict of interest.
This communication has been published in the middle of the COVID-19 pandemic and is available via expedited publication to assist patients and healthcare providers.
References
- 1.Cheng H., Wang Y., Wang G.Q. Organ-protective effect of angiotensin-converting enzyme 2 and its effect on the prognosis of COVID-19. J Med Virol. 2020 doi: 10.1002/jmv.25785. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Italian National Institute of Health (ISS) Epidemia COVID-19. https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_16-aprile-2020.pdf Available at:
- 3.ISTAT. Available at: demo.istat.it/tvm2018/index.php?lingua=ita. Accessed April 12, 2020.
- 4.Bukowska A., Spiller L., Wolke C., et al. Protective regulation of the ACE2/ACE gene expression by estrogen in human atrial tissue from elderly men. Exp Biol Med (Maywood) 2017;242:1412–1423. doi: 10.1177/1535370217718808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cagnacci A., Pansini F.S., Bacchi–Modena A., et al. Season of birth influences the timing of menopause. Hum Reprod. 2005;20:2190–2193. doi: 10.1093/humrep/dei040. [DOI] [PubMed] [Google Scholar]